Tension-type headache is the most common primary headache, with a high prevalence and a considerable socioeconomic impact. Manual physical therapy techniques are widely used in the clinical field to treat the symptoms associated with tension-type headache. This systematic review aims to determine the effectiveness of manual and non-invasive therapies in the treatment of patients with tension-type headache.
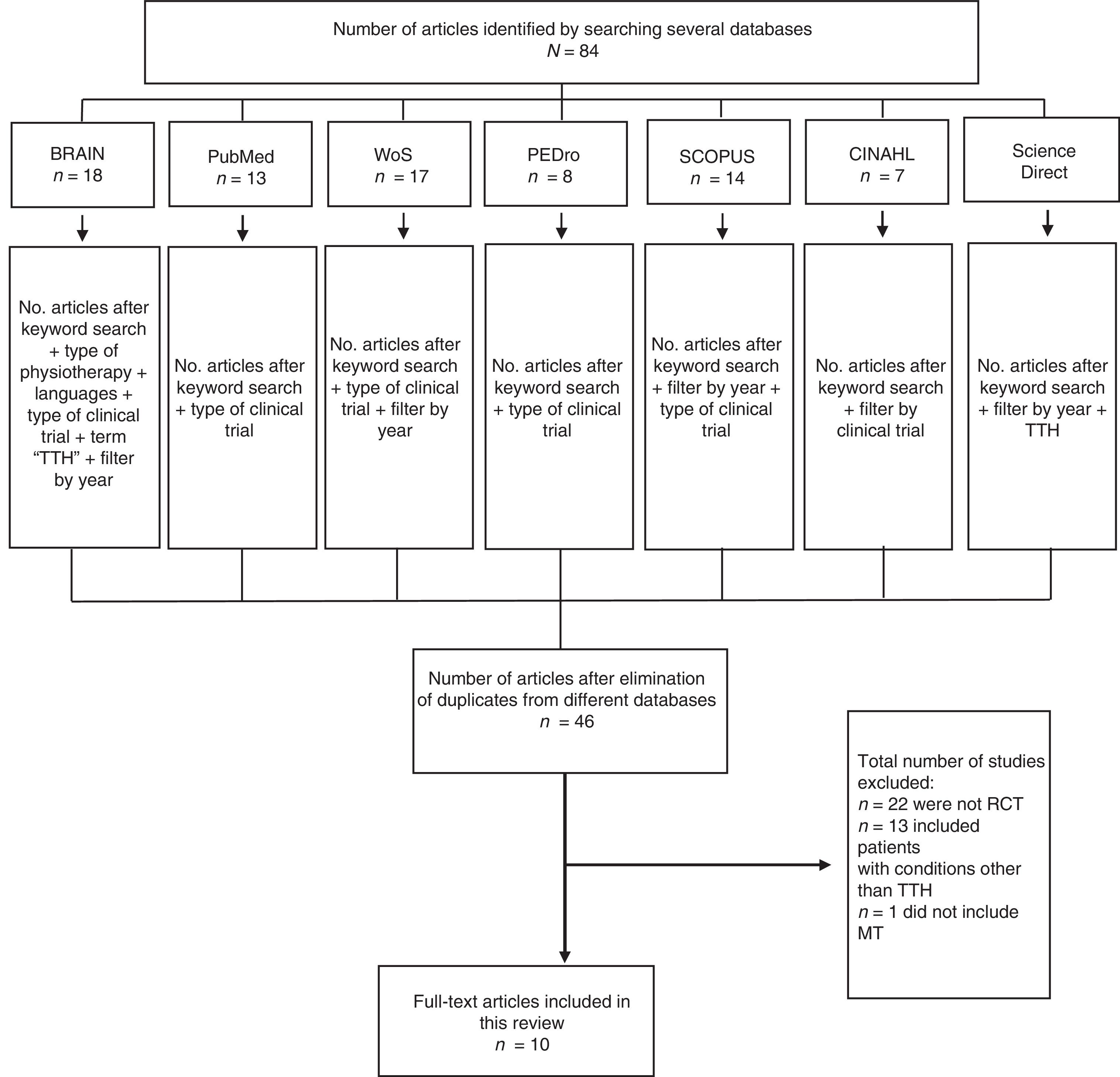
DevelopmentWe conducted a systematic review of randomised controlled trials in the following databases: Brain, PubMed, Web of Science, PEDro, Scopus, CINAHL, and Science Direct. Ten randomised controlled trials were included for analysis. According to these studies, manual therapy improves symptoms, increasing patients’ well-being and improving the outcome measures analysed.
