Greater understanding of the prevalence and incidence of multiple sclerosis in Spain and their temporal trends is necessary to improve the allocation of healthcare resources and to study aetiological factors.
MethodsWe performed a systematic search of the MedLine database and reviewed the reference lists of the articles gathered. We collected studies reporting prevalence or incidence rates of multiple sclerosis in any geographical location in Spain, with no time limits. In 70% of cases, data were extracted by 2 researchers (FGL and EAC); any discrepancies were resolved by consensus.
ResultsWe identified 51 prevalence and 33 incidence studies published between 1968 and 2018. In the adjusted analysis, the number of prevalent cases per 100 000 population increased by 26.6 (95% confidence interval [CI], 21.5–31.8) every 10 years. After adjusting for year and latitude, the number of incident cases per 100 000 population increased by 1.34 (95% CI, 0.98–1.69) every 10 years. We observed a trend toward higher prevalence and incidence rates at higher latitudes.
ConclusionsThe prevalence of multiple sclerosis in Spain has increased in recent decades, although case ascertainment appears to be incomplete in many studies. Incidence rates have also increased, but this may be due to recent improvements in the detection of new cases.
El conocimiento de la prevalencia y de la incidencia de la esclerosis múltiple en España y de sus tendencias temporales es necesario para planificar mejor los servicios clínicos y estudiar factores etiológicos.
MétodoSe efectuó una revisión sistemática, mediante una búsqueda en Medline y en las referencias de cada artículo, de todos los estudios que describieran cifras de prevalencia o de incidencia de la esclerosis múltiple en algún lugar geográfico de España, sin límites temporales. En el 70% de los casos la extracción de datos la hicieron dos observadores (FGL y EAC), que resolvieron las discrepancias por consenso.
ResultadosSe identificaron 51 estudios de prevalencia y 33 de incidencia entre 1968 y 2018. En el análisis ajustado, por cada 10 años la prevalencia por 100 000 habitantes aumentó en 26,6 (intervalo de confianza —IC— del 95%, 21,5 a 31,8). Según los datos del análisis ajustado por el año y la latitud, por cada 10 años la incidencia por 100 000 habitantes aumentó en 1,34 (IC 95%, 0,98 a 1,69). Se observó una tendencia de mayores prevalencias e incidencias en latitudes más altas.
ConclusionesLa prevalencia de la esclerosis múltiple aumentó en las últimas décadas en España, aunque en muchos estudios la verificación de casos parece haber sido incompleta. La incidencia también aumentó, pero eso puede deberse a una detección de casos nuevos más exhaustiva en los últimos años.
Multiple sclerosis (MS) is a chronic neurological disease characterised by destruction of myelin in the central nervous system, leading to varying degrees of axonal and neuronal damage. It causes a wide range of symptoms, which frequently worsen over time, leading to disability. MS is the second leading cause of neurological disability in young adults, after trauma.1,2
MS is an autoimmune disease with a progressive degenerative component. Although its aetiology is unknown, a combination of environmental factors and genetic predisposition are thought to play a role. Environmental factors include Epstein-Barr virus infection, low exposure to sunlight, and low vitamin D levels. At least 233 genetic loci associated with the disease have been identified, 32 of which are located in the major histocompatibility complex.3,4
Temporal trends in the incidence of MS may help to improve our understanding of its aetiology. However, given the difficulty of studying the incidence of MS, many hypotheses are based on prevalence data. The most widely accepted hypothesis is that formulated by Kurtzke,5 who established 3 bands of high, medium, and low frequency according to geographical latitude, with prevalence being greater at higher latitudes. Spain is located in the medium-prevalence band.
Many prevalence studies have been conducted in Spain,6,7 revealing a steady increase in the crude prevalence of MS over time. Spain seems to have become a country with a high prevalence of MS. The incidence of MS in Spain has also been studied,6,7 though less extensively and with highly heterogeneous results.
The purpose of this study was to analyse and update the information on the incidence and prevalence of MS in Spain.
MethodsDesignWe performed a systematic review of the literature.
Data sourcesWe performed a literature search on MEDLINE, using the PubMed search engine. We also reviewed the works cited in the reference sections of the original articles and literature reviews gathered in the literature search.
The search strategy used was as follows: ((“multiple sclerosis”[MeSH Terms] OR (“multiple”[All Fields] AND “sclerosis”[All Fields]) OR “multiple sclerosis”[All Fields]) AND (“epidemiology”[MeSH Subheading] OR “epidemiology”[All Fields] OR “prevalence”[All Fields] OR “prevalence”[MeSH Terms] OR “prevalence”[All Fields] OR “prevalences”[All Fields] OR “prevalences”[All Fields] OR “prevalent”[All Fields] OR “prevalently”[All Fields] OR “prevalents”[All Fields] OR (“epidemiology”[MeSH Subheading] OR “epidemiology”[All Fields] OR “incidence”[All Fields] OR “incidence”[MeSH Terms] OR “incidences”[All Fields] OR “incident”[All Fields] OR “incidents”[All Fields]))) AND (“Spain”[MeSH Terms] OR “Spain”[All Fields] OR “Spain s”[All Fields]).
Study selectionWe selected all studies reporting prevalence or incidence rates for MS in any location in Spain, from 1966 to 29 March 2021.
Extraction of dataWe gathered the following data from prevalence studies: location, date of estimation, diagnostic criteria used, sources for case collection, total number of prevalent cases and distribution by sex and age group, population of the geographical area under study and distribution by sex and age group, estimated prevalence, sex ratio, and mean age (standard deviation) at symptom onset.
From each incidence study, the following data were gathered: location, period of estimation, diagnostic criteria used, population of the geographical area under study, and estimated incidence.
For 70% of studies, data were collected by 2 researchers (FJGL and EAC); any discrepancies were solved by consensus.
Main outcome measuresPoint prevalence and incidence are expressed as the number of cases per 100 000 population.
Data synthesis and analysisWe calculated 95% confidence intervals for prevalence and incidence rates using the Poisson distribution. For prevalence rates, we used the reported or calculated cases from each study and the population of the geographical area under study. For incidence rates, we used the population of the geographical area under study to calculate the population corresponding to the period of estimation (person-years) and the number of cases needed to reach the described incidence.
We built forest plots to analyse the results of the included prevalence and incidence studies.8 Given the expected heterogeneity of study results and methodological differences, we decided not to perform a meta-analysis of the data. However, we did assess study heterogeneity with random effects models.
We performed meta-regression analyses9 to analyse the impact of the calendar year and geographical latitude on the incidence and prevalence of MS. The meta-regression analysis of prevalence also included the number of sources used to collect cases as an independent variable, whereas the meta-regression analysis of incidence included the length of the period of estimation, in years. In both cases, we conducted a sensitivity analysis exclusively including studies published in journals indexed in MEDLINE.
All statistical analyses were performed using Stata (version 15).10
Ethics approvalThe study did not involve any patients, biological samples, or personal data; therefore, institutional ethics committee approval was not necessary.
