Impulsivity is a psychological phenomenon that has not been extensively studied in headache patients. We aim to assess the presence of impulsivity in patients with chronic migraine (CM) and medication overuse (MO).
PatientsAll patients examined in an outpatient headache clinic between January 2013 and March 2014 were included. Episodic migraine, CM, and MO were diagnosed according to ICHD-III beta criteria. We prospectively gathered demographic and clinical characteristics. Mood disorders were evaluated using the Hospital Anxiety and Depression Scale (HADS) and impulsiveness was assessed with the Plutchik Impulsivity Scale.
ResultsA total of 155 patients were included (22 men, 133 women). The mean age (SD) was 38.2 (11.7) years (range, 18-70); 104 patients (67.1%) presented CM and, among them, 74 (71.1%) had MO. Of the patient total, 28.4% met criteria for anxiety, 7.1% for depression and 16.1% for impulsivity. The CM group showed higher scores for HADS-anxiety (8.5 [SD 4.5] vs 6.4 [SD 3.6], P=.003) and HADS-depression (4.4 [4.3] vs 1.9 [2.3], P<.001). Among CM cases only, scores for HADS-anxiety (9.3 [4.4] vs 6.8 [4.3], P=.01) and HADS-Depression (5.1 [4.6] vs 2.7 [2.9], P=.002) were higher in patients who also had MO. We found no associations between Plutchik scale scores or presence of impulsivity with either CM or MO.
ConclusionImpulsivity is a common trait in our population of migraine patients, but unlike mood disorders, it is not correlated with either CM or MO.
La impulsividad es una dimensión psicológica no estudiada en profundidad en pacientes con cefalea. Pretendemos evaluar su influencia en la presencia de una migraña crónica (MC) o uso excesivo de medicación (UEM).
PacientesPacientes atendidos consecutivamente en una consulta de cefaleas (enero de 2013-marzo de 2014). Diagnosticamos migraña episódica, MC o UEM de acuerdo con la Clasificación Internacional de Cefaleas, versión beta de la III edición (CIC-III). Recogimos prospectivamente características demográficas y clínicas. Evaluamos trastornos del ánimo mediante la Escala de Ansiedad y Depresión Hospitalaria (HADS) y la impulsividad con la Escala de Plutchik.
ResultadosCiento cincuenta y cinco pacientes (22 varones, 133 mujeres), edad 38,2±11,7 años (18-70); 104 (67,1%) con MC y entre ellos 74 (71,1%) con UEM. El 28,4% de los 155 pacientes incluidos en la serie cumplía criterios de ansiedad, el 7,1% de depresión, y el 16,1% de impulsividad. Las puntuaciones de las subescalas HADS-ansiedad (8,5±4,5 vs. 6.4±3.6, p: 0.003) y HADS-depresión (4,4±4,3 vs. 1,9±2,3, p<0,001), eran mayores en los casos con MC. Entre los pacientes con MC, HADS-ansiedad (9,3±4,4 vs. 6,8±4,3, p: 0,01) y HADS-depression (5,1±4,6 vs. 2,7±2,9, p: 0,002) eran más altas en aquellos con UEM. No encontramos relación entre la presencia de impulsividad o la puntuación en la Escala de Plutchik y la MC o UEM.
ConclusionesEn nuestra población de migrañosos la impulsividad es frecuente, pero, a diferencia de los estados de ánimo, no se correlaciona con MC o UEM.
Psychiatric disorders, which are common in patients with migraine,1,2 are increasingly being documented in the literature. The most frequent disorders in this population are major depression and anxiety disorders.3,4 Psychiatric comorbidities have been associated with poorer response to treatment, medication overuse (MO), and migraine transformation.5–7 Furthermore, certain personality profiles have been linked to pain coping strategies that make migraine management more difficult.8,9
MO is one of the main risk factors for transformation to chronic migraine (CM).10,11 This behaviour may be due to 2 main causes. On the one hand, increasing the dose of symptomatic medication may merely respond to an increase in the number of days with pain. Meanwhile, MO has been associated with certain personality traits that lead patients to take medication out of fear of experiencing new episodes of pain, especially episodes of intense pain that interfere with daily living activities.12 This second hypothesis is especially relevant for the purposes of our study.
