Risk of stroke soon after a transient ischaemic attack (TIA) is high. Urgent care can reduce this risk. Our aim is to describe and evaluate the efficacy of rapid assessment of TIA patients in a hospital without a neurologist available 24h a day.
MethodsIn February 2007, we set up a protocol of rapid management of patients with symptoms consistent with acute TIA, with the aim of prioritising urgent care and reducing hospital admissions, without increasing risk of recurrences. We analyse our results since the protocol was implemented with particular focus on the analysis of delay in neurological and neurovascular assessment, percentage and reasons for hospitalisation, and stroke recurrence rates after 3 months.
ResultsFour hundred and eleven patients were studied, with a final diagnosis of TIA in 282 (68.6%). Among other diagnoses, the most frequent were a vasovagal reaction (5.6%), and a confusional syndrome (4.6%). Delay between emergency arrival and neurovascular assessment was <24h in 82% of cases, and <48h in 93%. After neurological evaluation, 28.7% of the patients were immediately admitted to hospital (most common causes: severe stenosis of a large artery and crescendo TIA). The incidence of ischaemic stroke in TIA patients was 3.55% after 3 months, and 70% of them suffered the recurrence within the first week after the initial TIA.
ConclusionsIn a hospital without a neurologist available 24h a day, an early assessment and management of TIA patients can be carried out in accordance with the guidelines, and may avoid hospitalisation in most cases without increasing recurrence rates.
Los pacientes que presentan un ataque isquémico transitorio (AIT) tienen un alto riesgo de tener un ictus a corto plazo. Una atención urgente puede reducir dicho riesgo. El objetivo es describir y comprobar la eficacia de un protocolo de atención rápida a estos pacientes en un hospital sin guardias de neurología.
MétodosEn febrero del 2007 se puso en marcha en nuestro hospital un protocolo de evaluación rápida del AIT, con el objetivo de priorizar la atención urgente y disminuir ingresos hospitalarios sin aumentar riesgo de recurrencias. Se analizan los resultados tras los primeros 5 años, incidiendo especialmente en los tiempos de valoración neurológica y neurovascular, motivos de ingreso y tasa de recurrencia a los 90 días.
ResultadosHan sido evaluados 411 pacientes, de los cuales 282 (68,6%) fueron finalmente AIT. Entre los otros diagnósticos, los más frecuentes han sido el episodio vasovagal (5,6%) y el cuadro confusional (4,6%). La demora entre la llegada a Urgencias y la valoración del neurólogo fue <24h en el 82% de casos y <48h en el 93,9%. Tras la valoración neurológica, se decidió el ingreso en el 28,7% de pacientes (causas más frecuentes: hallazgos en el Doppler y AIT de repetición). A los 3 meses, 10 pacientes (3,55%) presentaron un ictus, 7 de ellos (70%) en la primera semana desde el episodio.
ConclusionesEn un hospital sin guardias de neurología, es posible una evaluación rápida de los pacientes con AIT, de acuerdo con las recomendaciones de las guías, evitando la mayoría de ingresos y con un bajo índice de recurrencias.
Transient ischaemic attack (TIA) is a focal neurological deficit of ischaemic origin that resolves spontaneously in less than 24hours, and usually in less than 1hour.1 While these events may seem benign, the risk of stroke in a patient who has experienced TIA may be as high as 20% in the following 3 months, and the risk is especially high in the first few days after the episode.2–5 For these reasons, TIA is regarded as a medical emergency, and considerable efforts have been made in recent years to reduce the accompanying risk of stroke. The main goals have been to identify and offer early treatment to those patients at the most risk, and several clinical practice guidelines have stressed the importance of providing them with urgent care.6,7
Historically, because of the short-term risk of stroke, patients with suspected TIA have always been hospitalised. This tendency is changing with the implementation of urgent care clinics that reduce the hospitalisation rates in this group. The French study SOS-TIA8 found that providing 24-hour telephone care followed by rapid assessment was useful for early detection of patients at the greatest risk. Between 2003 and 2005, this system reduced the hospitalisation rate to 26%, and also lowered the rate of recurrence significantly. At the same time, the EXPRESS study, carried out in the UK, examined the effectiveness of referring patients to a specialist urgent care clinic on the day after the hospital visit. This initiative significantly reduced the recurrence rate.9
In the last few years, other models have also been developed to this end, and they are specific to the type of centre: rapid diagnosis in the emergency department or referral to an external urgent care clinic. Decisions may be based on clinical risk scales, principally the ABCD2 score. Some of the more recent series, which have employed a variety of methods, report 90-day recurrence rates of 1.7%-3.2%.10–12 Nevertheless, some authors question the benefits of non-hospital management of patients with TIA on the grounds that fibrinolysis can be administered more quickly to hospitalised than to non-hospitalised patients in cases of early recurrence. For this reason alone, hospitalisation may be cost-effective.13
In 2007, our hospital adopted a protocol for TIA intended to provide urgent care to patients, identify patients at the most risk, and avoid unnecessary hospital admissions. We present our results after 5 years of following the protocol.