ConclusionsManual therapy has positive effects on pain intensity, pain frequency, disability, overall impact, quality of life, and craniocervical range of motion in adults with tension-type headache. None of the techniques was found to be superior to the others; combining different techniques seems to be the most effective approach.
La cefalea tensional es la cefalea primaria más usual, con una prevalencia elevada y unas consecuencias socioeconómicas de gran impacto. Las técnicas de terapia manual, desde la fisioterapia, son muy utilizadas en el abordaje del conjunto de síntomas que puede provocar. El propósito fue realizar una revisión sistemática sobre la efectividad de las terapias manuales y no invasivas en el tratamiento de pacientes que presentan cefalea tensional en sus actuales formas.
DesarrolloSe llevó a cabo una revisión sistemática de la literatura en busca de ensayos controlados y aleatorizados. Se emplearon las siguientes bases de datos: Brain, PubMed, Web of Science, PEDro, Scopus, CINHAL y Science Direct. Se analizaron 10 estudios, todos ellos ensayos controlados y aleatorizados. Según los estudios individuales, la intervención logra mejorar la clínica, aportando bienestar al paciente y mejorando las distintas medidas de resultado analizadas.
ConclusionesLa terapia manual logra efectos positivos sobre la intensidad y la frecuencia del dolor, la discapacidad, el impacto, la calidad de vida y el rango de movimiento craneocervical en adultos con cefalea tensional. No se encuentra superioridad entre una técnica con respecto a otra, siendo más efectivo el tratamiento combinado de estas.
Tension-type headache (TTH) is defined as oppressive, holocranial pain with few accompanying symptoms. TTH is the most prevalent primary headache.1
Episodic TTH (ETTH) may become chronic as a consequence of the central sensitisation caused by prolonged nociceptive stimulation in myofascial tissues.2–5 Some authors believe that peripheral sensitisation is the main cause of ETTH, whereas chronic TTH (CTTH) may be caused by central sensitisation.5,6
The efficacy of manual therapy (MT) in TTH seems evident. Numerous studies have found it to be effective in reducing headache frequency, intensity, and duration, with a positive influence on quality of life, disability, and cervical range of motion.7–15
To date, several reviews have been conducted on the use of MT for TTH, the most recent dating from 20166; however, the most recent study included in this review is from 2012. In another review from 2014, all trials included were published prior to 2011.16 Some studies also include subjects with migraine and neck pain.17 Another review published in 2015 only included studies comparing MT with pharmacological treatment; furthermore, it only considered pain intensity, frequency, and duration as outcome measures.18 Another review, published in 2010, studied other pathological entities in addition to TTH, and therefore did not address in detail specific questions on this condition.19 Finally, several reviews20,21 have exclusively focused on MT with vertebral manipulation. Therefore, there is a need for an updated systematic review specifically addressing the effects of MT on TTH.
The aim of this systematic review is to assess the effectiveness of non-invasive MT in the treatment of patients with different types of TTH.