Until now, few studies have analysed personality traits in patients with migraine and their influence on MO and CM.13–16 For example, a tendency to increase analgesic consumption rapidly and progressively, which ultimately leads to MO, may be associated with impulsivity. Impulsive patients are characterised by a tendency to act quickly since they usually underestimate the consequences of their actions. This type of patients may lose control of their analgesic consumption, something that cannot be managed with preventive medication for migraine, making it harder to manage their condition. Therefore, screening for impulsivity traits may help clinicians provide a more accurate prognosis and choose the best treatment for each patient.12
The purpose of this study is to evaluate impulsivity in migraine patients in different clinical situations and determine whether there is a connection between this personality trait and a stronger tendency towards symptomatic MO or transformation to CM.
Material and methodsWe included consecutive patients whose initial visit to the headache unit of a tertiary hospital took place between January 2013 and March 2014. Patients were diagnosed with episodic migraine (EM), CM, or MO based on the third edition of the International Classification of Headache Disorders, beta version (ICHD-3).17 None of the patients were evaluated during a migraine attack. We excluded all patients with medical conditions or psychiatric disorders not listed within the group of mood and anxiety disorders, and those having intellectual deficits able to limit their ability to understand or reply to any of the items on the questionnaires. We prospectively gathered the patients’ sociodemographic data, whether they had EM or CM, and time in years from initial migraine episode. We also recorded the number of headache days during the previous month. Patients with high-frequency EM (10-15 pain days per month) were excluded since we consider this type of migraine to overlap with CM, even though the ICHD-3 recognises it as EM. We also gathered data on MO, any history of psychiatric disorders or drug abuse, and use of psychiatric medication or preventive treatments for migraine.
The Headache Impact Test-6 (HIT-6) was used to assess the impact of migraine; this test includes 6 multiple-choice items and establishes 4 levels of disability: severe (≥60 points), moderate (56-59), mild (50-55), and no disability (≤49).18
The Hospital Anxiety and Depression Scale (HADS) was used to detect mood and anxiety disorders.19 HADS is a screening tool that detects anxiety and depression disorders. It is a self-assessment scale with which patients are asked to rate their feelings in the previous week. It has been adapted and validated in Spanish and includes 14 items grouped into 2 subscales: anxiety and depression. None of these items refer to somatic symptoms, which is very useful for migraine patients as a means of preventing overestimates of psychological distress due to mistaking migraine-related physical symptoms for somatic symptoms secondary to anxiety or depression. The cut-off point for each of the subscales is 10.
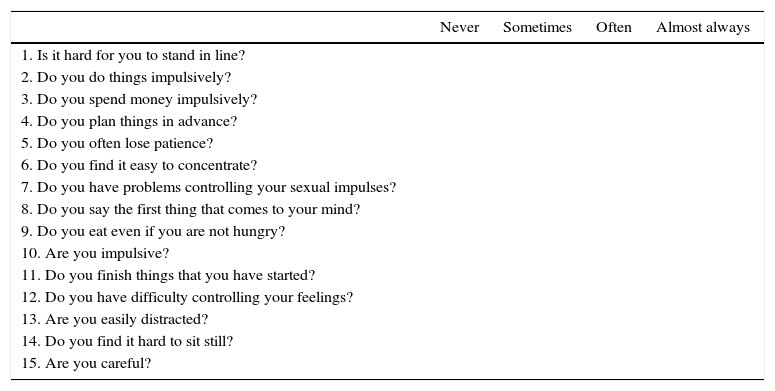
To measure impulsivity, we used the Plutchik Impulsivity Scale (PIS).20 This is a self-assessment test designed to evaluate impulsive behaviour. This screening tool, which has been validated in Spanish, is quick and easy to use (it takes 2-5min to complete). The PIS includes 15 items which address the patient's tendency to ‘do things without reflecting’ or act on impulse. All items evaluate a potential lack of control over planning ability (3 items); emotions (3); eating, spending money, or sexual impulses (3); and other behaviours (6) (Table 1). Responses are scored from 0 to 3 points (never, sometimes, often, almost always). Items 4, 6, 11, and 15 are reverse-scored. Total scores range from 0 to 45 points. The authors of the Spanish-language version propose a cut-off point of 20, with a sensitivity of 60% and a specificity of 74%. Internal consistency was 0.9 (Cronbach's alpha) and test–retest reliability was 0.91 (Pearson's r).
