Dementia units (DU) provide comprehensive and specialised care to patients with dementia. However, assessment in these units normally focuses on patient management. The aim of this study was to determine satisfaction of the caregivers of patients managed in a DU and how they rated DU care.
MethodsWe created a self-administered questionnaire which was completed by 236 caregivers visiting the DU in 2015. The questionnaire included 6 dimensions (accessibility, organisation, professionalism, relationship with staff, information, and facilities); data were analysed using problem rates.
ResultsA total of 53.4% caregivers completed the questionnaire; most were women, patients’ spouses, or first-degree relatives. The overall problem rates was 15.0% (95% CI, 13.9-16.1), with sizeable differences between dimensions: from 0.1% (95% CI, 0.0-0.4) for ‘relationship with staff’ and ‘professionalism’ to 49.3% (95% CI, 45.4-53.2) for ‘information’. Waiting times over 30minutes were perceived as excessive. Information problems were not directly related to patient management. Satisfaction was scored 8.29/10 (median 8; SD 1.45); 77.3% (95% CI, 69.8-74.8) of respondents were highly satisfied. Ninety-nine percent of the caregivers stated that they would recommend the DU.
ConclusionsThis questionnaire provides interesting data on care quality as perceived by patients’ caregivers. Our results have allowed us to identify problems and implement corrective actions. Our questionnaire has proved to be a useful tool for evaluating and improving care quality in DUs.
Las unidades de demencia (UD) realizan un abordaje integral y especializado de las personas con demencia. Su evaluación suele limitarse a aspectos asistenciales. El objetivo del trabajo fue conocer la satisfacción y calidad percibida por familiares/cuidadores de pacientes atendidos por una UD.
MétodosEncuesta autocumplimentada con cuestionario de elaboración propia a 236 acompañantes de pacientes ya conocidos en la UD durante 2015, estructurada en 6 dimensiones (accesibilidad, organización, profesionalidad, trato, información e infraestructura) y analizada mediante tasas de problemas.
ResultadosTasa de respuesta de 53,4%, resultando la mayoría mujeres, cónyuges o familiares de primer grado de los pacientes. La tasa de problemas global fue 15,0% (IC 95%: 13,9-16,1), con amplias variaciones por dimensión: desde 0,1% (IC 95%: 0,0-0,4) en «trato» y «profesionalidad» hasta 49,3% (IC 95%: 45,4-53,2) en «información». La espera se percibe excesiva a partir de 30min. Los problemas de información se centraron en actividades no directamente asistenciales. La satisfacción fue 8,29/10 (mediana 8; DE: 1,45) con 77,3% (IC 95%: 69,8-74,8) de puntuaciones excelentes. El 99% recomendarían la UD.
ConclusionesEl cuestionario ha ofrecido una visión global de la calidad percibida por los familiares/cuidadores de los pacientes atendidos, y permitido identificar y priorizar dónde implantar acciones correctoras. Ha demostrado ser una herramienta útil para evaluar y mejorar la calidad asistencial en las UD.
Population ageing has caused an increase in the incidence of such age-related diseases as dementia. Dementia is a clinical syndrome of variable aetiology, characterised by persistent impairment of higher mental functions, which results in poorer social and work performance in people with no alterations in the level of consciousness.1 In Spain, the prevalence of dementia in people aged over 65 ranges between 4% and 16%.2–4 The condition is the leading cause of disability and death among this age group, incurring considerable costs for the healthcare system.5
In response to this problem, dementia units have been created in many hospitals. These multidisciplinary teams provide comprehensive, specialised care to patients with dementia in a defined geographic area. In addition to diagnosing dementia and providing care to these patients, dementia units also address social, training, research, and management issues and establish alliances with universities, pharmaceutical companies, and institutions funding basic, clinical, and social research on dementia (healthcare, social, and community issues).6,7 However, assessment of these units has traditionally focused exclusively on health care.7,8 Very few studies have evaluated satisfaction with and perceived quality of the healthcare services offered; published evidence on this subject in our setting is anecdotal.9–11The west Murcia Area I dementia unit (UDAIMO) was created in 2002. Since 2015, the unit has adopted process-based management to reorient its activity towards meeting the needs and expectations of patients and their families. The information drawn from process follow-up is used to improve quality.12 Learning about relatives’ and caregivers’ opinions of our activity has, therefore, become a priority. This study aims to analyse satisfaction and the perceptions of the quality of the service among relatives and caregivers of the patients attended at a dementia unit.