DevelopmentInclusion and exclusion criteriaWe included studies meeting the following criteria: randomised clinical trials (RCT) including participants aged between 18 and 65 years and diagnosed with TTH according to the International Headache Society criteria.22,23
We searched for trials comparing interventions with joint mobilisations or physical therapy,8,14,24 vertebral manipulation,9,10,12,13,25 soft tissue techniques,8–10,12,13,15,24,25 cranial techniques,26 or neurodynamic techniques15 to a control group. Regarding outcome measures, we included studies assessing any of the following variables with their main assessment instruments: pain frequency with a headache diary8,12–15; pain intensity with the visual analogue scale,8,12–15,26 pressure algometry,8,15,24 the Headache Index,24,26 and the McGill Pain Questionnaire12; disability with the Headache Disability Index (HDI)8,10,13; quality of life with the Short Form-36 Health Survey14 and the Short Form-12 Health Survey9,25; cervical range of motion with the Cervical Range of Motion Device8,12,13 and goniometric measurements24; impact of headache on daily life with the Headache Impact Test (HIT-6)8,13,15; and such other outcome measures as presence of photophobia10 or phonophobia,10 self-perceived improvement,8 and psychological aspects of pain (Multidimensional Headache Locus of Control).14
Exclusion criteria were as follows: (1) TTH was associated with some mechanical disorder, such as neck or shoulder pain; (2) patients with other types of headache (migraine, cervicogenic headache, etc.) were included; and (3) study assessed invasive physiotherapy and pharmacological treatment interventions.
Search strategyThe search was conducted from September to November 2016. We selected studies published in English or Spanish between 2000 and 2016. We searched the Brain, PubMed, Web of Science, PEDro, Scopus, CINAHL, and ScienceDirect databases, using the following search strategy: (1) “tension-type headache”; (2) “manual therapy”; and (3) “tension-type headache” AND “manual therapy.”
Review methodologyStudies were selected on the basis of the title and abstracts obtained in the electronic searches; full texts of potentially relevant studies were reviewed by 2 reviewers. After identifying the articles meeting our inclusion criteria, we assessed their methodological quality with the CASP guidelines27,28 for clinical trials; the Oxford scale29 was used to specify the level of evidence and degree of recommendation. We used the PRISMA guidelines30 to assess the quality of reviews.
ResultsDescription of studiesOf the 84 studies identified, we excluded 38 duplicate studies and 36 studies that did not meet the inclusion criteria (Fig. 1).2,17,31–41,16,42–62 Data were extracted from 10 articles (Table 1):
- -
Five studies (240 participants) compared suboccipital soft tissue inhibition with articulatory technique and occiput–atlas–axis global manipulation, the combination of both techniques, and a control group.9,10,12,13,25
- -
One study (97 participants) compared soft tissue techniques with neuromobilisations, a combination of both, and placebo superficial massage.15
- -
One study (35 participants) compared soft tissue techniques with Cyriax's vertebral mobilisation.24
- -
One study (81 participants) compared craniocervical flexion exercises with a latex band combined with conventional physiotherapy techniques including massage techniques with frictions; mobilisations based on the Maitland® method and cervical, dorsal, and lumbar-pelvic posture retraining; and a control group undergoing conventional physiotherapy.14
- -
One study (82 participants) compared MT techniques, exercises, and posture retraining to usual care by the general practitioner.8
- -
One study (60 participants) compared the resting supine position to the CV-4 technique and a control group.26
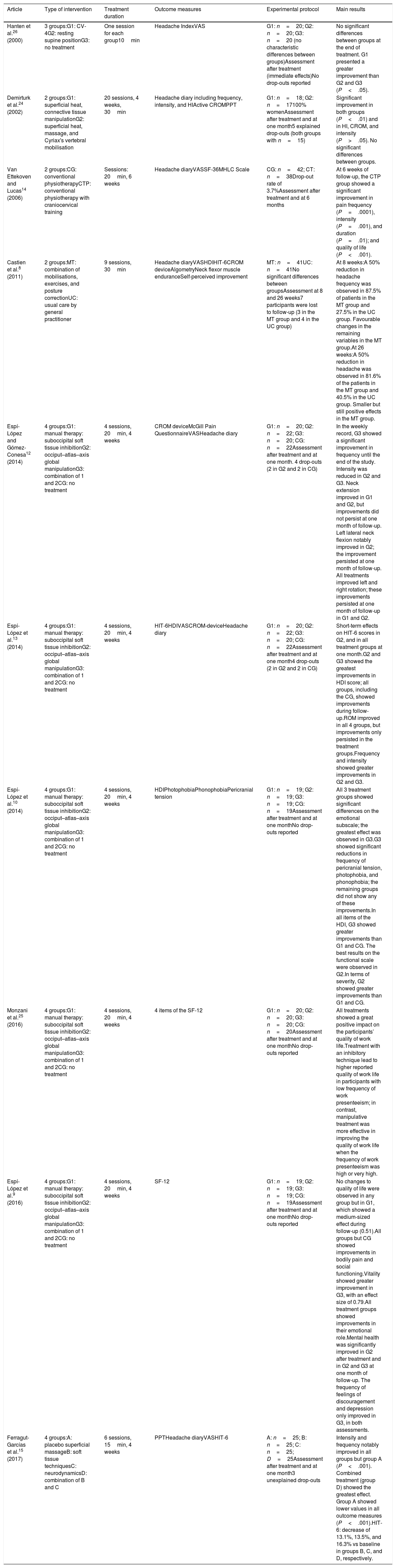
Summary of the study results.