Plutchik Impulsivity Scale.
| Never | Sometimes | Often | Almost always | |
|---|---|---|---|---|
| 1. Is it hard for you to stand in line? | ||||
| 2. Do you do things impulsively? | ||||
| 3. Do you spend money impulsively? | ||||
| 4. Do you plan things in advance? | ||||
| 5. Do you often lose patience? | ||||
| 6. Do you find it easy to concentrate? | ||||
| 7. Do you have problems controlling your sexual impulses? | ||||
| 8. Do you say the first thing that comes to your mind? | ||||
| 9. Do you eat even if you are not hungry? | ||||
| 10. Are you impulsive? | ||||
| 11. Do you finish things that you have started? | ||||
| 12. Do you have difficulty controlling your feelings? | ||||
| 13. Are you easily distracted? | ||||
| 14. Do you find it hard to sit still? | ||||
| 15. Are you careful? |
Responses are scored on a scale from 0 to 3. Items 4, 6, 11, and 15 are reverse-scored.
Source: García-Portilla et al.33
We compared demographic and clinical characteristics as well as results on the different scales (or presence of anxiety, depression, or impulsivity according to those scales) between the groups with EM and CM, and between patients with and without MO within the CM group. Either the t test or the chi-square test was used according to the data distribution. Statistical analysis was performed with SPSS software version 22.0.
ResultsWe included 155 patients (22 men, 133 women). Mean age at time of inclusion was 38.2±11.7 years (range, 18-70) and time since initial migraine was 19.2±13.3 years (range, 0-54). The number of pain days during the previous month was 17.9±10.4 (range, 1-30).
Fifty-one patients (32.9%) had EM and 104 (67.1%) had CM; 74 of the latter (71.1%) reported MO.
Twenty-two patients had a history of anxiety and/or depression (14.2%), although only 12 of them (7.7%) were taking psychoactive drugs at the time of inclusion. Regarding drug use, 47 patients (30.3%) were smokers and 25 (16.1%) were former smokers. Thirty-four patients (21.9%) were receiving preventive treatment for migraine.
Migraine severity according to the HIT-6 scale was 61.3±6.5 (range, 42-78); in 82.8% of the patients, disability was at least moderate (HIT-6>55).
Mean scores in our patient sample were 7.9±4.3 (range, 0-17) on the HADS anxiety subscale, 3.6±3.9 (range, 0-18) on the HADS depression subscale, and 14.1±6.7 (range, 1-32) on the PIS. After applying the corresponding cut-off points, 28.4% of the patients met the criteria for anxiety, 7.1% for depression, and 16.1% for impulsivity.
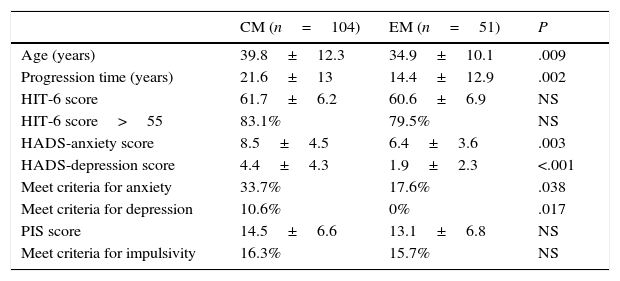
Scores on the HADS anxiety and depression subscales, and the percentage of patients meeting the criteria for anxiety and depression, were significantly higher in the group with CM than in the group with EM (Table 2).
Characteristics of the patient sample by type of migraine.
| CM (n=104) | EM (n=51) | P | |
|---|---|---|---|
| Age (years) | 39.8±12.3 | 34.9±10.1 | .009 |
| Progression time (years) | 21.6±13 | 14.4±12.9 | .002 |
| HIT-6 score | 61.7±6.2 | 60.6±6.9 | NS |
| HIT-6 score>55 | 83.1% | 79.5% | NS |
| HADS-anxiety score | 8.5±4.5 | 6.4±3.6 | .003 |
| HADS-depression score | 4.4±4.3 | 1.9±2.3 | <.001 |
| Meet criteria for anxiety | 33.7% | 17.6% | .038 |
| Meet criteria for depression | 10.6% | 0% | .017 |
| PIS score | 14.5±6.6 | 13.1±6.8 | NS |
| Meet criteria for impulsivity | 16.3% | 15.7% | NS |
CM, chronic migraine; EM, episodic migraine; NS, not significant.