Material and methodsThe UDAIMO, based at Hospital Clínico Universitario Virgen de la Arrixaca, Murcia, is the reference unit for the Region of Murcia. This multidisciplinary team provides high-quality, ethical, comprehensive dementia care, aiming to improve the quality of life of these patients and their families. The unit serves nearly 2500 patients annually, 500 of whom are new diagnoses.
As the patients attended at the unit have cognitive impairment, we decided to administer the perceived quality and satisfaction questionnaire to the patients’ relatives or caregivers accompanying them to their appointments at the UDAIMO. To create the questionnaire, we used the structure of the Health Service of Murcia's perceived quality questionnaire for the process “external consultation,” which has been validated by the Department of Health and Social Affairs of the Region of Murcia.13 The questionnaire mainly enquires about a specific experience, asking about the occurrence of objective circumstances or objective details previously identified by qualitative research (focus groups) and which have an impact on the informant's satisfaction. Based on the above, and with a view to adapting the questionnaire to the situation of the UDAIMO, our hospital's care quality unit proposed eliminating irrelevant questions and including questions deemed to be necessary in the light of the characteristics of the recently created care process. These questions enquired about the professionalism and attitude of specific members of the UDAIMO team (e.g. the neuropsychologist), their interest in the patient's preferences and values, and the information provided on the unit's activities. To help informants identify team members, we provided a definition for each role based on the activities that they usually perform with patients or their companions.
The final set of questions (in addition to questionnaire structure and question formulation) was assessed with cognitive pretesting and agreed on by the UDAIMO team. The final questionnaire, which is available on-line, includes 30 questions grouped into 6 dimensions (accessibility, professionalism, attitude, organisation, information, and infrastructure), and enquired about global satisfaction and fidelity.12
The study population comprised the companions of known patients attended at our unit. Participants had to meet 3 inclusion criteria: being the companions of patients who had previously visited the unit, visiting the UDAIMO during the study period, and agreeing to complete the questionnaire. We therefore excluded the companions of new patients (first appointment) and those not wishing to complete the questionnaire.
We used convenience sampling during a one-month period (June 2015) to gather a maximum of 150 completed questionnaires. Upon arrival at the unit, the administrative assistant or the nursing assistant explained the purpose of the questionnaire to patients’ companions and invited them to participate. Companions who volunteered to participate were given a copy of the questionnaire and a pen, and were asked to complete it while at the UDAIMO. Once completed, the questionnaire was placed inside a box provided for that purpose. No further copies of the questionnaire were issued once we had gathered 150 completed questionnaires.
Each questionnaire dimension was expressed as a rate of problems, a composite indicator summarising the percentage of undesired responses to the different aspects of each dimension (closed-ended questions, nearly all of them dichotomous or 5-point Likert-type). The weight of each aspect on the final rates was assessed using a Pareto chart. The 6 dimensions of the questionnaire were summarised as a global rate of problems. An 11-point Likert scale (scores 0 to 10) was used to measure satisfaction; these results were used to calculate mean satisfaction and the percentage of excellent scores (8 points and above). Fidelity was expressed as the percentage of affirmative answers to the question “Would you recommend our dementia unit to your family or friends?”. Results were broken down by sex, age (≤50 years or >50 years), time attending the UDAIMO (≤1 year or >1 year), and level of education (no studies/primary studies vs. secondary studies/further education). Depending on the type of variable, differences were analysed with the chi-square test, the t test, or the Mann–Whitney U test, with statistical significance set at P<.05.
The questionnaire also included an open-ended question asking which single aspect of the UDAIMO should be improved; answers to this question were categorised according to the questionnaire dimensions.
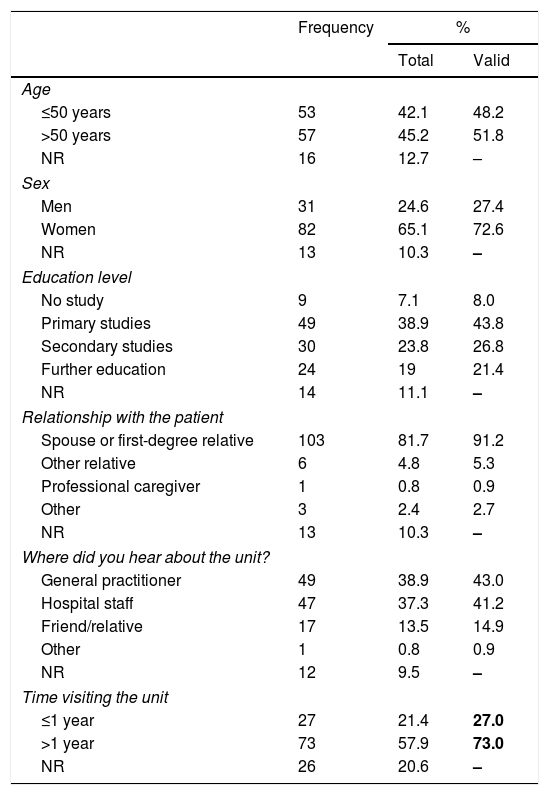
ResultsDuring the study period, we attended a total of 236 known patients (repeat visitors), whose companions were invited to participate. We gathered a total of 126 completed questionnaires; this translates into a response rate of 53.4%. The study methodology does not allow us to offer segmented data. Most respondents were women and were patients’ spouses or first-degree relatives. Respondents had a mean age of 52.7±12.1 years (range, 27-82). Table 1 summarises the main characteristics of survey respondents.