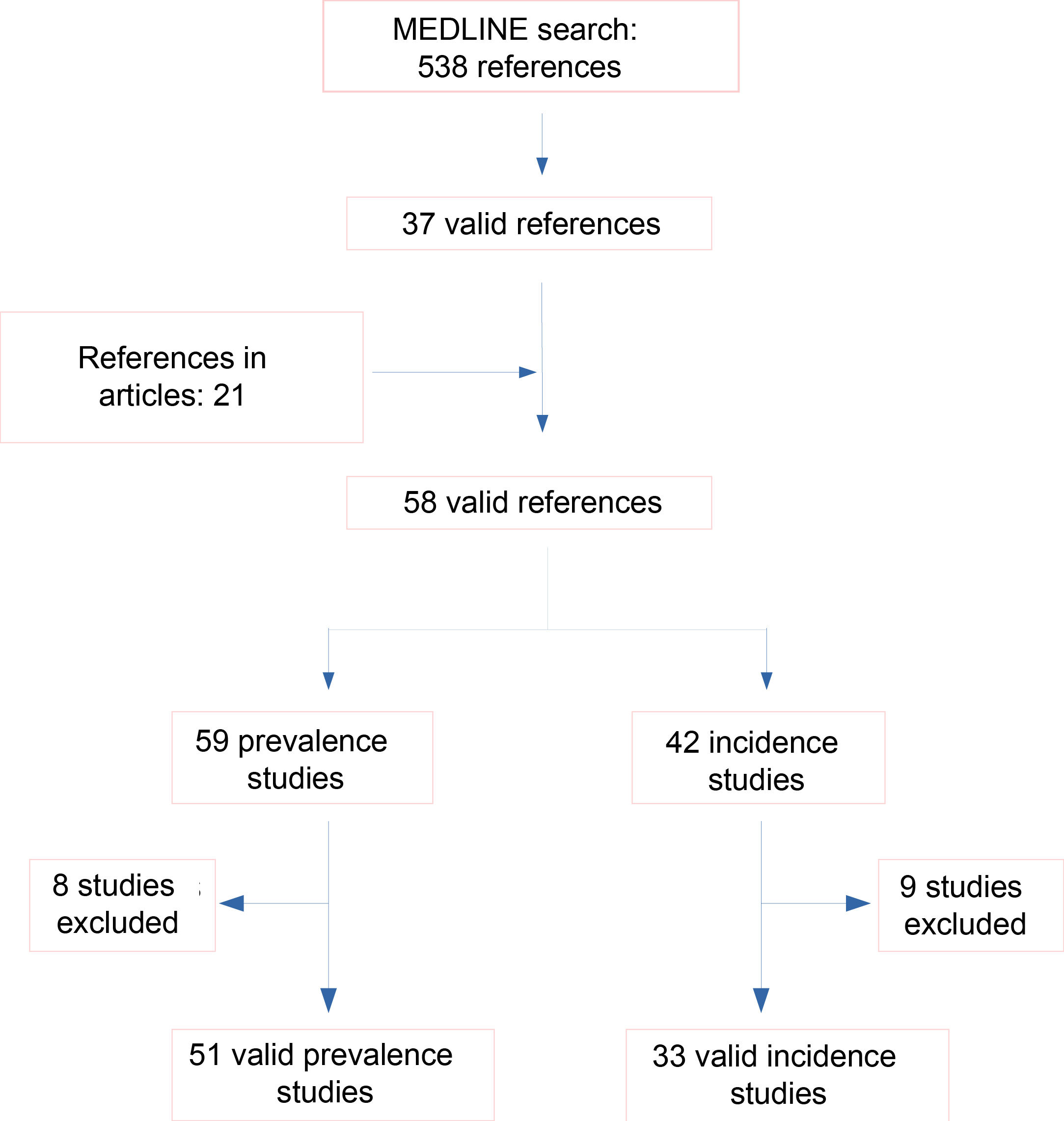
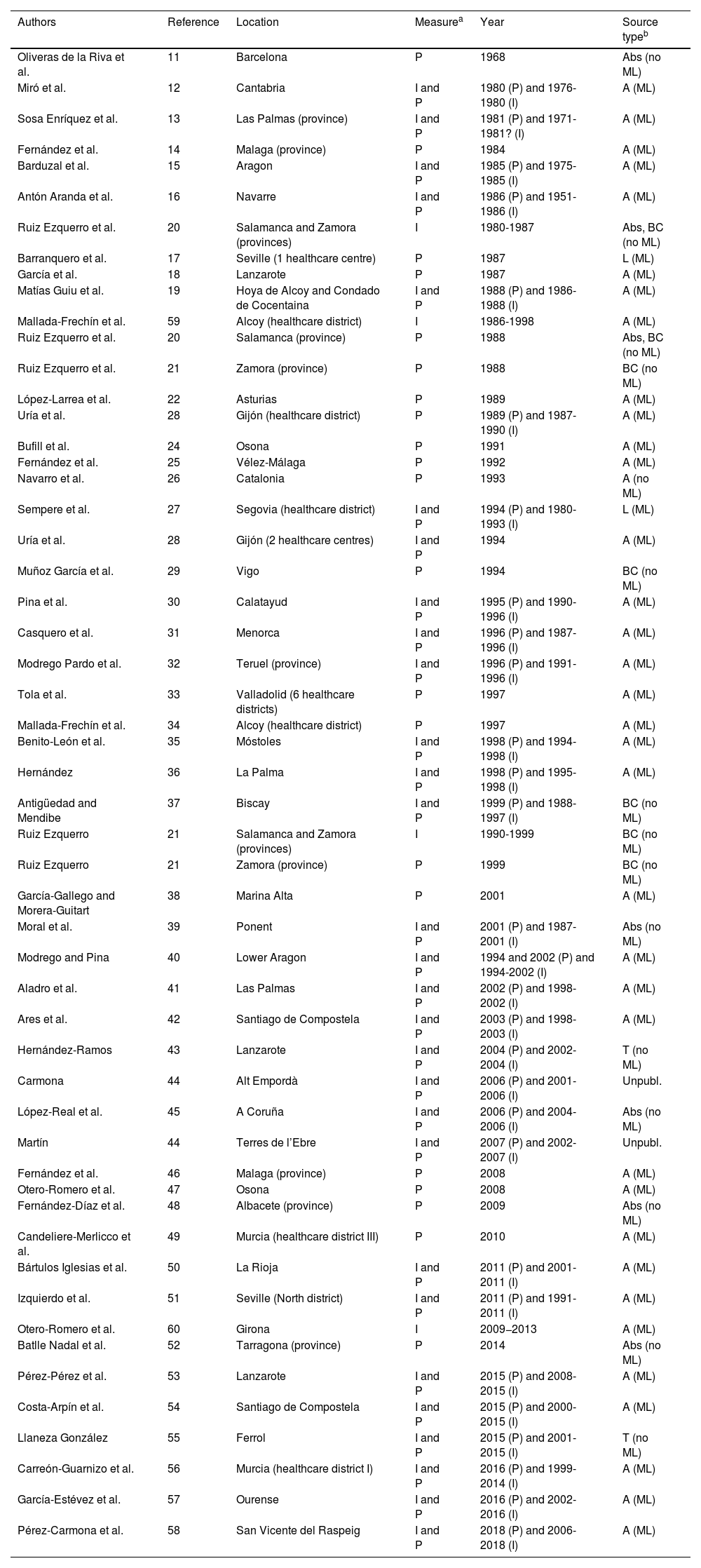
ResultsThe results of our literature search are shown in Fig. 1. We finally selected 51 prevalence studies11–58 and 33 incidence studies,12,13,15,16,19,20,27,28,30–32,35–37,39–45,50,51,53–60 corresponding to a total of 50 bibliographic references (Table 1). We excluded 8 incidence and prevalence studies (conducted in Alcoy,61–63 Osona,64 Ponent,65,66 La Coruña,67 and Ourense68) presenting very similar periods of estimation (less than 5 years apart) to those of other studies exploring the same geographical area. Furthermore, 2 incidence studies included the same period of estimation for overlapping geographical areas; therefore, we excluded the study with the shorter period of estimation.23 Over the total period of over 50 years, studies have been conducted in all Spanish autonomous communities except Extremadura.
