Trauma is the most frequent cause of posterior interosseous nerve palsy (the continuation of the deep branch of the radial nerve). Non-traumatic causes are infrequent. The literature reports cases of posterior interosseous nerve compression by such extraneural soft tissue masses as lipomas, rheumatoid nodules, ganglia, or myxomas.1,2 We present the case of a patient with a history of rheumatic disease and progressive radial nerve palsy.
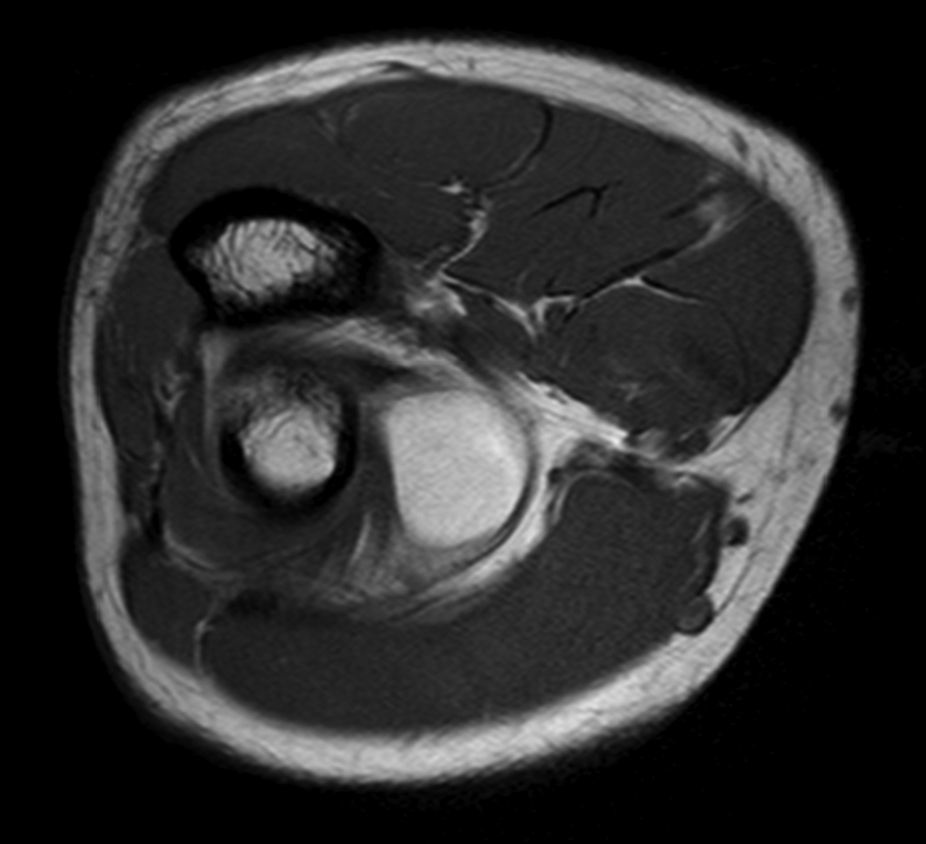
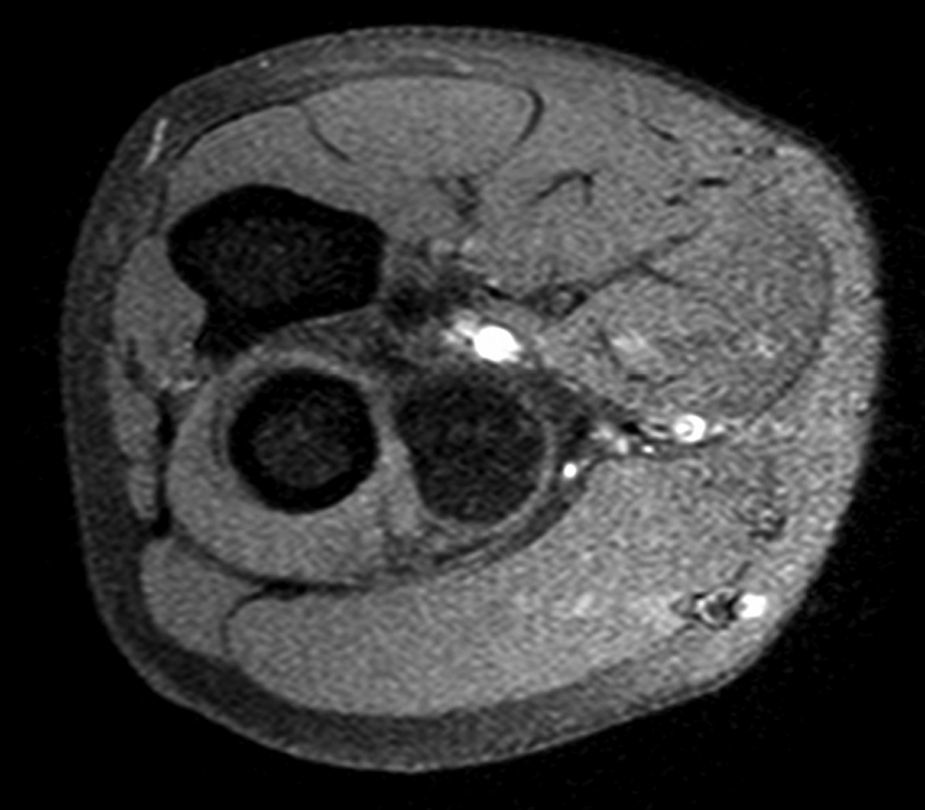
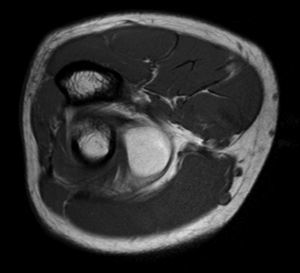
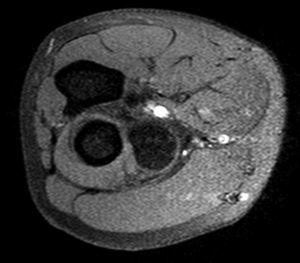
The patient, a 40-year-old man with SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis, and osteitis), came to our hospital with a one-month history of inability to extend the right thumb and index fingers. He reported no trauma and did not work in a high-risk occupation. The neurological examination revealed inability to extend the right thumb and index fingers, with no other neurological deficits or lesions to the right upper limb. An electromyography (EMG) study found a subacute axonal lesion to the radial nerve, predominantly affecting the posterior compartment (posterior interosseous nerve), at the level of the proximal part of the arm. Nerve entrapment was suspected. An MRI scan showed a tumor surrounding the neck of the radius and measuring approximately 4×3×2cm; the mass was hyperintense on T1 and hypointense on STIR, suggesting a fatty origin (Figs. 1 and 2). The patient underwent nerve decompression surgery; the tumor was removed and both branches of the radial nerve were released. The anatomical pathology study of the resected mass revealed lipoma. A follow-up EMG conducted 6 months after surgery revealed no conduction anomalies at the level of the radial nerve. After a year of rehabilitation, the patient achieved nearly full recovery from the initial deficits. Right upper limb function was assessed with the QuickDASH and Jamar® questionnaires.
