Progressive multifocal leukoencephalopathy (PML) is a condition caused by reactivation of the JC virus (JCV) in severely immunodeficient patients, for example, HIV-infected patients or patients treated with immunosuppressants. It affects oligodendrocytes in the central nervous system, causing such neurological symptoms as epileptic seizures, behaviour disorders, motor impairment, and ataxia. Symptoms are progressive. Typical neuroimaging findings include multifocal lesions in subcortical areas, normally with no mass effect or contrast uptake.
Diagnosis is based on clinical or radiological suspicion of the disease combined with detection of JCV DNA in CSF by PCR testing. Definitive diagnosis is reached when JCV DNA or viral proteins are detected in brain tissues. Treatment of immunodeficient patients with PML aims to restore immune system function by either administering antiretroviral treatment or discontinuing immunosuppressive drugs.
However, PML may also affect immunocompetent individuals.
We present the case of a 72-year-old man with no relevant medical history who visited the emergency department due to progressive gait impairment and a 5-month history of visual field alterations.
The physical examination revealed left-sided visual extinction and moderate weakness of the left lower limb. Neuropsychological tests confirmed visual extinction and revealed dyslexia, acalculia, and dysgraphia.
An MRI scan revealed hyperintensities in the right parieto-occipital area as well as in the subcortical area in T2/FLAIR sequences; no contrast uptake or mass effect were seen. The area appeared bright in diffusion-weighted images and no ADC restriction was observed. A spectroscopy study displayed a slight increase in the Cho/NAA ratio and presence of lipids and lactate.