Classification of survey respondents.
| Frequency | % | ||
|---|---|---|---|
| Total | Valid | ||
| Age | |||
| ≤50 years | 53 | 42.1 | 48.2 |
| >50 years | 57 | 45.2 | 51.8 |
| NR | 16 | 12.7 | – |
| Sex | |||
| Men | 31 | 24.6 | 27.4 |
| Women | 82 | 65.1 | 72.6 |
| NR | 13 | 10.3 | – |
| Education level | |||
| No study | 9 | 7.1 | 8.0 |
| Primary studies | 49 | 38.9 | 43.8 |
| Secondary studies | 30 | 23.8 | 26.8 |
| Further education | 24 | 19 | 21.4 |
| NR | 14 | 11.1 | – |
| Relationship with the patient | |||
| Spouse or first-degree relative | 103 | 81.7 | 91.2 |
| Other relative | 6 | 4.8 | 5.3 |
| Professional caregiver | 1 | 0.8 | 0.9 |
| Other | 3 | 2.4 | 2.7 |
| NR | 13 | 10.3 | – |
| Where did you hear about the unit? | |||
| General practitioner | 49 | 38.9 | 43.0 |
| Hospital staff | 47 | 37.3 | 41.2 |
| Friend/relative | 17 | 13.5 | 14.9 |
| Other | 1 | 0.8 | 0.9 |
| NR | 12 | 9.5 | – |
| Time visiting the unit | |||
| ≤1 year | 27 | 21.4 | 27.0 |