Prevalence and incidence studies conducted in Spain included in our systematic review.
| Authors | Reference | Location | Measurea | Year | Source typeb |
|---|---|---|---|---|---|
| Oliveras de la Riva et al. | 11 | Barcelona | P | 1968 | Abs (no ML) |
| Miró et al. | 12 | Cantabria | I and P | 1980 (P) and 1976-1980 (I) | A (ML) |
| Sosa Enríquez et al. | 13 | Las Palmas (province) | I and P | 1981 (P) and 1971-1981? (I) | A (ML) |
| Fernández et al. | 14 | Malaga (province) | P | 1984 | A (ML) |
| Barduzal et al. | 15 | Aragon | I and P | 1985 (P) and 1975-1985 (I) | A (ML) |
| Antón Aranda et al. | 16 | Navarre | I and P | 1986 (P) and 1951-1986 (I) | A (ML) |
| Ruiz Ezquerro et al. | 20 | Salamanca and Zamora (provinces) | I | 1980-1987 | Abs, BC (no ML) |
| Barranquero et al. | 17 | Seville (1 healthcare centre) | P | 1987 | L (ML) |
| García et al. | 18 | Lanzarote | P | 1987 | A (ML) |
| Matías Guiu et al. | 19 | Hoya de Alcoy and Condado de Cocentaina | I and P | 1988 (P) and 1986-1988 (I) | A (ML) |
| Mallada-Frechín et al. | 59 | Alcoy (healthcare district) | I | 1986-1998 | A (ML) |
| Ruiz Ezquerro et al. | 20 | Salamanca (province) | P | 1988 | Abs, BC (no ML) |
| Ruiz Ezquerro et al. | 21 | Zamora (province) | P | 1988 | BC (no ML) |
| López-Larrea et al. | 22 | Asturias | P | 1989 | A (ML) |
| Uría et al. | 28 | Gijón (healthcare district) | P | 1989 (P) and 1987-1990 (I) | A (ML) |
| Bufill et al. | 24 | Osona | P | 1991 | A (ML) |
| Fernández et al. | 25 | Vélez-Málaga | P | 1992 | A (ML) |
| Navarro et al. | 26 | Catalonia | P | 1993 | A (no ML) |
| Sempere et al. | 27 | Segovia (healthcare district) | I and P | 1994 (P) and 1980-1993 (I) | L (ML) |
| Uría et al. | 28 | Gijón (2 healthcare centres) | I and P | 1994 | A (ML) |
| Muñoz García et al. | 29 | Vigo | P | 1994 | BC (no ML) |
| Pina et al. | 30 | Calatayud | I and P | 1995 (P) and 1990-1996 (I) | A (ML) |
| Casquero et al. | 31 | Menorca | I and P | 1996 (P) and 1987-1996 (I) | A (ML) |
| Modrego Pardo et al. | 32 | Teruel (province) | I and P | 1996 (P) and 1991-1996 (I) | A (ML) |
| Tola et al. | 33 | Valladolid (6 healthcare districts) | P | 1997 | A (ML) |
| Mallada-Frechín et al. | 34 | Alcoy (healthcare district) | P | 1997 | A (ML) |
| Benito-León et al. | 35 | Móstoles | I and P | 1998 (P) and 1994-1998 (I) | A (ML) |
| Hernández | 36 | La Palma | I and P | 1998 (P) and 1995-1998 (I) | A (ML) |
| Antigüedad and Mendibe | 37 | Biscay | I and P | 1999 (P) and 1988-1997 (I) | BC (no ML) |
| Ruiz Ezquerro | 21 | Salamanca and Zamora (provinces) | I | 1990-1999 | BC (no ML) |
| Ruiz Ezquerro | 21 | Zamora (province) | P | 1999 | BC (no ML) |
| García-Gallego and Morera-Guitart | 38 | Marina Alta | P | 2001 | A (ML) |
| Moral et al. | 39 | Ponent | I and P | 2001 (P) and 1987-2001 (I) | Abs (no ML) |
| Modrego and Pina | 40 | Lower Aragon | I and P | 1994 and 2002 (P) and 1994-2002 (I) | A (ML) |
| Aladro et al. | 41 | Las Palmas | I and P | 2002 (P) and 1998-2002 (I) | A (ML) |
| Ares et al. | 42 | Santiago de Compostela | I and P | 2003 (P) and 1998-2003 (I) | A (ML) |
| Hernández-Ramos | 43 | Lanzarote | I and P | 2004 (P) and 2002-2004 (I) | T (no ML) |
| Carmona | 44 | Alt Empordà | I and P | 2006 (P) and 2001-2006 (I) | Unpubl. |
| López-Real et al. | 45 | A Coruña | I and P | 2006 (P) and 2004-2006 (I) | Abs (no ML) |
| Martín | 44 | Terres de l’Ebre | I and P | 2007 (P) and 2002-2007 (I) | Unpubl. |
| Fernández et al. | 46 | Malaga (province) | P | 2008 | A (ML) |
| Otero-Romero et al. | 47 | Osona | P | 2008 | A (ML) |
| Fernández-Díaz et al. | 48 | Albacete (province) | P | 2009 | Abs (no ML) |
| Candeliere-Merlicco et al. | 49 | Murcia (healthcare district III) | P | 2010 | A (ML) |
| Bártulos Iglesias et al. | 50 | La Rioja | I and P | 2011 (P) and 2001-2011 (I) | A (ML) |
| Izquierdo et al. | 51 | Seville (North district) | I and P | 2011 (P) and 1991-2011 (I) | A (ML) |