Patients and methodsA neurologist is physically present at our hospital from 8.00 to 17.00 on workdays, but there is no 24-hour on-call neurology service. In February 2007, the hospital introduced its urgent TIA care protocol with the aim of reducing care delays and hospitalisation rates in this patient group. According to our protocol, the emergency department's initial assessment of a patient whose symptoms are compatible with TIA includes anamnesis, physical examination, laboratory analyses, electrocardiogram, and cranial computed tomography (CT). If the patient arrives during the neurologist's working hours, transcranial duplex ultrasound and Doppler ultrasound of the supra-aortic trunks are performed at the same time. Otherwise, the patient will remain under observation in a short stay unit so that the neurologist can complete the neurosonology study the following morning (unless the patient's age, functional status, or other reasons warrant an immediate neurosonology study). After the first emergency study, doctors decide whether the patient should be hospitalised or monitored on an outpatient basis for approximately 2 weeks. Follow-up studies vary according to the patient and the neurologist's decisions, but they may include routine neuroimaging (normally MRI), transthoracic echocardiography (also transoesophageal if necessary), 24-h Holter monitor, and in rarer cases, a complete blood count with a coagulation study. If the Doppler study detects severe stenosis or if results are not conclusive, doctors perform a complementary magnetic resonance angiography or CT angiography.
While the final decision resides with the neurologist, admission criteria include recurrent TIA, a finding of severe extracranial or intracranial large-vessel stenosis, the need for immediate anticoagulation treatment, and any other factors that would make outpatient monitoring more difficult.
This study presents an analysis of our results 5 years after having implemented our action protocol. We included all evaluated patients and analysed delay between symptom onset and hospital visit, in-hospital delays (between arriving at the emergency department, alerting the neurologist, consultation with the neurologist, and performing the neurovascular study), and the percentage of patients hospitalised after the neurological evaluation.
The study also included those patients who, for any reason, were not managed according to the indicated action protocol (admitted by the Emergency Department or formally referred to the outpatient clinic). Patients who were excluded from certain calculations are indicated.
For a final diagnosis, TIA was defined as a neurological deficit caused by ischaemia and lasting less than 24hours. Cases in which neuroimaging studies reveal an acute ischaemic lesion consistent with the symptoms (and symptoms do not continue beyond 24hours) are defined as TIA with lesion. These cases were included in the general TIA series.
Tobacco habit was defined as smoking regularly or having stopped less than 5 years previously. Hypertension was defined as previously documented blood pressure readings of 140/90mmHg or higher; dyslipidaemia was defined as a plasma cholesterol level >220mg/dL or documented history of treatment with lipid-lowering drugs. Patients were classed as diabetic if they had a documented history of diabetes or were undergoing treatment with oral antidiabetic drugs or insulin. Severe large-vessel stenosis was listed where there was a peak systolic velocity >220cm/s in the extracranial internal carotid, >220cm/s in the middle cerebral artery (MCA), >145cm/s in the posterior cerebral artery (PCA), or >140cm/s in the basilar artery.14,15
TIA aetiology was defined according to the Spanish Society of Neurology classification system.16 In cases in which severe carotid stenosis was detected and the patient needed interventional reperfusion therapy, this decision was made in the meeting between the Neurovascular Group and the tertiary referral hospital. The treatment was then carried out as quickly as possible, and preferably less than 2 weeks after symptom onset.
All patients with a final diagnosis of TIA were reevaluated 3 months after the event, preferably at the hospital, although telephone consultations were used if this was not possible. Patients answered questions about any recurrent events, including infarcts, new TIAs, intracranial haemorrhages, acute coronary syndromes, or episodes of peripheral ischaemia.
