Neurogenic stunned myocardium (NSM) is a clinical-pathological entity that presents with myocardial injury and dysfunction occurring after diverse types of acute brain injury; it results from imbalance of the autonomic nervous system1 which is typically secondary to subarachnoid haemorrhage. However, NSM may also be related to other central nervous system disorders associated with brain injuries, such as ischaemic strokes, trauma, hydrocephalus, and epileptic seizures. Several theories attempt to explain the pathophysiological mechanism of NSM, but the most widely accepted theory implicates a flood of catecholamines released by the central nervous system. These catecholamines cause systemic myocardial injury, which is characterised by pathological findings of contraction band necrosis with normal coronary perfusion.2–5 Electrocardiogram shows QT prolongation, deep symmetrical T-wave inversions, and ST slurring. It also displays a depressed ejection fraction of less than 40%.6
We present the case of a patient with chronic hydrocephalus due to idiopathic stenosis of the aqueduct of Sylvius, with onset of NSM after an endoscopic third ventriculostomy.
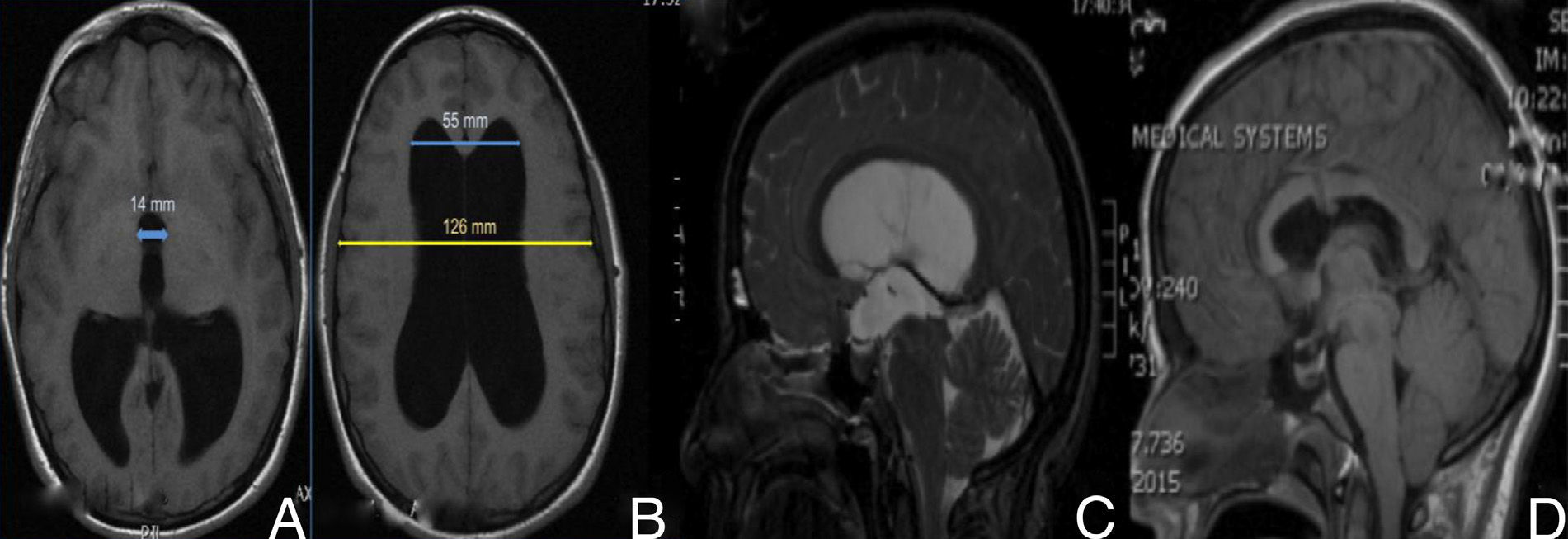
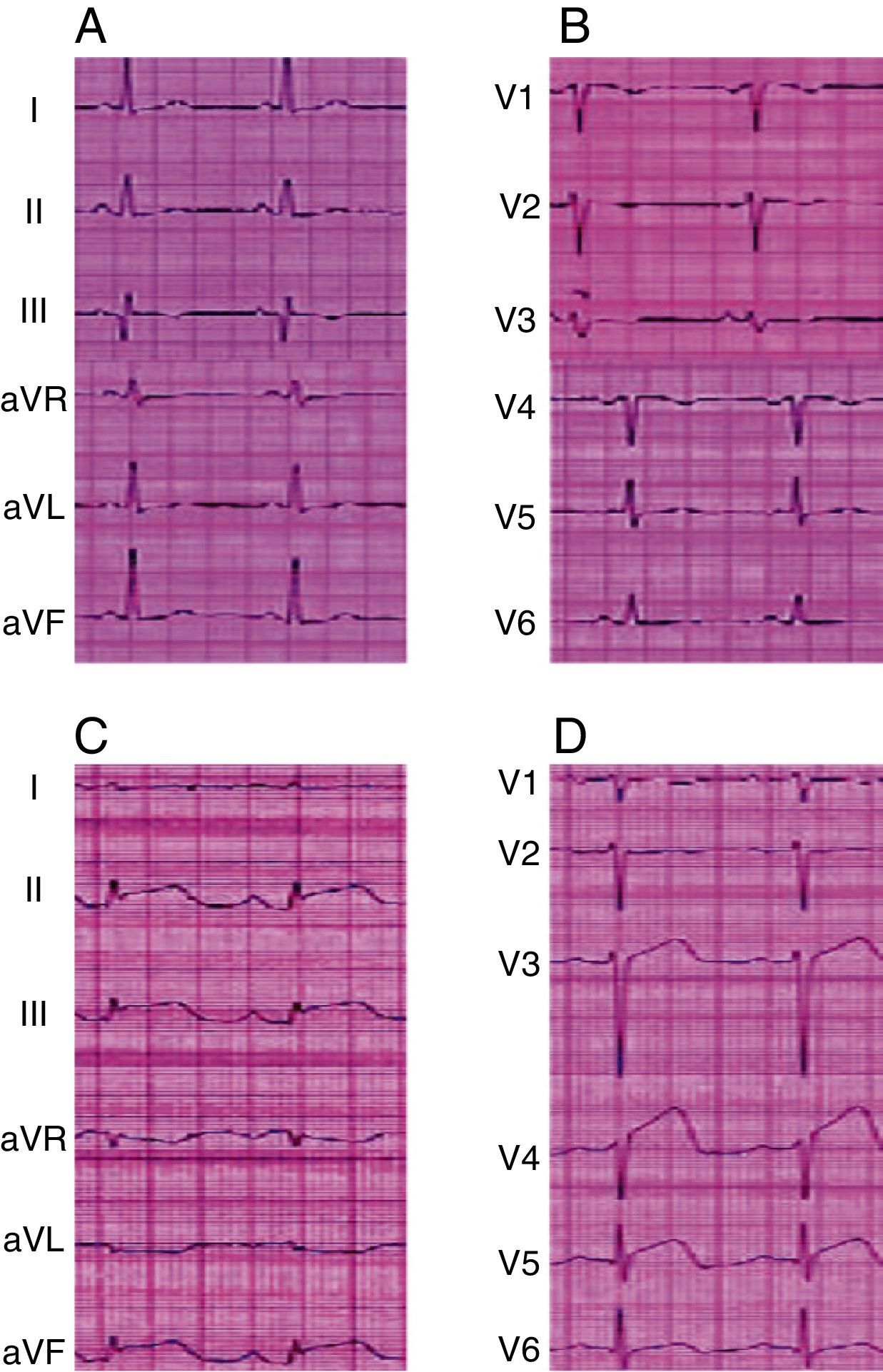
Our patient is a 35-year-old woman admitted to the neurosurgery department for scheduled surgical treatment of chronic hydrocephalus secondary to idiopathic stenosis of the aqueduct of Sylvius. In the preceding 10 months, she had experienced increased frontal headache and fluctuating memory changes. Findings