| >1 year | 73 | 57.9 | 73.0 |
| NR | 26 | 20.6 | – |
NR: no response.
The percentage of valid responses excludes participants not responding to the item in question.
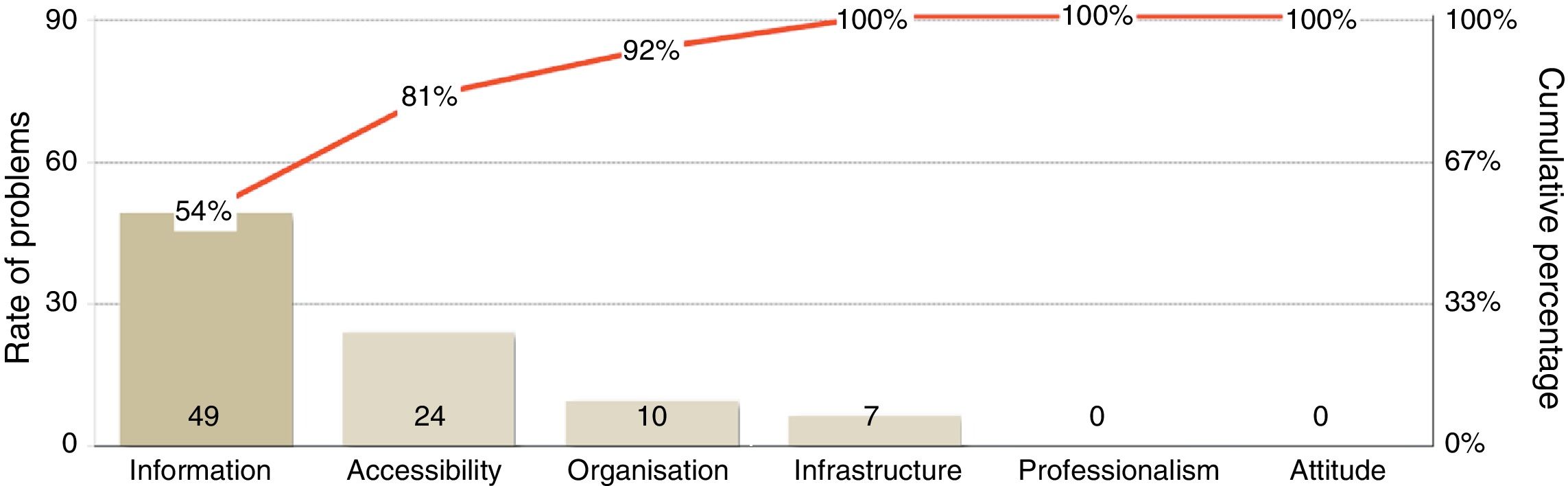
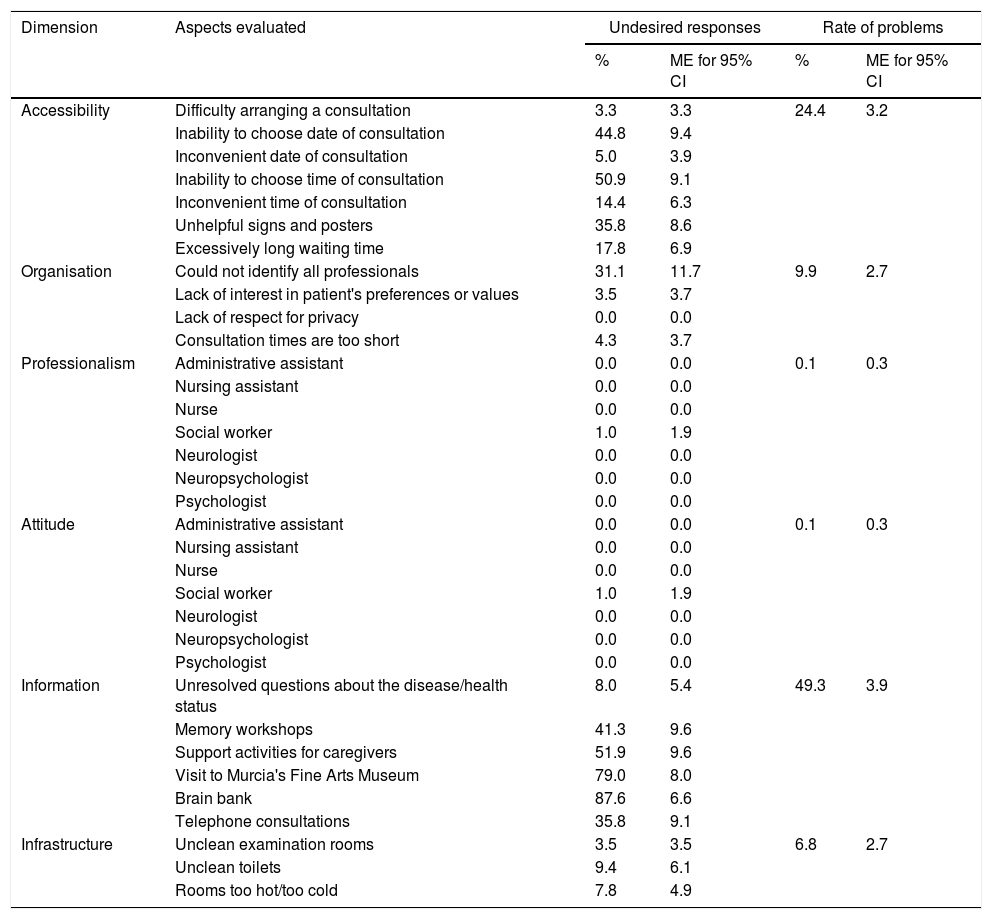
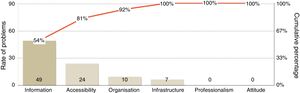
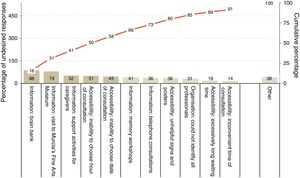
The global rate of problems was 15.0% (95% CI, 13.9-16.1), and was significantly higher among companions of patients who had been attended at the UDAIMO for less than a year (19.5%±2.6% vs. 14.1%±1.4%, P<.001). The rate of problems showed marked variations between dimensions, ranging from 0.1% for attitude and professionalism to 49.3% for information (Table 2 and Fig. 1). The rate of problems in the dimension “information” was also higher among companions of patients who had visited the unit for less than a year (66.4%±7.7% vs. 44.4%±4.9%, P<.0001). No differences were detected in any of the remaining dimensions for any of the variables analysed.