| Otero-Romero et al. | 60 | Girona | I | 2009−2013 | A (ML) |
| Batlle Nadal et al. | 52 | Tarragona (province) | P | 2014 | Abs (no ML) |
| Pérez-Pérez et al. | 53 | Lanzarote | I and P | 2015 (P) and 2008-2015 (I) | A (ML) |
| Costa-Arpín et al. | 54 | Santiago de Compostela | I and P | 2015 (P) and 2000-2015 (I) | A (ML) |
| Llaneza González | 55 | Ferrol | I and P | 2015 (P) and 2001-2015 (I) | T (no ML) |
| Carreón-Guarnizo et al. | 56 | Murcia (healthcare district I) | I and P | 2016 (P) and 1999-2014 (I) | A (ML) |
| García-Estévez et al. | 57 | Ourense | I and P | 2016 (P) and 2002-2016 (I) | A (ML) |
| Pérez-Carmona et al. | 58 | San Vicente del Raspeig | I and P | 2018 (P) and 2006-2018 (I) | A (ML) |
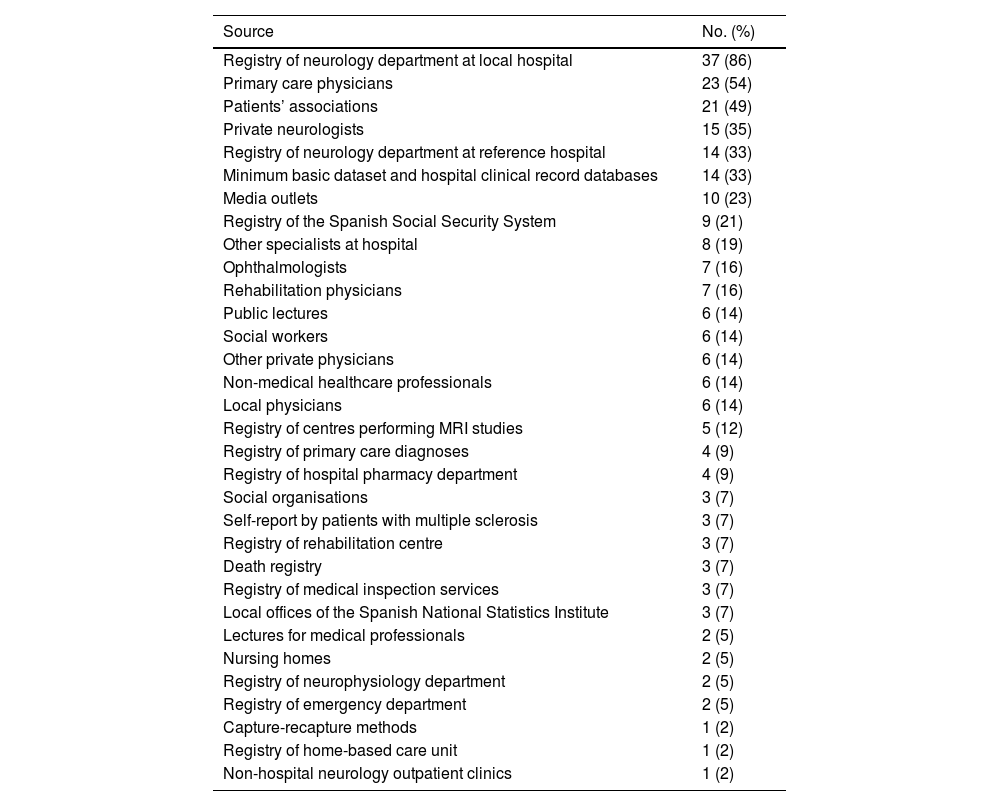
Table 2 lists the sources used for collecting cases of MS in the studies included in our review. The main source was the registry of cases of MS of the neurology department at the local hospital. Other important sources were primary care physicians, patients’ associations, neurologists working in private practice, the registry of cases of MS of the neurology department at the reference hospital, and the minimum basic dataset and hospital clinical record databases. The median number of sources reported in the studies was 4 (range, 0-16; Q1-Q3, 1-6) and the mean number was 4.65.
Frequency of the sources used to identify cases of multiple sclerosis.
| Source | No. (%) |
|---|---|
| Registry of neurology department at local hospital | 37 (86) |
| Primary care physicians | 23 (54) |
| Patients’ associations | 21 (49) |
| Private neurologists | 15 (35) |
| Registry of neurology department at reference hospital | 14 (33) |
| Minimum basic dataset and hospital clinical record databases | 14 (33) |
| Media outlets | 10 (23) |
| Registry of the Spanish Social Security System | 9 (21) |
| Other specialists at hospital | 8 (19) |
| Ophthalmologists | 7 (16) |
| Rehabilitation physicians | 7 (16) |
| Public lectures | 6 (14) |
| Social workers | 6 (14) |
| Other private physicians | 6 (14) |
| Non-medical healthcare professionals | 6 (14) |
| Local physicians | 6 (14) |
| Registry of centres performing MRI studies | 5 (12) |
| Registry of primary care diagnoses | 4 (9) |
| Registry of hospital pharmacy department | 4 (9) |
| Social organisations | 3 (7) |
| Self-report by patients with multiple sclerosis | 3 (7) |
| Registry of rehabilitation centre | 3 (7) |
| Death registry | 3 (7) |
| Registry of medical inspection services | 3 (7) |
| Local offices of the Spanish National Statistics Institute | 3 (7) |
| Lectures for medical professionals | 2 (5) |
| Nursing homes | 2 (5) |
| Registry of neurophysiology department | 2 (5) |
| Registry of emergency department | 2 (5) |
| Capture-recapture methods | 1 (2) |
| Registry of home-based care unit | 1 (2) |
| Non-hospital neurology outpatient clinics | 1 (2) |
Percentages were calculated with a denominator of 52 (total no. of studies indicating the sources for case collection).
Regarding the relative importance of the sources used for case collection, most of the studies providing this information collected over 80%31–33,41 or 90%16,54,56 of the cases from neurology department registries, although in some studies this source provided only a small percentage of the cases (17%19 or 55%24).
Of the 51 studies describing the diagnostic criteria used, 30 (59%) used the Poser criteria; 7 (14%) used the 2001 McDonald criteria; 5 (10%) used the Rose criteria; 4 (8%) used the Poser and the McDonald criteria; one (2%) used the Schumacher, the Poser, and the McDonald criteria; one (2%) used the Boston University Workshop criteria and the Poser criteria; one (2%) used the Poser criteria and the diagnostic criteria proposed by the Multiple Sclerosis International Federation (MSIF) International Medical and Scientific Board; and one (2%) used the McDonald and the Holliday criteria.