All these findings suggested an infectious or inflammatory aetiology, with neoplasia being less likely. A thorough blood analysis revealed normal results for vitamins, thyroid hormones, and tumour markers, and no HIV infection. The results of a white blood cell count and peripheral blood smear also yielded normal results. A thoracic-abdominal CT scan revealed no signs of neoplasia.
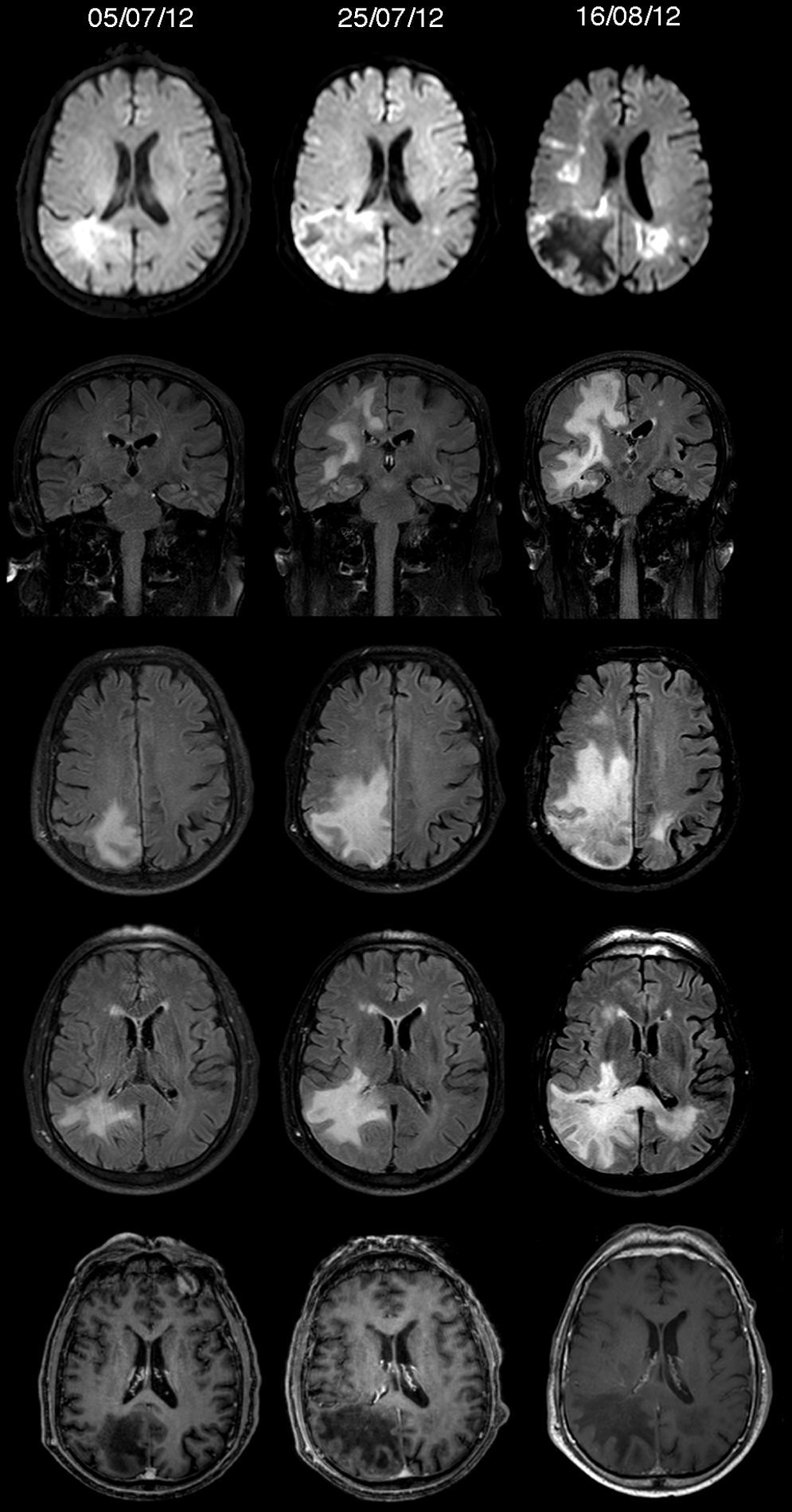
As the patient remained stable and MRI findings were non-specific, we scheduled an additional MRI scan to be performed a few weeks later. However, 2 weeks after discharge, the patient returned to the emergency department due to clinical deterioration, left hemiparesis, and aphasia. An additional MRI scan revealed that the affected area had increased and now extended to the cortical area and corpus callosum (Fig. 1). In light of a suspected inflammatory or infectious process, we decided to perform a lumbar puncture. The CSF analysis revealed slightly increased protein levels (62.2mg/dL; 5leukocytes/mm3, 110erythrocytes/mm3, glucose 72mg/dL), and no oligoclonal bands.
Diffusion-weighted sequences, coronal and axial FLAIR sequences, and gadolinium-enhanced T1-weighted sequences. Timeline of our patient's MR images. The lesion was initially located in the right parieto-occipital area; it was hyperintense on T2/FLAIR sequences, it displayed no contrast uptake or mass effect, and was bright on diffusion-weighted images. In about a month, the lesion progressed from focal to multifocal, affecting the corpus callosum and cortex.
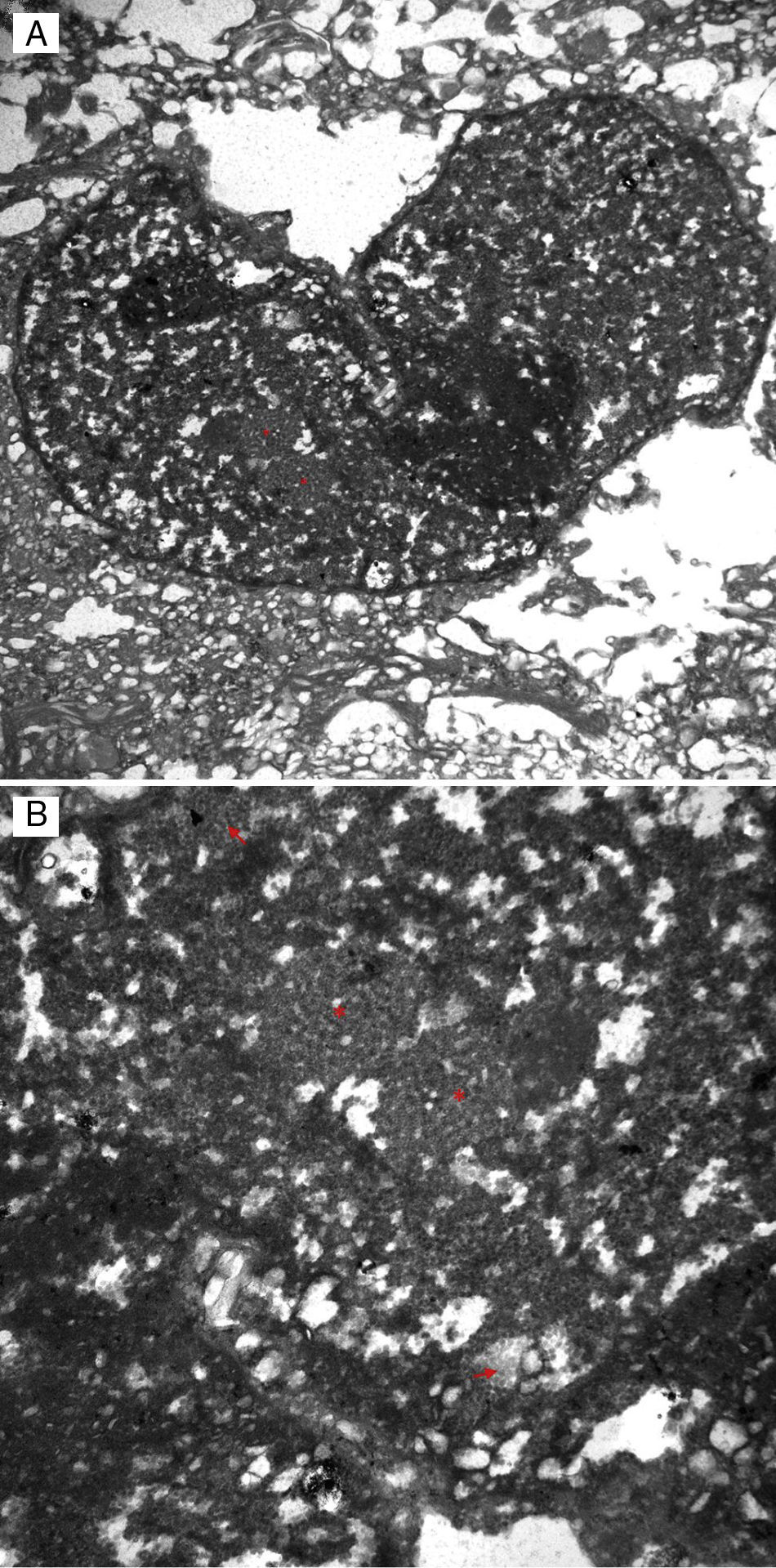