from the neurological exam were limited to slightly diminished visual acuity. Magnetic resonance imaging (MRI) showed triventricular hydrocephalus (Fig. 1A–C). Presurgical cardiological evaluation revealed no cardiac changes (Fig. 2A and B). Presurgical blood pressure was 126/84mmHg. With the patient's informed consent, we proceeded to perform an endoscopic third ventriculostomy and found no elevated intracranial pressure. The external ventricular drain was placed on the right lateral ventricle. Nine hours after the surgery, while the patient's status was good, she began to develop symptoms of sudden-onset headache and progressive decrease in level of consciousness, with subsequent decerebrate rigidity, right-sided mydriasis, intracranial hypertension, altered heart rate, and arterial hypotension. The patient was intubated and transferred in coma to the intensive care unit. A transthoracic echocardiogram showed dilated left ventricle with akinesia of the lower interventricular septum, lateral and posterior hypokinesia, and an ejection fraction of 38%. Electrocardiogram revealed widened QRS complex, inverted T wave, and ST segment elevation (Fig. 2C and D). Levels of cardiac enzymes were high. Initial brain computed tomography revealed diffuse subarachnoid haemorrhage (Fig. 3). Three days after onset of coma, we performed an electroencephalogram that showed no brain activity. Our patient died 5 days later due to acute heart failure. We were unable to perform an autopsy because the patient's family did not give consent.