| Article | Type of intervention | Treatment duration | Outcome measures | Experimental protocol | Main results |
|---|---|---|---|---|---|
| Hanten et al.26 (2000) | 3 groups:G1: CV-4G2: resting supine positionG3: no treatment | One session for each group10min | Headache IndexVAS | G1: n=20; G2: n=20; G3: n=20 (no characteristic differences between groups)Assessment after treatment (immediate effects)No drop-outs reported | No significant differences between groups at the end of treatment. G1 presented a greater improvement than G2 and G3 (P<.05). |
| Demirturk et al.24 (2002) | 2 groups:G1: superficial heat, connective tissue manipulationG2: superficial heat, massage, and Cyriax's vertebral mobilisation | 20 sessions, 4 weeks, 30min | Headache diary including frequency, intensity, and HIActive CROMPPT | G1: n=18; G2: n=17100% womenAssessment after treatment and at one month5 explained drop-outs (both groups with n=15) | Significant improvement in both groups (P<.01) and in HI, CROM, and intensity (P>.05). No significant differences between groups. |
| Van Ettekoven and Lucas14 (2006) | 2 groups:CG: conventional physiotherapyCTP: conventional physiotherapy with craniocervical training | Sessions: 20min, 6 weeks | Headache diaryVASSF-36MHLC Scale | CG: n=42; CT: n=38Drop-out rate of 3.7%Assessment after treatment and at 6 months | At 6 weeks of follow-up, the CTP group showed a significant improvement in pain frequency (P=.0001), intensity (P=.001), and duration (P=.01); and quality of life (P<.001). |
| Castien et al.8 (2011) | 2 groups:MT: combination of mobilisations, exercises, and posture correctionUC: usual care by general practitioner | 9 sessions, 30min | Headache diaryVASHDIHIT-6CROM deviceAlgometryNeck flexor muscle enduranceSelf-perceived improvement | MT: n=41UC: n=41No significant differences between groupsAssessment at 8 and 26 weeks7 participants were lost to follow-up (3 in the MT group and 4 in the UC group) | At 8 weeks:A 50% reduction in headache frequency was observed in 87.5% of patients in the MT group and 27.5% in the UC group. Favourable changes in the remaining variables in the MT group.At 26 weeks:A 50% reduction in headache was observed in 81.6% of the patients in the MT group and 40.5% in the UC group. Smaller but still positive effects in the MT group. |
| Espí-López and Gómez-Conesa12 (2014) | 4 groups:G1: manual therapy: suboccipital soft tissue inhibitionG2: occiput–atlas–axis global manipulationG3: combination of 1 and 2CG: no treatment | 4 sessions, 20min, 4 weeks | CROM deviceMcGill Pain QuestionnaireVASHeadache diary | G1: n=20; G2: n=22; G3: n=20; CG: n=22Assessment after treatment and at one month. 4 drop-outs (2 in G2 and 2 in CG) | In the weekly record, G3 showed a significant improvement in frequency until the end of the study. Intensity was reduced in G2 and G3. Neck extension improved in G1 and G2, but improvements did not persist at one month of follow-up. Left lateral neck flexion notably improved in G2; the improvement persisted at one month of follow-up. All treatments improved left and right rotation; these improvements persisted at one month of follow-up in G1 and G2. |
| Espí-López et al.13 (2014) | 4 groups:G1: manual therapy: suboccipital soft tissue inhibitionG2: occiput–atlas–axis global manipulationG3: combination of 1 and 2CG: no treatment | 4 sessions, 20min, 4 weeks | HIT-6HDIVASCROM-deviceHeadache diary | G1: n=20; G2: n=22; G3: n=20; CG: n=22Assessment after treatment and at one month4 drop-outs (2 in G2 and 2 in CG) | Short-term effects on HIT-6 scores in G2, and in all treatment groups at one month.G2 and G3 showed the greatest improvements in HDI score; all groups, including the CG, showed improvements during follow-up.ROM improved in all 4 groups, but improvements only persisted in the treatment groups.Frequency and intensity showed greater improvements in G2 and G3. |