Percentage of undesired responses and rates of problems for each dimension.
| Dimension | Aspects evaluated | Undesired responses | Rate of problems | ||
|---|---|---|---|---|---|
| % | ME for 95% CI | % | ME for 95% CI | ||
| Accessibility | Difficulty arranging a consultation | 3.3 | 3.3 | 24.4 | 3.2 |
| Inability to choose date of consultation | 44.8 | 9.4 | |||
| Inconvenient date of consultation | 5.0 | 3.9 | |||
| Inability to choose time of consultation | 50.9 | 9.1 | |||
| Inconvenient time of consultation | 14.4 | 6.3 | |||
| Unhelpful signs and posters | 35.8 | 8.6 | |||
| Excessively long waiting time | 17.8 | 6.9 | |||
| Organisation | Could not identify all professionals | 31.1 | 11.7 | 9.9 | 2.7 |
| Lack of interest in patient's preferences or values | 3.5 | 3.7 | |||
| Lack of respect for privacy | 0.0 | 0.0 | |||
| Consultation times are too short | 4.3 | 3.7 | |||
| Professionalism | Administrative assistant | 0.0 | 0.0 | 0.1 | 0.3 |
| Nursing assistant | 0.0 | 0.0 | |||
| Nurse | 0.0 | 0.0 | |||
| Social worker | 1.0 | 1.9 | |||
| Neurologist | 0.0 | 0.0 | |||
| Neuropsychologist | 0.0 | 0.0 | |||
| Psychologist | 0.0 | 0.0 | |||
| Attitude | Administrative assistant | 0.0 | 0.0 | 0.1 | 0.3 |
| Nursing assistant | 0.0 | 0.0 | |||
| Nurse | 0.0 | 0.0 | |||
| Social worker | 1.0 | 1.9 | |||