Presurgical imaging studies (A and B): T1-weighted brain MRI without contrast that revealed triventricular hydrocephalus. Evans index was 0.43 (B) and third ventricle diameter was >1.4cm (A). Presurgical study (C): T2-weighted MRI showing increased convexity of the corpus callosum, flattening of the midbrain, and stenosis of the aqueduct of Sylvius. Postsurgical studies (D): T1-weighted MRI without contrast that revealed decreased ventricular size, upward displacement of midbrain, and the endoscope path for the third ventriculostomy.
NSM is usually secondary to acute neurological damage that activates the sympathetic nervous system, causing a catecholaminergic storm. In fact, previous studies have established an association between subarachnoid haemorrhage and hypothalamic disturbances as precipitants of cardiac hyperexcitability and secondary myocardial damage.7,8 These entities have also been causally linked to other brain injuries such as head trauma, acute hydrocephalus, etc.7,9
In our case, the patient displayed heart symptoms a few hours after the endoscopic third ventriculostomy and external ventricular drain placement were performed. On this basis, we might conclude that stunned myocardium could have been secondary to hypothalamic stimulation during surgery. Another possible explanation might be subarachnoid haemorrhage after the intervention. Diffuse cerebral oedema could also have been due to a significant decrease in brain perfusion during the period in which ejection fraction was below 40%.7,10,11 Pulmonary oedema, also called neurogenic pulmonary oedema, is a widely studied entity.12 It is believed to be secondary to sympathetic hyperactivity, although this condition is not always present in stunned myocardium.
Although intraventricular hydrocephalus due to stenosis of the aqueduct of Sylvius generally manifests in childhood, its first clinical signs may not appear until adulthood in some cases. The precise pathophysiological mechanism explaining delayed manifestation is still unknown. However, idiopathic stenosis of the aqueduct of Sylvius could be due to a congenital anomaly in the development of the aqueduct of Sylvius, or to aqueductal gliosis. Several cases of chronic hydrocephalus due to idiopathic stenosis of the aqueduct of Sylvius in adults have been described in the literature.13,14
The most common symptom is headache, but that symptom is not necessarily progressive. Treatment of choice for hydrocephalus due to aqueductal stenosis is usually endoscopic third ventriculostomy, in both children and adults.13
Cases described in the literature do not normally present fulminant progression. In fact, cardiac enzyme levels generally improve in a period of several hours to a few days, after which patients recover. We cannot explain why our patient displayed non-reactive right-sided mydriasis and decerebrate rigidity as initial signs.
Please cite this article as: Piña Batista KM, Gutiérrez Morales JC, Astudillo A, Alvarez de Eulate-Beramendi S. Síndrome de corazón contundido fulminante tras ventriculostomía endoscópica en una paciente con hidrocefalia crónica. Neurología. 2015;30:181–183.
This study was presented in poster format at the 18th Congress of the Spanish Society of Neurosurgery, 14–17 May 2013.