| Espí-López et al.10 (2014) | 4 groups:G1: manual therapy: suboccipital soft tissue inhibitionG2: occiput–atlas–axis global manipulationG3: combination of 1 and 2CG: no treatment | 4 sessions, 20min, 4 weeks | HDIPhotophobiaPhonophobiaPericranial tension | G1: n=19; G2: n=19; G3: n=19; CG: n=19Assessment after treatment and at one monthNo drop-outs reported | All 3 treatment groups showed significant differences on the emotional subscale; the greatest effect was observed in G3.G3 showed significant reductions in frequency of pericranial tension, photophobia, and phonophobia; the remaining groups did not show any of these improvements.In all items of the HDI, G3 showed greater improvements than G1 and CG. The best results on the functional scale were observed in G2.In terms of severity, G2 showed greater improvements than G1 and CG. |
| Monzani et al.25 (2016) | 4 groups:G1: manual therapy: suboccipital soft tissue inhibitionG2: occiput–atlas–axis global manipulationG3: combination of 1 and 2CG: no treatment | 4 sessions, 20min, 4 weeks | 4 items of the SF-12 | G1: n=20; G2: n=20; G3: n=20; CG: n=20Assessment after treatment and at one monthNo drop-outs reported | All treatments showed a great positive impact on the participants’ quality of work life.Treatment with an inhibitory technique lead to higher reported quality of work life in participants with low frequency of work presenteeism; in contrast, manipulative treatment was more effective in improving the quality of work life when the frequency of work presenteeism was high or very high. |
| Espí-López et al.9 (2016) | 4 groups:G1: manual therapy: suboccipital soft tissue inhibitionG2: occiput–atlas–axis global manipulationG3: combination of 1 and 2CG: no treatment | 4 sessions, 20min, 4 weeks | SF-12 | G1: n=19; G2: n=19; G3: n=19; CG: n=19Assessment after treatment and at one monthNo drop-outs reported | No changes to quality of life were observed in any group but in G1, which showed a medium-sized effect during follow-up (0.51).All groups but CG showed improvements in bodily pain and social functioning.Vitality showed greater improvement in G3, with an effect size of 0.79.All treatment groups showed improvements in their emotional role.Mental health was significantly improved in G2 after treatment and in G2 and G3 at one month of follow-up. The frequency of feelings of discouragement and depression only improved in G3, in both assessments. |
| Ferragut-Garcías et al.15 (2017) | 4 groups:A: placebo superficial massageB: soft tissue techniquesC: neurodynamicsD: combination of B and C | 6 sessions, 15min, 4 weeks | PPTHeadache diaryVASHIT-6 | A: n=25; B: n=25; C: n=25; D=25Assessment after treatment and at one month3 unexplained drop-outs | Intensity and frequency notably improved in all groups but group A (P<.001). Combined treatment (group D) showed the greatest effect. Group A showed lower values in all outcome measures (P<.001).HIT-6: decrease of 13.1%, 13.5%, and 16.3% vs baseline in groups B, C, and D, respectively. |
CG: control group; CROM: cervical range of movement; CV-4: compression of the fourth ventricle; G1: group 1; G2: group 2; G3: group 3; G4: group 4; HDI: Headache Disability Index; HI: Headache Index; HIT-6: Headache Impact Test; MHLC: Multidimensional Headache Locus of Control; MT: manual therapy; PPT: pressure pain threshold; SF-12: Short Form-12 Health Survey; SF-36: Short Form-36 Health Survey; VAS: visual analogue scale.