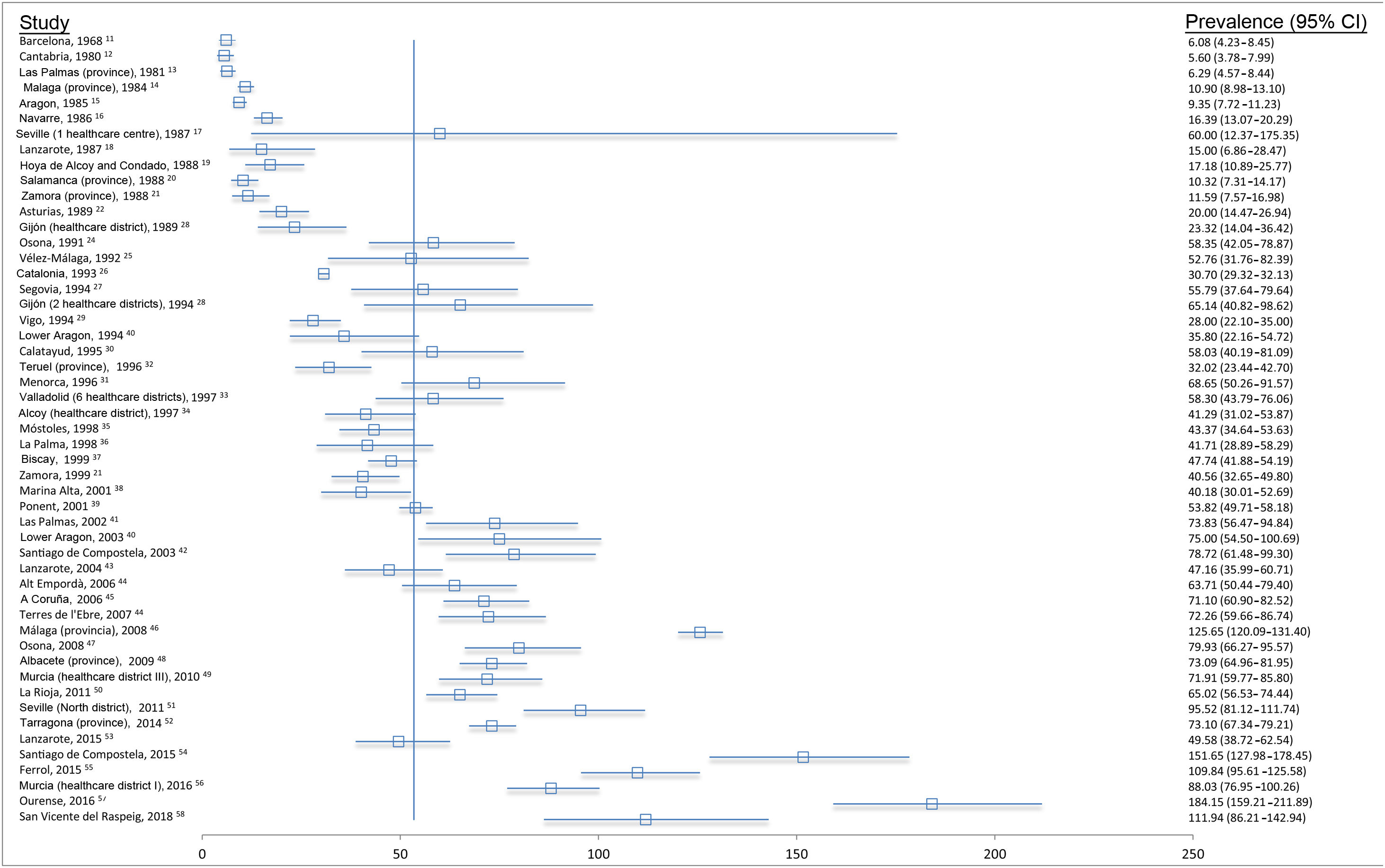
PrevalenceThe prevalence of MS has increased over time (Fig. 2), with rates showing great heterogeneity (Cochran Q = 113.28, df = 50 [P < .00001]; I2 = 56%).
Forest plot of the point prevalence of multiple sclerosis in Spain. The figure shows all the studies, by year (mid-point of the estimation period), and their point prevalence estimates per 100 000 population along with 95% confidence intervals (Poisson distribution). The vertical line indicates the weighted average of the studies (53.41), although no meta-analysis was conducted.
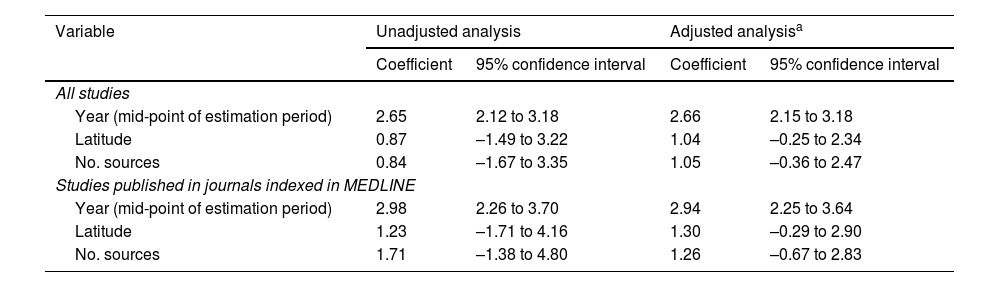
Table 3 shows the meta-regression coefficients for prevalence, considering the impact of year (mid-point of estimation period), latitude, and number of sources used. An association was observed between prevalence and the year of the study, with prevalence rates being higher in more recent years. This association was observed in analyses adjusted and unadjusted for latitude and number of sources. According to data from the adjusted analysis, the prevalence rate increased by 26.6 cases per 100 000 population every 10 years (95% CI: 21.5-31.8). This association was more marked after performing a sensitivity analysis exclusively including studies published in journals indexed in MEDLINE (increase of 29.4 cases per 100 000 population every 10 years; 95% CI, 22.5-36.4).
Meta-regression coefficients of the influence of several factors on the point prevalence of multiple sclerosis, in number of cases per 100 000 population. Adjusted and unadjusted analysis.
| Variable | Unadjusted analysis | Adjusted analysisa | ||
|---|---|---|---|---|
| Coefficient | 95% confidence interval | Coefficient | 95% confidence interval | |
| All studies | ||||
| Year (mid-point of estimation period) | 2.65 | 2.12 to 3.18 | 2.66 | 2.15 to 3.18 |