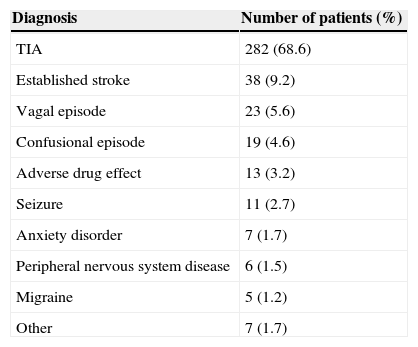
ResultsBetween 1 February 2007 and 31 January 2012, a total of 411 patients with a mean age of 71.5 years were evaluated; 231 were men (56.2%). The definitive diagnosis was TIA in 282 cases (68.6%), established stroke in 38 (9.2%), and other diagnoses in 91 (22.1%). Data are listed in Table 1.
Definitive diagnoses for all patients.
| Diagnosis | Number of patients (%) |
|---|---|
| TIA | 282 (68.6) |
| Established stroke | 38 (9.2) |
| Vagal episode | 23 (5.6) |
| Confusional episode | 19 (4.6) |
| Adverse drug effect | 13 (3.2) |
| Seizure | 11 (2.7) |
| Anxiety disorder | 7 (1.7) |
| Peripheral nervous system disease | 6 (1.5) |
| Migraine | 5 (1.2) |
| Other | 7 (1.7) |
The patient's delay between reaching the emergency department and being evaluated by the neurologist was less than 24hours in 82% of the cases and less than 48hours in 93.9%. Neurological evaluation and the neurosonology study were performed less than 24hours after consultation in 97.8% of all cases.
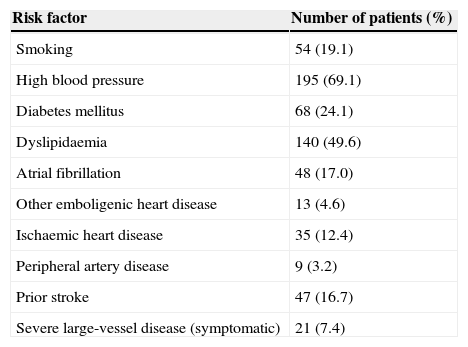
An analysis of the 282 patients diagnosed with TIA revealed a mean age of 71.6 years; 166 were men (58.9%). The most typical symptom was language deficit (38.7%) followed by hemiparesis (36.5%) and sensory deficit (29.8%). Vascular risk factors are listed in Table 2. The most common risk factor is AHT (69.1%), followed by dyslipidaemia (49.6%) and diabetes mellitus (24.1%). Examination revealed severe and symptomatic large-vessel disease in 21 patients (7.4%). Aetiology was large vessel atherothrombosis in 22.1%, cardioembolic in 18.7%, lacunar in 16.2%, and undetermined in 41.1%.