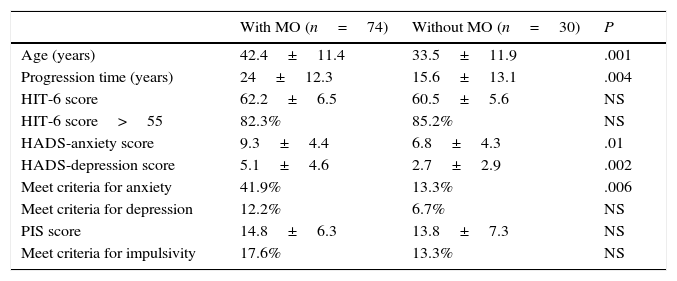
Within the CM group, HADS scores for anxiety and depression, and the percentage of patients with anxiety, were both significantly higher in the group reporting MO (Table 3).
Characteristics of CM patients with or without MO.
| With MO (n=74) | Without MO (n=30) | P | |
|---|---|---|---|
| Age (years) | 42.4±11.4 | 33.5±11.9 | .001 |
| Progression time (years) | 24±12.3 | 15.6±13.1 | .004 |
| HIT-6 score | 62.2±6.5 | 60.5±5.6 | NS |
| HIT-6 score>55 | 82.3% | 85.2% | NS |
| HADS-anxiety score | 9.3±4.4 | 6.8±4.3 | .01 |
| HADS-depression score | 5.1±4.6 | 2.7±2.9 | .002 |
| Meet criteria for anxiety | 41.9% | 13.3% | .006 |
| Meet criteria for depression | 12.2% | 6.7% | NS |
| PIS score | 14.8±6.3 | 13.8±7.3 | NS |
| Meet criteria for impulsivity | 17.6% | 13.3% | NS |
CM, chronic migraine; NS, not significant; MO, medication overuse.
We found no connection between presence of CM or MO and scores on the PIS or for scores higher than the cut-off point for impulsivity.
DiscussionImpulsivity is one of the most basic and relevant personality traits. It is a widely used concept and should therefore be defined each time it is used since there are different notions of what constitutes impulsivity. Despite the marked heterogeneity among current theories, authors agree in many areas. Impulsive behaviour almost always responds to 3 underlying mechanisms: reward-seeking personality, acting without planning, and compulsively seeking relief from tension or stress.21
In the case of migraine, impulsivity may be responsible for anxiety resulting from anticipating pain, which may lead to losing control over consumption of symptomatic medication. This neurobehavioural phenomenon may promote rapid and increased analgesic use and the consequent tendency towards symptomatic MO; as previously stated, MO is a major risk factor for migraine transformation.10,11,22 This is the reason why we decided to study this personality trait in patients with EM or CM and its connection with MO.
In our view, the PIS is a reliable screening tool for impulsivity. It evaluates impulsive behaviours with items examining potential lack of control over certain distinct behaviours20: planning abilities, emotions, basic reactions, and other types of conduct.
Treatment will vary according to whether symptomatic MO is due to an increasing need for pain relief or to certain behavioural patterns, such as cognitive impulsivity.23 Whereas identifying the most effective preventive drug for each patient would be enough in the first case, these drugs would probably be less effective in the second case. These latter patients need a multidisciplinary approach including psychological treatment for pathological behaviours. Distinguishing between these 2 patient profiles may optimise triage and improve treatment strategies.
Our study design did not include patients with high-frequency EM (10-15 headache days per month). These patients form part of the EM group according to the ICHD-3; therefore, excluding them constitutes a selection bias. However, we agree with other authors24 that setting the cut-off point at 15 days to distinguish EM from CM is arbitrary: in our view, patients with high-frequency EM share more features with CM patients than with EM patients. This premise underlies the current study and other ongoing studies conducted by our research group.
We should also highlight that the groups with CM and EM were quite similar in age and disability status. Regarding age, patients with CM visit our headache unit at a fairly young age, as we mentioned previously25; this may reflect our efforts to provide information about CM to all doctors referring patients to our unit. As for severity, patients with EM scored very high on the HIT-6. This may be due to a selection bias since all cases of EM presented here were patients referred to a specialist unit.
