In 1988, Lance et al.1 described a syndrome consisting of unilateral facial flushing and sweating triggered by exercise or hot weather. They called it ‘Harlequin syndrome’ (HS) based on Harlequin, a Commedia dell’Arte character. As a general rule, HS is a benign condition caused by a dysfunction in the upper thoracic sympathetic pathway. When it affects the first thoracic segment (T1), it is associated with ipsilateral Horner syndrome due to oculosympathetic fibre involvement. HS is a rare disease affecting autonomic innervation. Although benign in most cases, it is extremely distressing for patients and a diagnostic challenge for doctors.
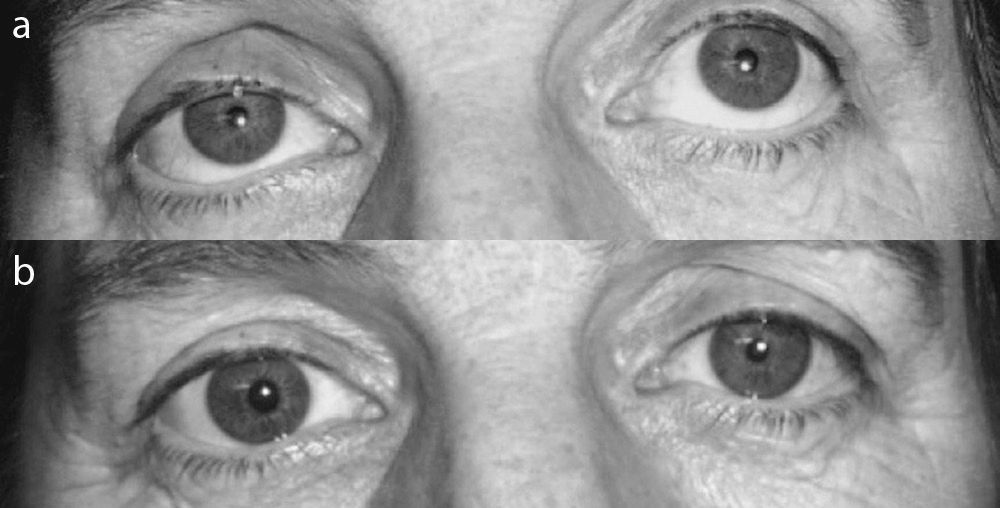
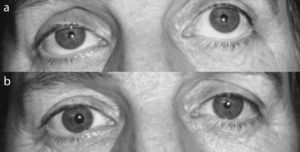
We present the case of a 54-year-old woman with long-standing right palpebral ptosis. She had no relevant personal or family history. Approximately 4 years earlier, she had noticed a narrowing of the right palpebral fissure, which was sometimes more pronounced with no apparent trigger factor. She had never experienced diplopia, dysphagia, excessive limb fatigue, or any other signs or symptoms suggesting a neuromuscular disease. The patient's medical records reported a 15-year history of left-sided facial flushing and profuse sweating with the right side of the face remaining pale and dry (Fig. 1). These episodes were triggered by physical exercise and were especially noticeable in hotter settings. The patient described a distinct frontier between the two halves of her face, and regarded the prominent left-sided facial flushing as a source of social embarrassment. Physical examination revealed mild right palpebral ptosis and slight anisocoria with right miosis. Irises were the same colour, and pupillomotor response was normal. Results from the general and neurological examinations were normal. In light of the above, we suspected a lesion in the sympathetic pathway affecting vasomotor and sudomotor fibres in the right side of the face (consistent with HS), possibly associated with Horner syndrome. Results from the analyses (complete blood count, erythrocyte sedimentation rate, glucose test, a serum electrolyte study, renal and thyroid function studies, etc.) were normal. Neuroimaging studies (cranial and cervical MRI, duplex Doppler ultrasonography of the supra-aortic trunks, and thoracic computerized tomography) showed no relevant abnormalities. A negative apraclonidine test ruled out Horner syndrome. However, instillation of phenylephrine 10% reversed ptosis, and the patient was diagnosed with aponeurotic ptosis (Fig. 2). Once we determined the patient showed no structural changes, she was diagnosed with idiopathic HS and informed that it was a benign condition requiring no treatment. The patient was also offered surgical treatment for the aponeurotic ptosis but she refused since the condition was not functionally debilitating.
HS is a rare autonomic disorder whose main symptom is the appearance of hemifacial flushing and sweating attacks, generally triggered by hot weather or physical exertion. Flushing and sweating does not occur on one side due to ipsilateral dysfunction of the vasomotor and sudomotor sympathetic pathways.2 Researchers postulate that compensatory neuronal activity on the healthy side accentuates the skin symptoms typical of the disease. Dysfunction may be located at any of the three levels in the cervical sympathetic chain. The first neuron originates in the hypothalamus. It descends along the brainstem into the spinal cord, where it forms a synapse with the second (preganglionic) neuron of the intermediolateral column, at the level of segments C8-T2. The preganglionic neuron leaves the spinal cord, travels through the stellate ganglion, and ascends to the superior cervical ganglion through the paravertebral sympathetic chain, which is in contact with the apex of the lung. The second (preganglionic) and third (postganglionic) neurons form a synapse in the superior cervical ganglion. Two branches leave this ganglion. One runs along the internal carotid artery and includes the vasomotor and sudomotor fibres innervating the nose and medial frontal region and the sympathetic fibres which cause the iris to dilate; the second branch runs along the external carotid artery and includes vasomotor and sudomotor postganglionic fibres that innervate the rest of the face.
HS is usually benign. It has been described in up to 10% of healthy newborns and it is associated with a temporary imbalance in the tone of cutaneous blood vessels due to hypothalamic immaturity.3 However, many different aetiologies for HS have been described, including dissection of the carotid artery,4 toxic goitre,5 tumours,6–8 syringomyelia,9 multiple sclerosis,10 and iatrogenic effects of invasive procedures.11–14 Researchers have recently attempted to find a pathogenic connection between migraine and HS based on the autonomic dysfunction associated with migraine. However, this correlation is yet to be established.15
The term ‘Harlequin syndrome’ should be used exclusively for attacks of flushing and sweating which are not associated with any other neurological symptoms. When these symptoms appear in conjunction with other autonomic disorders, the term ‘Harlequin sign’ should be used.16
The diagnostic process for patients with HS should attempt to determine the organic cause. If symptoms are idiopathic, it is essential to assure patients that the disorder is benign and that follow-up examinations will not be necessary.
Although idiopathic cases require no treatment, contralateral sympathectomy can be performed when HS has a severe psychological impact on patients. However, this surgical procedure may lead to compensatory flushing and sweating in other locations.16
Please cite this article as: Zabalza Estévez RJ, Unanue López F. Síndrome de Arlequín, una rareza neurológica. Neurología. 2015;30:185–187.