All studies included participants with TTH, 2 studies included adults with CTTH only,8,24 and the remaining studies included both patients with CTTH and patients with ETTH.9,10,12–15,25,26
Intervention duration was 4 weeks in 7 studies,9,10,12,13,15,24,25 more than 6 weeks in 2,8,14 and only one session in one study.26 Session duration ranged from 10 to 20minutes in 8 studies,9,10,12–15,25,26 and 30minutes in 2 studies.8,24
A third assessment to observe long-term effects was only conducted in 3 studies.8,14,15
Synthesis of resultsThe most widely used outcome measures in the studies reviewed were intensity8,12–15,26 and frequency8,12–15 of TTH. All trials used a headache self-report or diary and the visual analogue scale to measure these variables. Furthermore, several studies also used pressure algometry,8,15,24 the Headache Index,24,26 and the McGill Pain Questionnaire.12 All the studies reported significant improvements after the intervention with regard to the control group. Combined therapy with different MT techniques had a larger effect.12,13,15 A study based on a craniocervical exercise programme showed a significant, long-lasting reduction in frequency and intensity.14
Four studies analysed changes in craniocervical range of motion,8,12,13,24 with 3 using the CROM device8,12,13; results were better in the groups treated with manipulation techniques.12,13
Three studies used the HDI. All treatment groups showed significant improvements in overall HDI scores. Total HDI score showed greater improvements with combined therapy of manipulation techniques plus suboccipital soft tissue inhibition in 2 studies.10,13 In one study, improvements only persisted at 8 weeks in the group that received cervical manipulation.13
Three studies assessed participants’ quality of life using the Short Form-36 Health Survey and its abbreviated version, the Short Form-12 Health Survey (Spanish-language version).63,64 One of these focused on quality of life with regard to professional life,25 using only 4 items from the Short Form-12 Health Survey. The greatest improvement was observed in the group performing craniocervical exercises, posture retraining, and passive mobilisations based on the Maitland® method.14 Quality of life in the professional domain improved especially in the group undergoing soft tissue techniques.
The HIT-6 was used in 3 trials, obtaining statistically significant improvements over baseline values.8,13,15