| Latitude | 0.87 | –1.49 to 3.22 | 1.04 | –0.25 to 2.34 |
| No. sources | 0.84 | –1.67 to 3.35 | 1.05 | –0.36 to 2.47 |
| Studies published in journals indexed in MEDLINE | ||||
| Year (mid-point of estimation period) | 2.98 | 2.26 to 3.70 | 2.94 | 2.25 to 3.64 |
| Latitude | 1.23 | –1.71 to 4.16 | 1.30 | –0.29 to 2.90 |
| No. sources | 1.71 | –1.38 to 4.80 | 1.26 | –0.67 to 2.83 |
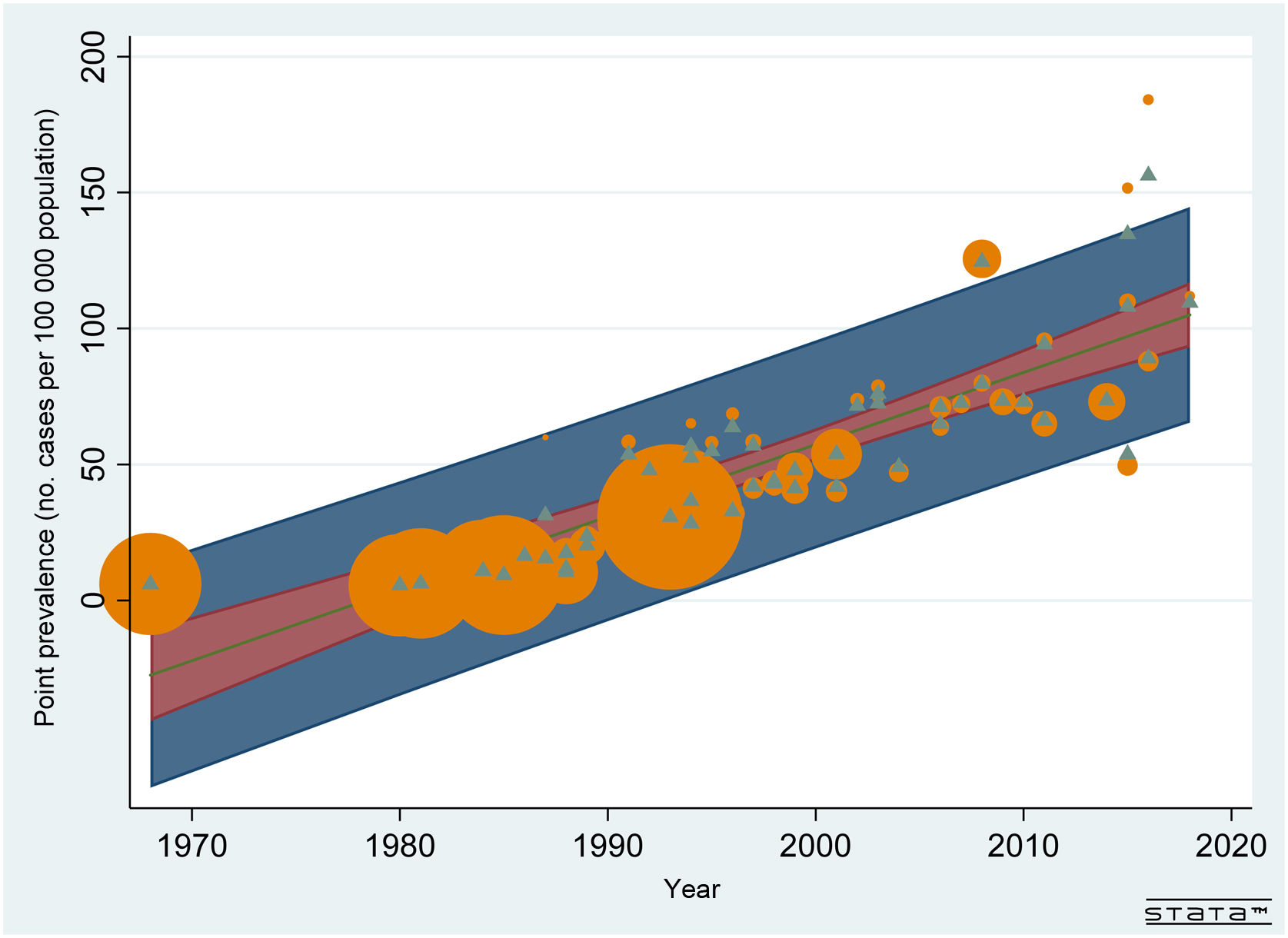
Fig. 3 shows the plot for the unadjusted meta-regression analysis of the point prevalence of MS over time. This association showed an I2 of 97% and an adjusted R2 of 72%.
Meta-regression analysis of the impact of time on the point prevalence of multiple sclerosis. The straight line reflects the predicted prevalence by year (mid-point of the estimation period), the red area reflects the 95% confidence interval, and the dark blue area reflects the prediction interval. Orange circles indicate the observed prevalence rates (size is inversely proportional to total variance), while green triangles reflect empirical Bayes estimates (ie, the predicted prevalence rates of the random effects).
Regarding latitude, the adjusted analysis showed an increase in point prevalence of 10.4 cases per 100 000 population with every 10° increment in latitude (95% CI, –2.5 to 23.4); in the adjusted analysis only including articles from journals indexed in MEDLINE, prevalence increased by 13.0 cases per 100 000 population (95% CI, –2.9 to 29.0).
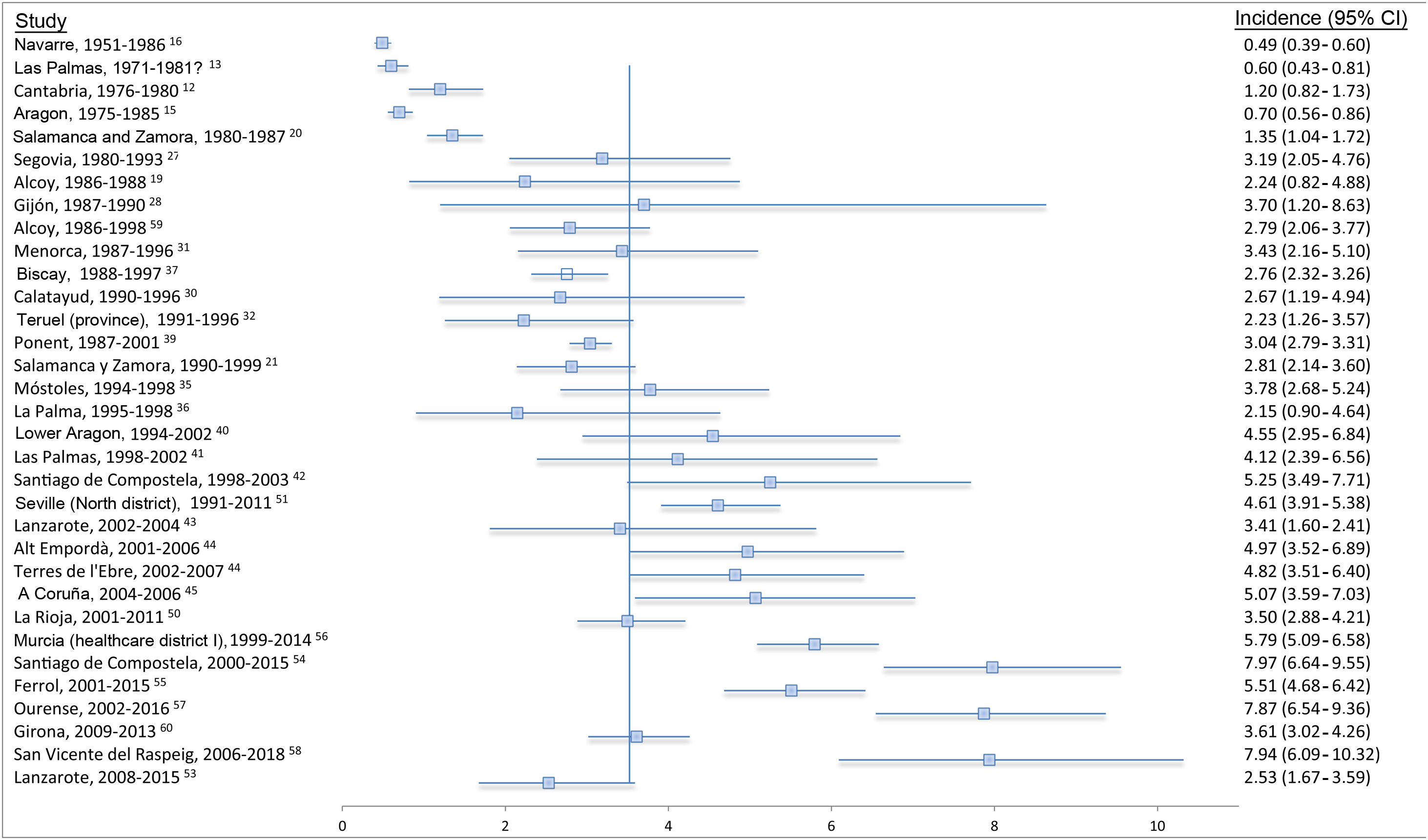
IncidenceFig. 4 presents a forest plot of incidence studies conducted in Spain, ordered by the mid-point of the estimation period. Our results show an increase in the incidence of MS over the years, with moderate heterogeneity of incidence rates (Cochran Q = 51.40, df = 32 [P = .0163]; I2 = 38%).