Since both symptoms and the lesion were progressing rapidly, we decided to conduct a brain biopsy, which revealed atypical nuclear inclusions in astrocytes, with proliferation and accumulation of foamy macrophages. An immunohistochemical study showed p53 overexpression and increased expression of SV40 (polyomavirus large T antigen) in astrocytes, as well as viral inclusions displayed by electron microscopy (Fig. 2). These findings were compatible with definitive diagnosis of PML. The PCR study of JCV in CSF yielded 50536copies/mL.
Our patient died a month after diagnosis due to disease progression.
PML is extremely rare in immunocompetent patients. Only 7 cases have been described to date; of these, only 4 were confirmed histologically.1–6 In some of these cases, it was unclear whether immune system imbalances were present. For example, one patient had low levels of IgA, CD8, and natural killer cells; another patient had a hepatitis B infection; and another patient had type 2 diabetes mellitus and low levels of IgG and IgM, and had not been tested for HIV. Of these, only 2 had favourable outcomes: the patient with diabetes mellitus and the one with low levels of IgA.
We present a case of histopathologically confirmed PML with no underlying neoplastic or immunological causes, and no history of other treatments, which presented atypically on MR images. This supports the idea that PML should be included in the differential diagnosis of rapidly progressing white matter lesions, even in immunocompetent patients displaying lesions that are initially focal and affecting cortical areas.
Conflicts of interestThe authors have no conflicts of interest to declare. This study has received no funding of any kind.
Please cite this article as: Muiño E, Rubio MA, Navalpotro I, Munteis E. Leucoencefalopatía multifocal progresiva en un paciente inmunocompetente. Neurología. 2017;32:337–339.