With regard to secondary outcome measures, one article analysed the presence of photophobia and phonophobia,10 reporting improvements in the group receiving combined therapy of soft tissue inhibition plus cervical manipulation. Self-perceived improvement after treatment was assessed in one study; the MT group showed significant long- and short-term improvement.8 One study14 analysed the psychological aspects of pain using the Multidimensional Headache Locus of Control scale.65,66
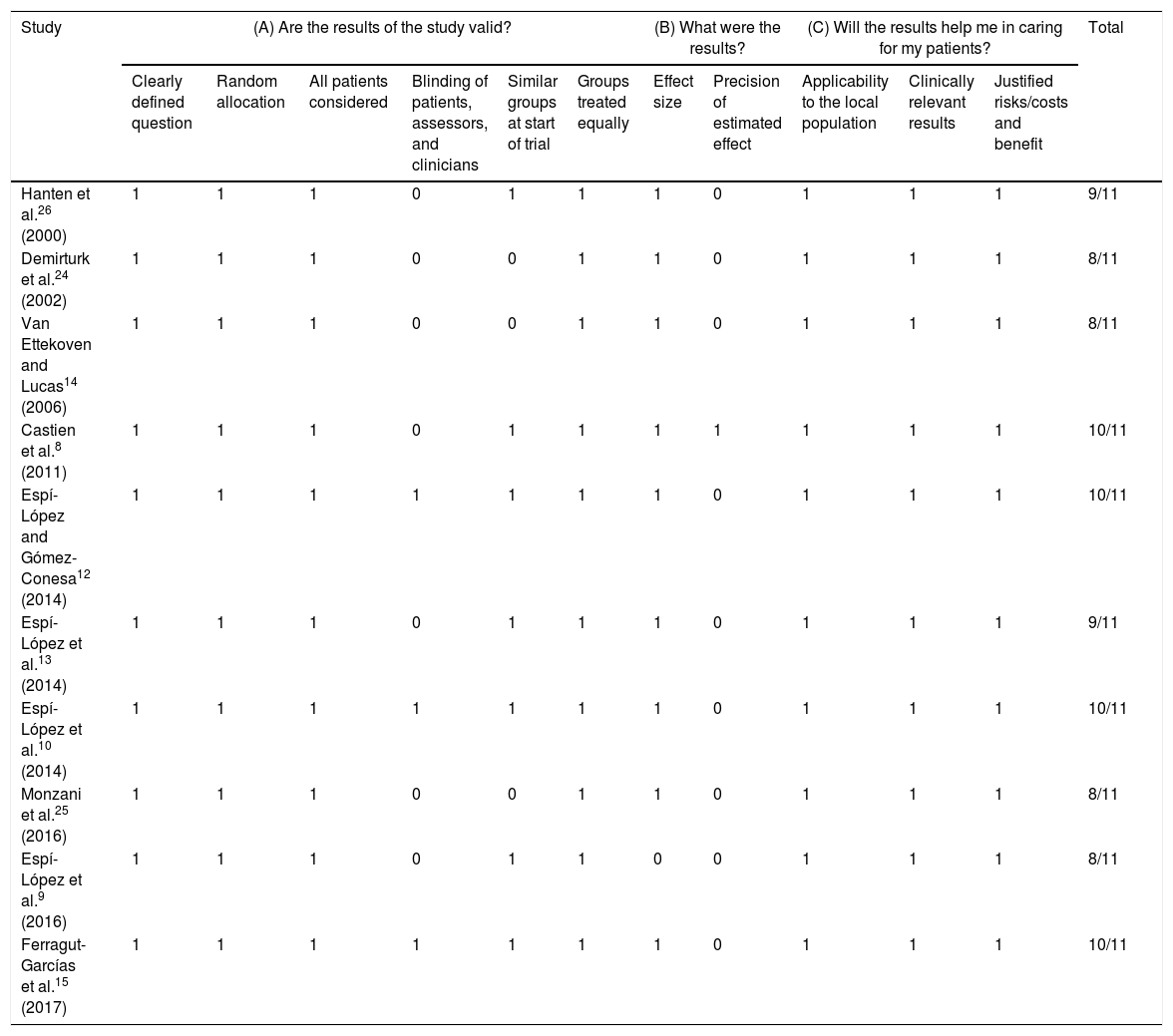
Methodological qualityWe contacted Espí-López9,10,12,13,25 and Oliva-Pascual-Vaca15 to clarify some issues related to the blinding of therapists12,13 and the participant selection process9,10,12,13 in order to assess methodological quality. Only the first author provided the requested information.
All studies scored between 8 and 10 in the CASP guidelines (Table 2). The Oxford scale was used to assess both the level of evidence and the degree of recommendation. All studies were classified with a level of evidence 2B, with the exception of one, which was classified 1B.
CASP scale.
| Study | (A) Are the results of the study valid? | (B) What were the results? | (C) Will the results help me in caring for my patients? | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clearly defined question | Random allocation | All patients considered | Blinding of patients, assessors, and clinicians | Similar groups at start of trial | Groups treated equally | Effect size | Precision of estimated effect | Applicability to the local population | Clinically relevant results | Justified risks/costs and benefit | ||
| Hanten et al.26 (2000) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 9/11 |
| Demirturk et al.24 (2002) | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 8/11 |
| Van Ettekoven and Lucas14 (2006) | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 8/11 |
| Castien et al.8 (2011) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10/11 |
| Espí-López and Gómez-Conesa12 (2014) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 10/11 |
| Espí-López et al.13 (2014) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 9/11 |
| Espí-López et al.10 (2014) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 10/11 |
| Monzani et al.25 (2016) | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 8/11 |
| Espí-López et al.9 (2016) | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 8/11 |
| Ferragut-Garcías et al.15 (2017) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 10/11 |
0=no; 1=yes.