| Neurologist | 0.0 | 0.0 | |||
| Neuropsychologist | 0.0 | 0.0 | |||
| Psychologist | 0.0 | 0.0 | |||
| Information | Unresolved questions about the disease/health status | 8.0 | 5.4 | 49.3 | 3.9 |
| Memory workshops | 41.3 | 9.6 | |||
| Support activities for caregivers | 51.9 | 9.6 | |||
| Visit to Murcia's Fine Arts Museum | 79.0 | 8.0 | |||
| Brain bank | 87.6 | 6.6 | |||
| Telephone consultations | 35.8 | 9.1 | |||
| Infrastructure | Unclean examination rooms | 3.5 | 3.5 | 6.8 | 2.7 |
| Unclean toilets | 9.4 | 6.1 | |||
| Rooms too hot/too cold | 7.8 | 4.9 | |||
ME for 95% CI: margin of error for a 95% confidence interval.
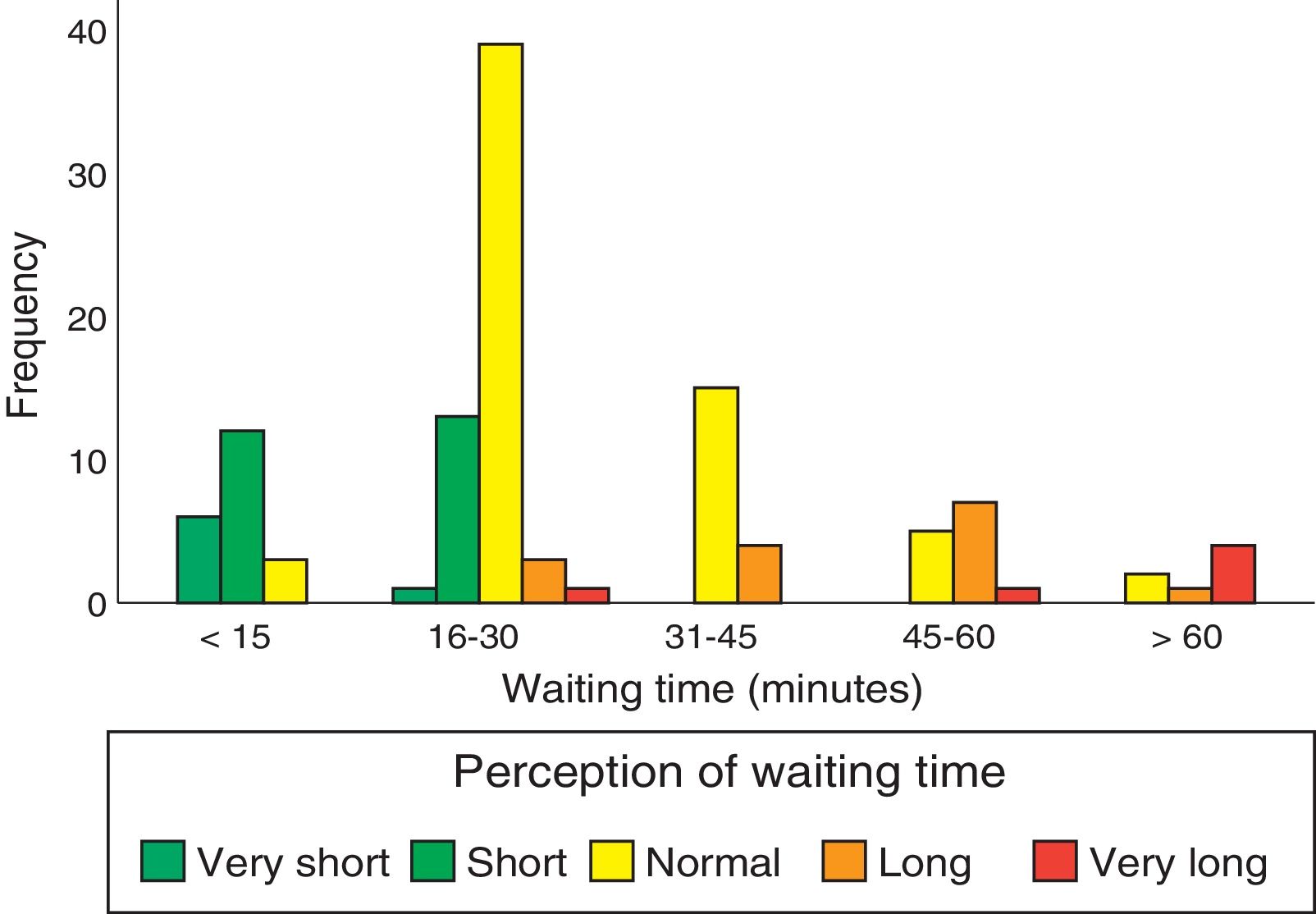
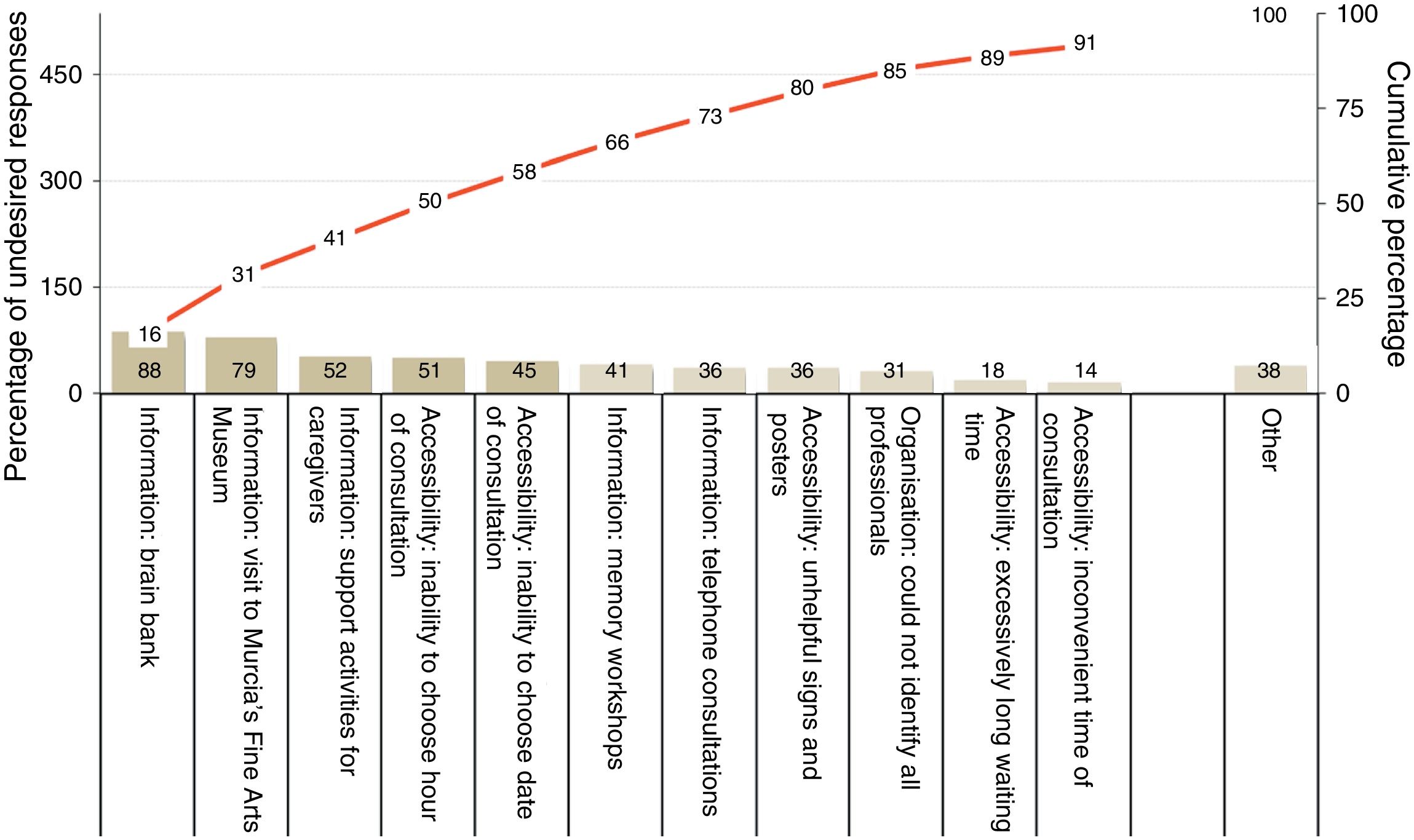
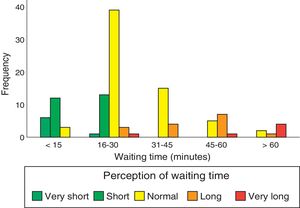
Regarding undesired responses (Table 2), inability to choose the date and time of consultations constitutes the main problem of accessibility. Regarding waiting times, 34% of patients had to wait for longer than 30minutes, although 18% had to wait for less than 15minutes. Waiting time was perceived as excessively long when it exceeded 30minutes (Fig. 2). The main organisational problem was informants being unable to identify all the types of professionals working at the UDAIMO, although only 4% of respondents reported not knowing any of the staff. The most relevant information problems