Lipomas are benign tumors, usually located in subcutaneous cellular tissue; however, they may also appear in deeper tissues, compressing adjacent structures. Lipomas are an infrequent cause of posterior interosseous nerve palsy. This occurrence was first described in 1953 by Richmond, in a 62-year-old painter. Two further cases were subsequently reported by Hustead in 1958. To date, only around 40 cases of posterior interosseous nerve palsy caused by a lipoma have been described in the literature.1,3,4 Lipomas causing peripheral nerve compression are most commonly located at the level of the femur, radius, and tibia.3,4 Posterior interosseous nerve palsy secondary to lipoma usually manifests progressively with inability to extend the hand and fingers, with no associated sensory alterations.5–7 This condition is slightly more common in women and tends to present between the ages of 50 and 80. Symptoms are unpredictable and presence of pain varies from case to case. Lipomas may appear as radiolucency in simple radiography, as described by Richmond.8 EMG studies help confirm clinical suspicion and locate the area of compression. MRI is the technique of choice for evaluating the soft tissues surrounding the nerve. This condition requires surgical treatment; tumor resection must be complete to prevent relapses, as previously reported.6 Early diagnosis and adequate surgical treatment are essential for a good functional outcome.
Conflicts of interestThis study has received no public or private funding. The authors have no conflicts of interest to declare.
Please cite this article as: Flores Robles BJ, Sanz Sanz J, Sanabria Sanchinel AA, Hualde Juvera A. Parálisis del nervio interóseo posterior secundario a lipoma profundo. Neurología. 2017;32:557–558.