Vascular risk factors.
| Risk factor | Number of patients (%) |
|---|---|
| Smoking | 54 (19.1) |
| High blood pressure | 195 (69.1) |
| Diabetes mellitus | 68 (24.1) |
| Dyslipidaemia | 140 (49.6) |
| Atrial fibrillation | 48 (17.0) |
| Other emboligenic heart disease | 13 (4.6) |
| Ischaemic heart disease | 35 (12.4) |
| Peripheral artery disease | 9 (3.2) |
| Prior stroke | 47 (16.7) |
| Severe large-vessel disease (symptomatic) | 21 (7.4) |
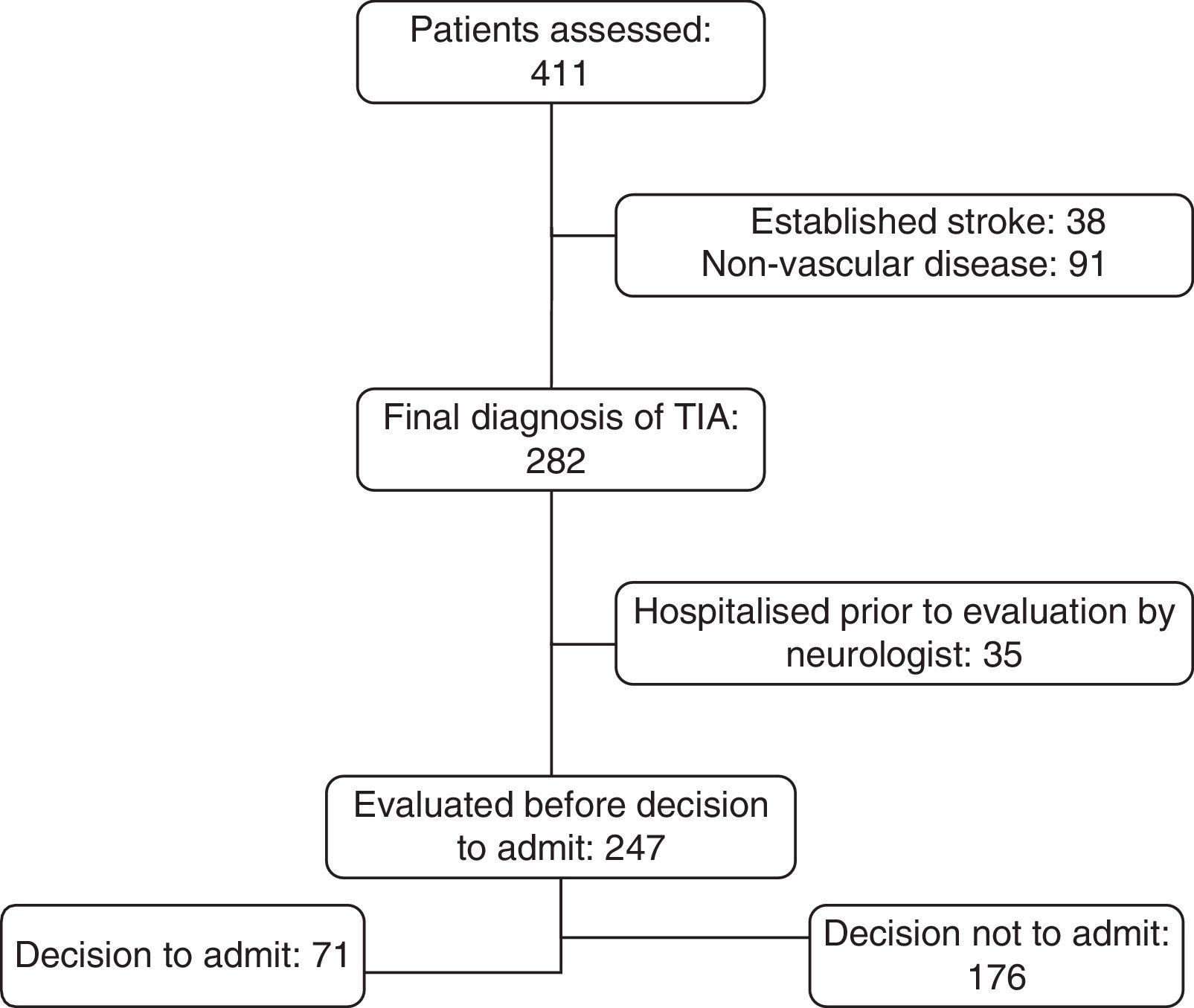
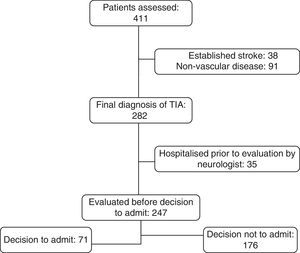
Leaving aside 35 patients who were admitted directly by the emergency department without prior examination by a neurologist, or examined on an outpatient basis without following the protocol, 71 of the remaining 247 patients (28.7%) were hospitalised after the neurological evaluation. Fig. 1 explains the steps taken in classifying patients. The most frequent reasons for admitting the patient were pathological findings in the Doppler study (31.0%), repeated TIA (25.3%), and severe heart disease or need for anticoagulant therapy (14.1%).
The 21 patients with signs of severe large-vessel disease were all hospitalised. Carotid occlusion was present in 6 of these patients, and intracranial stenosis was identified in 4. The remaining patients had severe carotid stenosis. Six cases were treated with endarterectomy or angioplasty with stenting within no more than 16 days, 2 patients refused treatment, 1 patient was not considered a candidate for the intervention, and 2 patients experienced stroke (with minimal sequelae in both cases) a few days after TIA and prior to reperfusion therapy.
