Extrapulmonary tuberculosis affects the central nervous system (CNS) in 5%-10% of cases, manifesting with a range of clinical symptoms1: meningitis, hydrocephalus, stroke secondary to vasculitis,2 abscesses, and brain tuberculomas. Spinal epidural abscess is exceptional,3 as is involvement of the cerebral meningeal compartment with simultaneous spinal abscess.
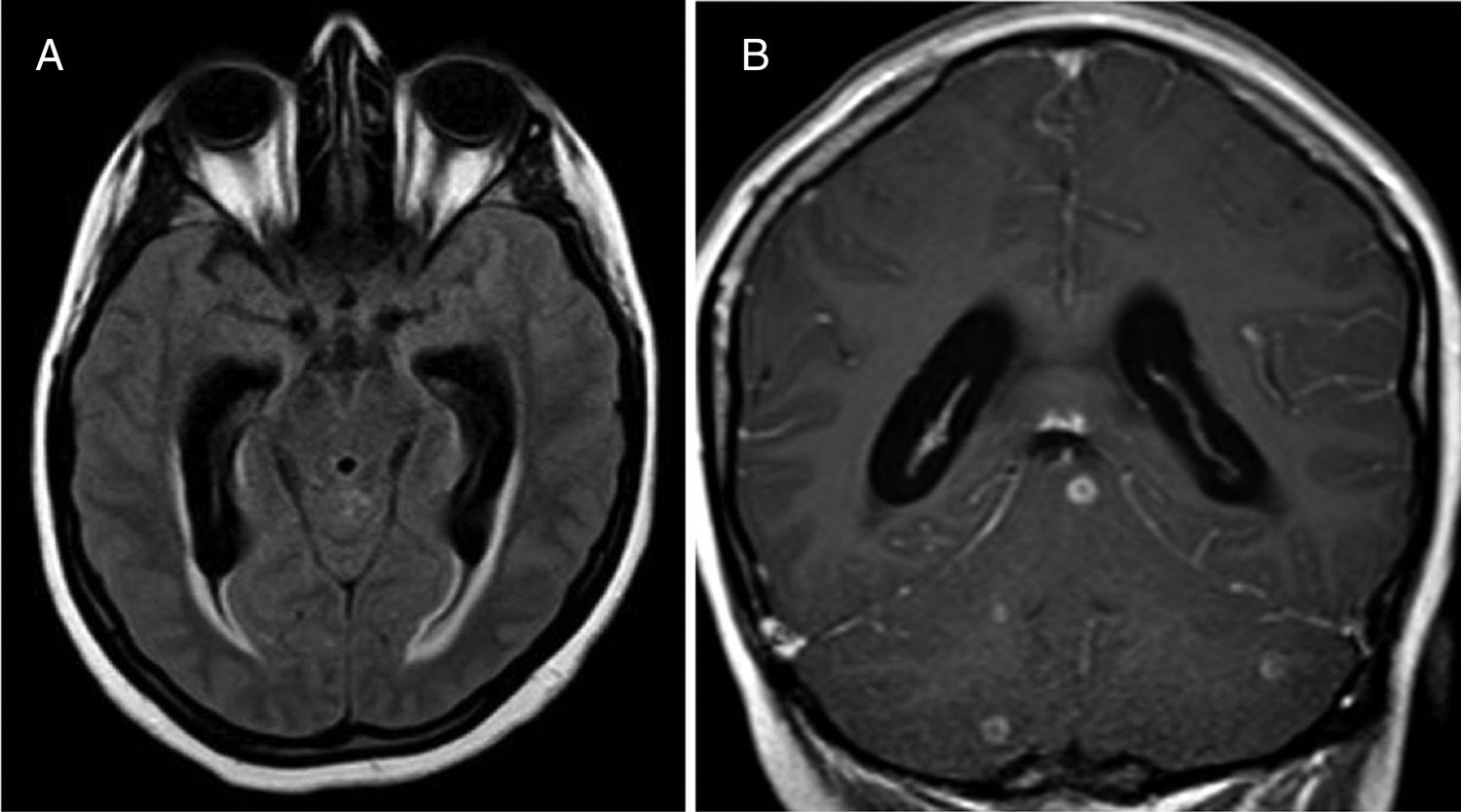
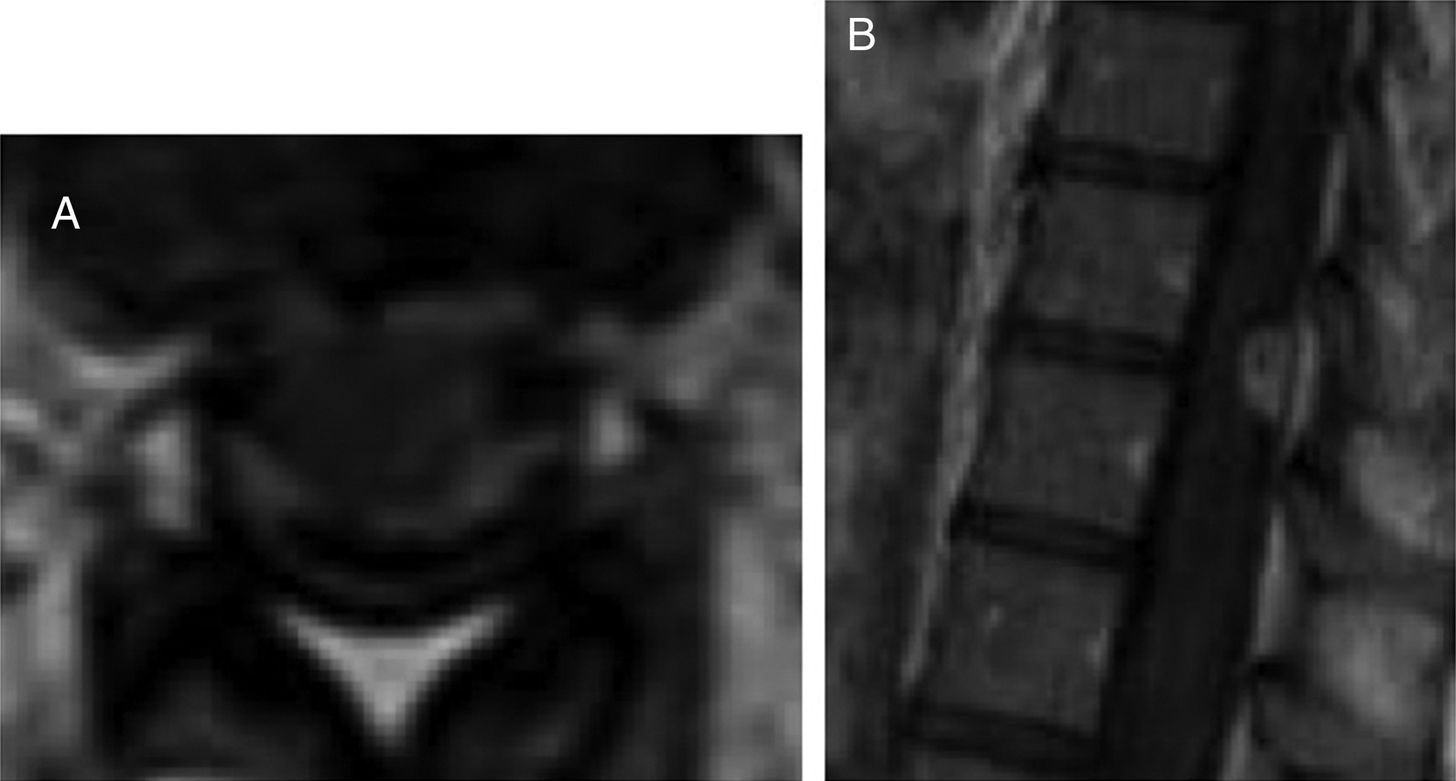
We present the case of a 23-year-old immunocompetent Berber woman who, after a second caesarean section with epidural anaesthesia, presented headache, neck rigidity, and subacute nausea progressing for 2 weeks; fever was not observed. A brain computed tomography scan showed normal findings, but a subsequent lumbar puncture revealed thick cerebrospinal fluid with low glucose levels, lymphocytic pleocytosis, and elevated adenosine deaminase (ADA) activity. A chest radiography revealed no abnormalities. Several hours after starting empirical treatment with tuberculostatic drugs (isoniazid 300 mg + pyrazinamide 1600 mg + rifampicin 600 mg + ethambutol 1100 mg/day, orally) and steroids (dexamethasone 4 mg/8 h), the patient presented neurological impairment with confusional symptoms, paraparesis of the lower limbs and anaesthesia from T10, and urinary retention. Neuroaxial magnetic resonance imaging (MRI) revealed communicating hydrocephalus, brain and spinal meningeal enhancement, posterior fossa tuberculomas, and a spinal extra-axial contrast-enhanced lesion at the T10 level suggestive of epidural abscess (Figs. 1 and 2). We observed no vertebral involvement. The Löwenstein-Jensen medium yielded positive results for Mycobacterium tuberculosis.