involved activities not directly related to care, such as the existence of a brain bank, the visit to the fine arts museum (a guided tour to promote and/or preserve cognitive abilities through art and culture, and to promote social integration), and support activities for caregivers. Only 8% (95% CI, 2.6-13.4) reported having unresolved doubts about the disease or the patient's health status. Fig. 3 shows the main undesired responses and the dimension to which they belong.
Satisfaction was similar between groups; respondents scored a mean of 8.29 points (median, 8; SD, 1.45; SE, 0.13), with a 77.3% (95% CI, 69.8-74.8) rate of excellent scores. The question as to whether the respondent would recommend the unit to their relatives or friends was answered by 118 of the 126 survey respondents; 99% answered “yes” or “probably.” Only one respondent would not recommend the unit.
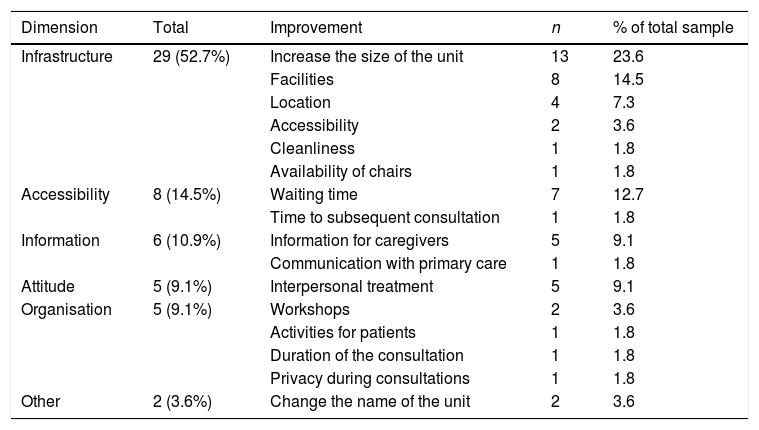
The question enquiring about which single aspect of the unit should be improved was completed by 69 respondents (55%); 14 of these (20%) indicated that there was nothing to improve. The remaining respondents suggested improvements in infrastructure (52.7%: size and condition of the unit, etc.), accessibility (14.5%), information (10.9%), organisation of activities (9.1%), and staff attitude (9.1%) (Table 3).