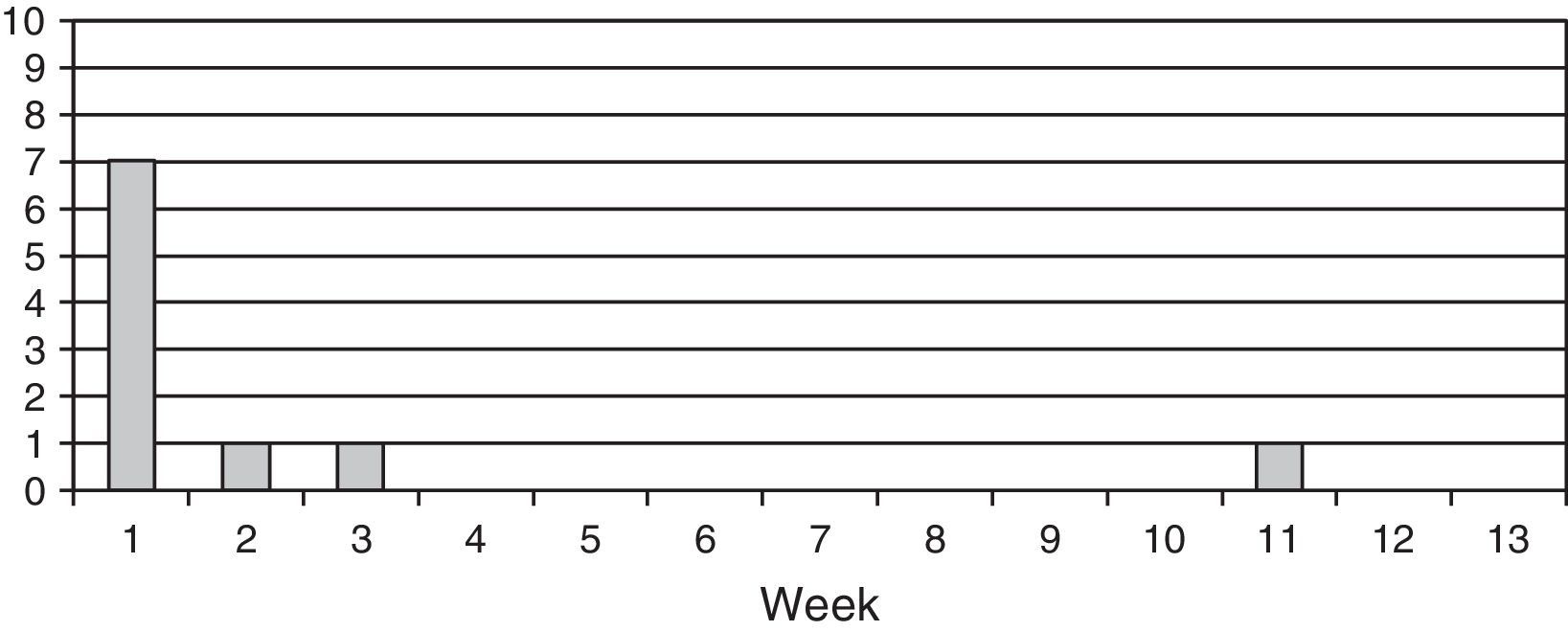
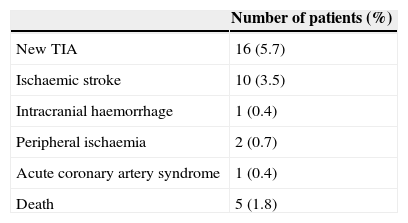
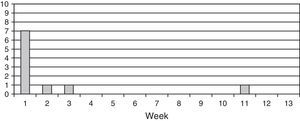
Incidents occurring in a 3-month follow-up period are listed in Table 3. It was not possible to obtain reliable information about 3 of the patients (1.06%). A total of 16 patients experienced an additional TIA. The rate of appearance of subsequent ischaemic stroke was 3.55% (10 patients). A weekly breakdown of this 3-month period, as displayed in Fig. 2, shows that 7 of these patients (70%) experienced recurrence within 1 week of the TIA, one had an episode in the second week, another in the third week, and the tenth in week 11. Further analysis of these 10 patients shows that the infarct territory was the same for the initial TIA and the subsequent event in 7 cases (territory was undetermined in the other 3). The cause of TIA was atherothrombotic in 8 patients, undetermined due to copresence of 2 causes in 1 patient, and small vessel disease in the remaining patient. Still within the same group, 7 displayed severe stenosis or large-vessel occlusion. The 3-month mortality rate in our series was 1.78%; a total of 5 patients died of ischaemic stroke (1), cerebral haemorrhage (2), and neoplasia (2).