The initial tuberculostatic treatment was maintained for 2 months and was later simplified to isoniazid + rifampicin and dexamethasone for one year. The patient progressively recovered mobility and was able to walk unaided at 2 months; brain MRI results were normal at 4 months. At 8 months, neurogenic bladder persisted and clean intermittent catheterisation was required; symptoms resolved at 11 months after treatment onset, and a follow-up MRI showed resolution of the spinal lesion. Treatment was well tolerated.
This is an exceptional case of CNS tuberculosis in an immunocompetent patient, manifesting with initial meningeal symptoms and pronounced neurological impairment possibly associated with a paradoxical response during the onset of tuberculostatic treatment.4,5 We opted for a conservative approach to the spinal abscess. Progression was favourable with prolonged treatment.
Women in the early postpartum period are twice as likely to develop tuberculosis as non-pregnant women.6 Pregnancy suppresses the T-helper type 1 (Th1) proinflammatory response, which may mask symptoms, and increases susceptibility to new infections and tuberculosis reactivation.7 After delivery, Th1 suppression reverts, similarly to the immune reconstitution inflammatory syndrome, and symptoms are exacerbated.8
Please cite this article as: Romero-Imbroda J, Sagrario-Fustero T, Del Canto-Pérez C, Requena-Pou M. Tuberculosis meningoencefálica y espinal tras parto. Neurología. 2020;35:349–350.