Forest plot of the incidence of multiple sclerosis in Spain. The figure shows all the studies, by mid-point of the estimation period, and their incidence estimates per 100 000 person-years along with 95% exact confidence intervals (Poisson distribution). The vertical line indicates the weighted average of the studies (3.52), although no meta-analysis was conducted.
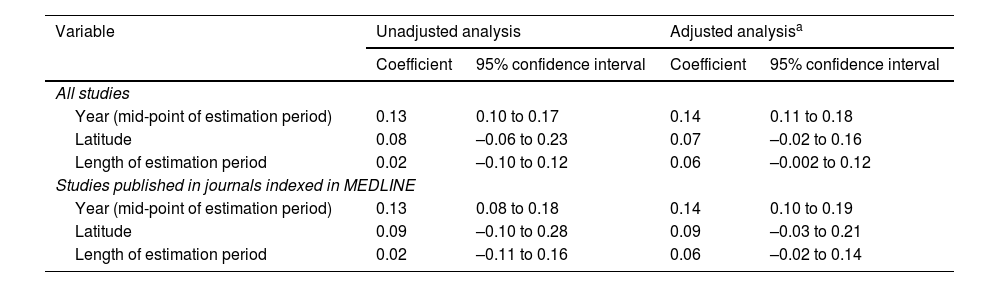
Table 4 shows the meta-regression coefficients for incidence, considering the year (mid-point of estimation period) and latitude. A correlation was observed between incidence and year, with more recent years presenting higher incidence rates. This association was also observed in analyses adjusted and unadjusted for latitude and study duration (in number of years). According to the results of the analysis adjusted for year and latitude, incidence increased by 1.34 cases per 100 000 person-years every 10 years (95% CI, 0.98-1.69). According to the analysis of studies published in journals indexed in MEDLINE, incidence rates increased by 1.33 cases per 100 000 population every 10 years (95% CI, 0.87-1.80).
Meta-regression coefficients of the influence of several factors on the incidence of multiple sclerosis, in number of cases per 100 000 population. Adjusted and unadjusted analysis.
| Variable | Unadjusted analysis | Adjusted analysisa | ||
|---|---|---|---|---|
| Coefficient | 95% confidence interval | Coefficient | 95% confidence interval | |
| All studies | ||||
| Year (mid-point of estimation period) | 0.13 | 0.10 to 0.17 | 0.14 | 0.11 to 0.18 |
| Latitude | 0.08 | –0.06 to 0.23 | 0.07 | –0.02 to 0.16 |
| Length of estimation period | 0.02 | –0.10 to 0.12 | 0.06 | –0.002 to 0.12 |
| Studies published in journals indexed in MEDLINE | ||||
| Year (mid-point of estimation period) | 0.13 | 0.08 to 0.18 | 0.14 | 0.10 to 0.19 |
| Latitude | 0.09 | –0.10 to 0.28 | 0.09 | –0.03 to 0.21 |
| Length of estimation period | 0.02 | –0.11 to 0.16 | 0.06 | –0.02 to 0.14 |
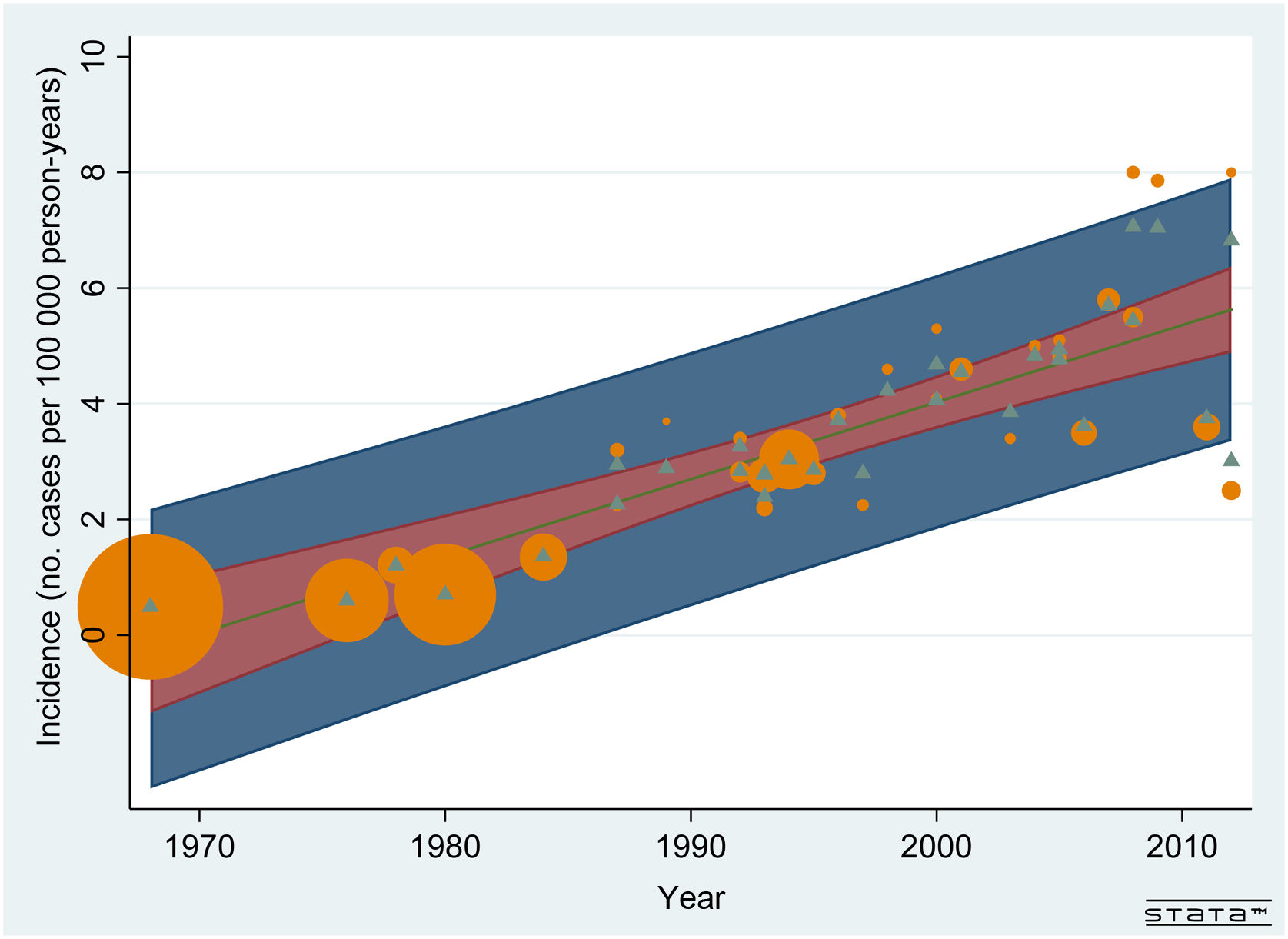
Fig. 5 shows the plot for the unadjusted meta-regression analysis of the incidence of MS over time. This association showed an I2 of 90% and an adjusted R2 of 69%.
Meta-regression analysis of the impact of time on the incidence of multiple sclerosis. The straight line reflects the predicted incidence rate by year (mid-point of the estimation period), the red area reflects the 95% confidence interval, and the dark blue area reflects the prediction interval. Orange circles indicate the observed incidence rates (size is inversely proportional to total variance), while green triangles reflect empirical Bayes estimates (ie, the predicted incidence rates of the random effects).