All current guidelines recommend that patients with TIA be evaluated immediately in order to detect those at the greatest risk of recurrence in the short term. These patients should be hospitalised and monitored closely.6,7 In the past, patients with suspected TIA were admitted to hospitals. While TIA requires urgent assessment, the most recent tendency is to avoid hospitalisation. Two studies published in 2007 showed that implementing an urgent care system for TIA patients can simultaneously reduce the rate of admission and the frequency of recurrence. SOS-TIA,8 a 24-hour telephone hotline enabling consultations with a specialist nurse and a vascular neurologist, is a tool that facilitates immediate urgent care. In the EXPRESS study,9 patients were referred to an outpatient clinic on the workday subsequent to their arrival at the hospital. In the last 5 years, many hospitals have optimised their resources to develop a range of different urgent care models. Examples include urgent care units for TIA that identify high-risk patients12 or rapid triaging by emergency departments using the ABCD2 score.10,11 In our case, the evaluations were made by neurologists and included a neurovascular study on the day the patient arrives at the emergency department, or the morning of the next working day at the latest.
Providing urgent care for patients with TIA is a means of significantly reducing hospital admissions. In our series, 28.7% of the patients were admitted. This number is similar to results from other published series, although methodological differences, and probably the idiosyncrasies of each hospital as well, have resulted in a range of 17.3% and 65%.8,11,12,17,18
The main purpose of all rapid action protocols for TIA is to minimise the recurrence rate. In fact, recurrence rates after TIA have been dropping gradually over the past 10 years. Different studies published between 2004 and 2007, prior to the implementation of our protocol, report 90-day stroke rates that range between 3.5% and 17.3%, although most studies indicate between 9% and 10%.19–25 The 2 studies we mentioned, SOS-TIA8 and EXPRESS,9 were both published in 2007. They reported 90-day recurrence rates of 1.24% and 2.1% respectively, and rates in more recent years have dropped to between 1.7% and 6.7%.10–12,18,25–30 Our rate of ischaemic stroke (3.55% at 90 days) is one of the lowest of all reported published series.
One of the salient qualities of this study is the fact that 7 of the 10 episodes of ischaemic strokes occurred within 1 week of the TIA. Other series investigating this area report similar figures: between 55% and 67% of all recurrences occur within a week of the TIA, and according to some more in-depth studies, most such events occur within 48hours of the initial event.10,18,26,28,31 These data underscore the importance of urgent care and early diagnosis and treatment for this patient group.
The diagnosis of TIA is essentially clinically based. The need for quick decision-making regarding patients who are practically asymptomatic upon arrival also introduces the possibility that patients will be checked for TIA and assigned a different final diagnosis. In our case, 22.1% of the patients were diagnosed with a non-vascular disease. The same rate is also reported by SOS-TIA,8 but several other studies have indicated even higher rates ranging between 44% and 60%.11,12,32 Although these latter rates seem very high to us, we believe that a few ‘false alarms’ are acceptable in the context of a protocol like the one we describe. Proper training will allow us to reduce these percentages; in fact, in the case of our hospital, this rate has decreased steadily every year.
Hospital admissions have decreased and the evidence shows that recurrence rates have dropped thanks to a variety of different urgent care strategies for TIA. However, some critical voices maintain that these patients should be hospitalised since an early recurrence presenting while the patient is already in the hospital is more likely to be treated successfully.13 In our opinion, appropriate triage of high-risk patients who should be hospitalised is crucial to preventing certain admissions in addition to unnecessarily long hospital stays. Two recent studies support the decision to avoid hospitalisation where possible, based on the patient's clinical progress and also on cost-efficiency reasons.33,34
Our study has a few limitations. As has been stated, it reflects daily clinical practice in a hospital and lacks the methodological rigour of a clinical trial. The study includes all patients with TIA, which may have delivered heterogeneous patient characteristics and use of tests. Another consideration is that patients were not seen by neurologists as soon as they arrived at the hospital, which means that very early recurrences beginning prior to the neurological examination may not have been counted, and this could have decreased the observed recurrence rate somewhat. In any case, we feel that this series is an accurate reflection of daily clinical practice with minimal selection biases.
In summary, our results support the use of an urgent care protocol for patients with TIA in a hospital that lacks an on-call neurology service. The data show that it is possible to avoid hospital stays in most cases while still keeping recurrence rates under control.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Palomeras Soler E, Fossas Felip P, Cano Orgaz AT, Sanz Cartagena P, Casado Ruiz V, Muriana Batista D. Evaluación rápida del ataque isquémico transitorio en un hospital sin guardias de neurología. Neurología. 2015;30:325–330.