Responses to the open-ended question “In your experience, if you had to choose a single aspect of the dementia unit that should be improved, what would it be?”, broken down by dimension.
| Dimension | Total | Improvement | n | % of total sample |
|---|---|---|---|---|
| Infrastructure | 29 (52.7%) | Increase the size of the unit | 13 | 23.6 |
| Facilities | 8 | 14.5 | ||
| Location | 4 | 7.3 | ||
| Accessibility | 2 | 3.6 | ||
| Cleanliness | 1 | 1.8 | ||
| Availability of chairs | 1 | 1.8 | ||
| Accessibility | 8 (14.5%) | Waiting time | 7 | 12.7 |
| Time to subsequent consultation | 1 | 1.8 | ||
| Information | 6 (10.9%) | Information for caregivers | 5 | 9.1 |
| Communication with primary care | 1 | 1.8 | ||
| Attitude | 5 (9.1%) | Interpersonal treatment | 5 | 9.1 |
| Organisation | 5 (9.1%) | Workshops | 2 | 3.6 |
| Activities for patients | 1 | 1.8 | ||
| Duration of the consultation | 1 | 1.8 | ||
| Privacy during consultations | 1 | 1.8 | ||
| Other | 2 (3.6%) | Change the name of the unit | 2 | 3.6 |
The questionnaire provided data on perceived quality, satisfaction, and fidelity of the caregivers or relatives of patients attended at the UDAIMO. We should bear in mind that the results obtained may be influenced by a number of factors. Although the questionnaire underwent pretesting and is an adaptation of another questionnaire which is validated in this setting,13 it is not itself a validated questionnaire. Furthermore, convenience sampling does not allow us to generalise our results. The response rate, though greater than 50% and higher than usual for the Health Service of Murcia,13 may have led to a selection bias; we attempted to control this by stratifying the results. The nature of some items of the questionnaire (especially those referring to professionalism, attitude, and information, which enquire about long-term contact with the UDAIMO) and the method for completing and gathering the questionnaires (i.e. during the consultation) prevent us from knowing respondents’ perception of quality during the first consultation. In spite of the above, our results allowed us to build indicators to clearly identify which areas should be improved in order to increase patient satisfaction and the perceived quality of the UDAIMO. The questionnaire may inform the continuous improvement involved in process-based management.14
The main problems detected involve the dimension “information.” This is consistent with the results of other studies, using semi-structured interviews, which have shown that information and communication problems are those which most commonly affect the care provided to patients with cognitive impairment.15,16 The most prevalent information problems were linked to UDAIMO activities that are rarely offered during first-ever consultations12 (for example, the brain bank or museum visit [Fig. 3]); this explains why these problems are more common among the relatives or caregivers of patients who have attended the UDAIMO for a shorter time. We should also mention the lack of information on the availability of telephone consultations, an important service at dementia units.9 Although telephone consultations are better known than the other activities, this factor may have had a negative impact on perceived accessibility, which we address later in the article. These results have led us to develop specific improvements in our unit.
Inability to choose the date and time of consultation is the main problem of accessibility, and points to the need to change the scheduling system. Once at the UDAIMO, waiting times are considered excessively long when they exceed 30minutes (Fig. 2); this was the case for one-third of patients, although 18% waited less than 15minutes to be attended. The UDAIMO has implemented a strategy of directing patients to different professionals according to availability, rather than in a fixed order.
The professionalism and attitude of staff are highly valued by the relatives and caregivers of these patients.16 We found nearly no problems in these 2 dimensions; this is directly correlated with the high levels of satisfaction, fidelity, and the low global rate of problems in our sample. In line with the importance of conscientious care and recognition of the patient as a person for quality care,17 the UDAIMO explicitly mentions “treating patients appropriately” and “considering patients’ and caregivers’ preferences” among its principles.12 These principles are part of all the unit's activities and procedures and contribute to the positive results observed.
The participants’ responses point to the need to improve the unit's infrastructure (size and condition of the space, number of staff, etc.); although these measures cannot be implemented internally, they should be brought to the management's attention in order to be properly addressed.
In summary, our survey not only provided a general overview of the relatives’ and caregivers’ perception of quality, but also helped identify and prioritise opportunities for improvement with a moderate need for resources, which are achievable by a great majority of dementia units in our setting. While we should not forget the importance of such instruments as focus groups and other tools that are more difficult to implement,15 the current lack of specific alternatives in the context of dementia care makes this questionnaire a useful tool for continuous improvement. Further studies should aim to improve this tool through validation and application in other contexts.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: López-Picazo JJ, de Dios Cánovas-García J, Antúnez C, Marín J, Antequera MM, Vivancos L, et al. Calidad percibida en una unidad de demencias: el portavoz del paciente como proveedor de información. Neurología. 2018;33:570–576.