Regarding drop-outs, 2 studies reported no drop-outs9,10 and there were explained drop-outs in 312,13,24 and unexplained drop-outs in another 3 studies.8,14,15 Finally, no mention was made of drop-outs in 2 studies.25,26
DiscussionThe aim of this systematic review was to assess the effectiveness of MT in patients with TTH by gathering and critically analysing RCTs.
All the studies analysed show positive results in patients receiving physiotherapy with MT. This review only includes patients diagnosed with TTH according to the International Headache Society criteria.
All but one24 of the studies used an adequate sample size (≥60 participants). However, methodological flaws were present in several studies, justifying cautious interpretation of the results. Firstly, only 3 trials were considered double-blind12,13,15; no blinding is mentioned or only participants were blinded in the remaining studies. Secondly, only one study8 calculated confidence intervals to determine the precision of the effect on the clinical findings. Another important consideration was the similarity of the groups at the beginning of the study: 2 trials did not describe the groups,25,26 which may have led to a confounding effect, for instance sex differences: some authors have found that women present a better response to physiotherapy than do men, and that patients with CTTH respond better than those with ETTH.67
In terms of outcome measures, most studies reported improved scores on the visual analogue scale.8,12–15,26 All studies assessing headache frequency reported significant improvements. It should be noted that 3 studies analysing the disability caused by TTH showed significant improvements in the HDI, which has good psychometric properties in the study of headache.68,69 The Spanish version of the tool70 was used in one study.13
Quality of life improved significantly with treatments including a craniocervical exercise programme,14 as reflected in changes in the Short Form-36 Health Survey score.71 Significant improvements were also observed in the HIT-6 (which assesses the impact of headache on the patient's work or daily activities)72 in the 3 studies that used it.8,13,15
We established the presence of photophobia and phonophobia as secondary outcome measures, given the importance of assessing these symptoms; however, only one study included them.12
After analysing the experimental protocols used in the studies, we can conclude that the dose of MT was very heterogeneous. Treatment duration in all studies ranged from 10 to 30minutes for 4–6 weeks. Other systematic reviews recommend sessions of 30–45minutes every 7–10 days.6 In most of the studies, follow-up and assessment only consisted of a pre- and post-treatment examination; few studies included a third analysis.8,14,15
According to the findings of the studies reviewed, manipulation therapy might be more useful for gaining mobility in the neck, and improving disability indices and pain frequency. Soft tissue treatment achieved a greater improvement in the impact and intensity of pain. Most studies agreed that groups undergoing any combined therapy based on MT showed greater improvements than those receiving the different techniques separately.10,12,13,15 Considering the information from the studies analysed, we believe that one effective treatment would consist of the combination of soft tissue techniques and structural techniques, in addition to craniocervical flexion exercises.
In line with previous reviews,6,16,18–21,48 the studies analysed report that changes after MT are clinically significant. However, further studies of high methodological quality are needed to demonstrate the effectiveness of MT in improving quality of life and decreasing the disability caused by TTH.
This review presents several limitations. Some can be attributed to the samples used in some studies, since after contacting the lead author, we discovered that 2 studies included the same participants12,13; another 2 studies also used a single sample.9,10 Furthermore, there may be studies published in other languages, which we have not included.
ConclusionsPhysiotherapy treatment based on MT achieves positive outcomes in pain intensity and frequency, disability, impact of headache, quality of life, and craniocervical range of motion in adults with TTH. Although the results show a clinical improvement, there is no clear evidence that any one technique is superior to another; the combination of both techniques is the most effective treatment.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cumplido-Trasmonte C, Fernández-González P, Alguacil-Diego IM, Molina-Rueda F. Terapia manual en adultos con cefalea tensional: revisión sistemática. Neurología. 2019. https://doi.org/10.1016/j.nrl.2017.12.004