Our series shows a strong association between presence of mood disorders and CM or MO. The high prevalence of mood disorders in these patients has already been described in the literature.14 Curone et al. state that 44% of patients with CM and MO also have mood disorders.12 Raggi et al. compared mood and disability between patients with EM, with and without MO, and those with CM and found that the patients with CM and MO scored significantly higher on the Beck Depression Inventory.26 However, it is not known whether mood disorders in these patients are linked to chronicity of migraine or to symptomatic MO.
The terms ‘pain panic’ or ‘cephalgiaphobia’,27 first used by Harvey Featherstone, describe a powerful, uncontrolled fear of experiencing a migraine attack, which results in an urgent need to self-medicate compulsively while disregarding the potential consequences. This behaviour typically leads to MO and may be present in patients with CM whose pain is difficult to manage. As mentioned previously in this section, these actions correspond, to a certain extent, to impulsive behaviour.
According to PIS results, impulsivity was frequent in our sample, although the lack of a control group does not allow us to draw definitive conclusions. However, we found no correlations between CM or MO and impulsivity.
To date, no other published studies have analysed impulsive behaviour in migraine patients, or the association between that behaviour and MO or CM; therefore, we cannot compare our results to any other findings. However, some authors have described other psychological profiles linked to certain pain coping patterns which are associated with more difficult treatment and poorer outcomes.12 For example, a tendency to take medications compulsively has been linked to obsessive-compulsive personality traits. According to Curone and Cupini, symptomatic MO linked to those personality traits affects patients’ responses to preventive treatment. This has an impact on the progression of migraine, leading to transformation into CM in many cases.14,15 In the past years, there have been many advances in the study of orbitofrontal dysfunction, with approaches ranging from the neuropsychological28 to the structural,29 in patients with MO.
The lack of a correlation between impulsivity and MO may be due to choosing the wrong screening tool, erroneously regarding impulsivity as a personality trait, not assessing overall personality types, or simply because impulsivity is not associated with MO in these patients.
However, in view of the high percentage of patients meeting criteria for impulsivity, we should not rule out the idea that this personality trait may have a significant effect on response to pain, preventive treatment, or other therapies administered to these patients.
Regarding the neurobiological substrate of impulsivity, impulsive patients show dysfunction in the pathways that mediate generation and regulation of emotions (corticolimbic and corticostriatal).30 Dysfunction in these pathways is mediated by alterations in the main modulatory neurotransmitters (serotonin, norepinephrine) and by changes in the white and grey matter.27 Impulsive patients display alterations in emotional regulation in response to external or internal stimuli,31 and pain is a negative external/internal stimulus. It could be hypothesised that there is a connection between the neurobiological basis of impulsivity and that of pain, especially chronic pain. The International Association for the Study of Pain highlights the subjectivity of pain as well as its multiple dimensions (sensory, affective, motivational).
Abnormal data processing in migraine patients may alter coping strategies,32 that is, the cognitive and behavioural efforts that a patient adopts in order to manage, reduce, or tolerate external and internal stimuli threatening their well-being. Questions remain about whether impulsivity might affect dysfunctional pain coping strategies, such as those leading to the previously mentioned ‘pain panic’ phenomenon. For this reason, we currently assess personality from a multidimensional perspective and evaluate any potential differences in response to preventive treatment according to the presence or absence of impulsivity.
ConclusionsMood disorders, especially anxiety disorders, are frequent in patients with migraine. There is a strong association between mood/anxiety and both CM and MO; we therefore recommend systematically screening for these psychological comorbidities in these patients.
Patients with migraine often display impulsivity. Although we found no correlation between this trait and CM or MO, this does not mean that impulsivity might not be a decisive factor in pain coping strategies and response to preventive medication in these patients.
We need further studies on the hypothetical relationship between the neurobiological basis of impulsivity and pain (especially chronic pain), and the negative impact of impulsivity on pain coping strategies. Abnormal psychological profiles in patients with migraine may have significant clinical and therapeutic consequences. Psychological evaluations provide additional data which may be helpful for choosing the best treatment option for each patient.
FundingThis study has received no funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Muñoz I, Hernández MS, Pedraza MI, Domínguez E, Ruiz M, Isidro G, et al. Impulsividad en pacientes migrañosos: estudio en una serie de 155 casos. Neurología. 2016;31:599–605.
Study partially presented as an oral communication at the 65th Annual Meeting of the Spanish Society of Neurology, Barcelona, November 2013.