Regarding latitude, the year-adjusted analysis showed an increase in the incidence rate of 0.87 cases per 100 000 person-years with every 10° increment in latitude (95% CI, –0.005 to 1.75); in the year-adjusted analysis of articles from journals indexed in MEDLINE, incidence increased by 1.08 cases per 100 000 with every 10° increment (95% CI, –0.12 to 2.28).
We were unable to conduct a meta-regression analysis of age at symptom onset as a function of the study year as few studies reported the standard deviation of mean age at symptom onset. The mean age at symptom onset was 31.14 years (range, 27.3-36.10), and the median age was 31.25 years (Q1-Q3, 29.37-32.37). We performed a simple linear regression analysis of the relationship between age at symptom onset and year, and found a slight increase in age in more recent years, although with a negative lower bound of the 95% CI (linear regression coefficient: 0.09; 95% CI, –0.02 to 0.16).
A simple linear regression analysis was also performed for sex ratio and year (median: 2.09; range, 1.1-3.29; Q1-Q3, 1.68-2.5). The female-to-male ratio barely increased over time (linear regression coefficient: 0.0043; 95% CI, –0.0123 to 0.0210).
DiscussionThis systematic review of prevalence and incidence studies conducted in Spain revealed a clear increase in the prevalence and incidence of MS over the years, as well as a trend toward a positive correlation between latitude and prevalence/incidence.
This increase in prevalence rates may be due to multiple factors. Firstly, the number of detected cases has increased, which in turn results in fewer undiagnosed cases. The number of sources for case detection has also increased. However, it has been hypothesised that prevalence studies still fail to include all existing cases; this idea is further supported by the great number of records gathered from MS registries of neurology departments, while some studies have suggested the use of capture-recapture methods to achieve more complete estimates.46,69
Secondly, improvements in diagnosis associated with the use of MRI and CSF analysis and updates in the diagnostic criteria for MS70–72 have increased the number of detected cases, including some patients who would not have been diagnosed with older criteria. Thirdly, the development of new pharmacological treatments has favoured the referral of suspected cases to neurology departments. Furthermore, the development and consolidation of the Spanish National Health System and the greater predisposition of the public to seek medical care may have also resulted in greater likelihood of patients with such neurological conditions as MS, which presents with relatively mild symptoms in early stages, consulting with their physician. These phenomena are reflected both in a marked decrease in diagnostic delay73 and in a decrease in median Expanded Disability Status Scale score74 in prevalent cases over time.47
Lastly, the increased prevalence of MS is largely due to the fact that the mortality rate associated with the disease is lower than the incidence rate, despite the latter remaining stable. Prevalence comprises the set of all new and pre-existing cases of a condition (excluding cured or deceased patients). As MS is a chronic disease with a very low short-term mortality, its prevalence will necessarily increase over time as long as its incidence is higher than the associated mortality. In any case, survival may have increased with the introduction of disease-modifying treatments.75
The extent to which a real increase in the incidence of MS in Spain has contributed to the increase in its prevalence is unclear. The heterogeneity of results, however, suggests that case detection may have been incomplete on many occasions.
The increase in incidence rates over time should be interpreted with caution, since the association does not necessarily imply causation. Improvements in the methodological quality of the studies, with greater diagnostic certainty of new cases (in line with the aforementioned changes in diagnostic and treatment criteria and greater patient awareness of the need to seek medical attention) may explain the greater numbers of cases detected in more recent studies, in the absence of a real increase in the incidence of MS. However, we cannot rule out the hypothesis that the observed increase in the incidence of MS is real.
Researchers from the Biomedical Research Networking Centre on Neurodegenerative Diseases and the applied epidemiology section of the Spanish National Centre for Epidemiology, in collaboration with other authors, have recently published a systematic review of studies into the incidence of MS in the European Economic Area.73 This review included 2 studies conducted in Spain (in lower Aragon and Alcoy), which provide serial determinations of the incidence of MS over time. These studies revealed a huge fluctuation in the number of cases per 100 000 person-years, rather than a homogeneous, increasing trend, probably due to the small number of new cases. In Spain, prevalence studies focusing on relatively small areas (30 000-100 000 inhabitants) have been extremely fruitful, as they were able to perform more exhaustive tracking of cases. However, the size of these populations is insufficient to obtain stable rates for incidence studies, a crucial tool for identifying environmental factors potentially linked to the aetiology of the disease. In the rest of Europe, 2 distinct patterns are observed: an increase in incidence in Northern European countries until the mid-1980s, with a subsequent decrease, and a sustained increase in Italy and Greece, with the latter starting at lower incidence rates.73
Other European studies have reported diverging results. The results of the systematic review by Kingwell et al.6 are inconclusive, since the included studies were highly heterogeneous in terms of diagnostic criteria and definition of validated cases, and lacked standardised results. Our study also observed considerable methodological differences; data synthesis with such techniques as meta-analysis is therefore not recommended. A more recent study including data from a Danish registry did find a marked increase in the incidence of MS in women over the last 50 years (114%), especially at older ages, whereas incidence in men increased only slightly (30%).76 This study benefits from the strengths of multiple sclerosis registries, which unify diagnostic criteria, standardise procedures, and provide extremely valuable information for evaluating temporal trends.
We found a trend toward an association between prevalence/incidence and latitude; however, after considering the year of the study (mid-point of the estimation period), we can neither confirm nor rule out Kurtzke’s hypothesis,5 since the confidence intervals are very imprecise, though estimators are positive. Further studies with greater statistical power should aim to clarify this issue, given the relatively small difference in prevalence and incidence rates between extreme latitudes in Spain.
Our study has a number of limitations. Firstly, we did not adjust rates using a standard population; this may have biased the comparison between regions with different age distributions (for instance, the Canary Islands and Andalusia have younger populations than those of Galicia and Castile-Leon). Some prevalence studies gave detailed data by sex and age group, but this was not the case for incidence studies. Secondly, we did not perform a formal assessment of study quality with a view to performing the corresponding sensitivity analyses. Although a number of validated instruments have been developed for quality assessment of randomised controlled trials and analytical observational studies, such as the Grading of Recommendations Assessment, Development and Evaluation tool,77 no similar tools exist for incidence and prevalence studies due to the difficulty of evaluating them. The instrument used by Kingwell et al.6 was specifically designed for their study; therefore, it is not validated and its content is relatively inconsistent and of unclear applicability.
One of the strengths of our study is its comprehensiveness, as it includes nearly every study published on the topic, as well as evidence from some unpublished studies. Furthermore, it uses the methods of systematic reviews, although these are less developed for incidence and prevalence studies.
Despite the difficulty of drawing clear conclusions on the temporal trends of prevalence and, especially, incidence rates, our study reveals the existence of a vast network of research groups focusing on MS, which play an essential role in the organisation of healthcare, resource allocation, and the development of aetiological studies. This network may be integrated into a cooperative structure seeking to unify the criteria for case detection and perform a thorough search of all existing cases in the population of interest. This will surely shed light on the real prevalence and incidence of MS and its geographical and temporal variability.
FundingThis study has received funding from Biogen Idec, S. L.
Conflicts of interestThe authors have no conflicts of interest to declare.