This study assesses the presence of sleep disturbances and their relationship with clinical and demographic variables in patients with MS, with a view to establishing correlations between the different variables and the frequency of sleep disturbances.
MethodsThe Pittsburgh Sleep Quality Index (PSQI) was used to detect sleep disorders. We contacted patients treated at the MS unit and distributed a questionnaire (PSQI) to 221 patients, receiving 142 usable questionnaires between 8 and 30 September 2019.
ResultsThe prevalence of patients with sleep disturbances in our study was 74.7% (73.7% in women and 76.8% in men). Therefore, sleep disorders are pervasive in patients with MS, with 3 out of 4 patients experiencing them, a higher rate than that observed in the population without the disease. The frequency of sleep disorders gradually increased in line with age. In the 2 age groups analyzed, 44–54 years and 55–68 years, the proportion of moderate and severe sleep disorders was 42.8% and 53.9%, respectively. Moderate and severe sleep disturbances were observed in 27.5%, 44.7%, and 58.3% of patients with Expanded Disability Status Scale scores of 0–3, 3–6, and >6, respectively.
ConclusionOur results indicate that sleep disorders are more common in patients with MS than in other populations. Patients with secondary progressive forms of MS more frequently present sleep disturbances, while patients with primary progressive forms report them less frequently. Age and degree of disability were positively correlated with the prevalence and severity of sleep disorders in MS patients.
Evaluamos la presencia de alteraciones del sueño en pacientes con EM y su relación con variables clínicas y demográficas en esta población para establecer correlaciones entre diversas variables y la frecuencia de trastornos del sueño.
MétodosSe utilizó el Índice de Calidad de Sueño de Pittsburgh para identificar la presencia de trastornos del sueño. Distribuimos el cuestionario a 221 pacientes de nuestra unidad de EM, y recibimos respuesta de 142 de ellos entre el 8 y el 30 de septiembre de 2019.
ResultadosEn nuestra muestra, el 74,7% de los pacientes presentaban trastornos del sueño (73,7% de las mujeres y 76,8% de los hombres). Nuestros resultados muestran que los trastornos del sueño están muy presentes en la EM, detectándose en 3 de cada 4 pacientes, lo que supone una proporción mayor que en la población general. La presencia de trastornos del sueño aumenta con la edad. En los 2 grupos etarios analizados (44-54 años y 55-68 años), la proporción de pacientes con trastornos del sueño moderados o graves fue del 42,8% y el 53,9%, respectivamente. El 27,5%, el 44,7% y el 58,3% de los pacientes con puntuaciones de 0-3, 3-6 y >6 puntos en la Escala Expandida del Estado de Discapacidad, respectivamente, presentaron trastornos del sueño moderados o graves.
ConclusiónNuestros resultados indican que los trastornos del sueño son más prevalentes en los pacientes con EM que en otras poblaciones. Dichos trastornos son más frecuentes en pacientes con EM secundaria progresiva que en pacientes con la forma primaria progresiva. La edad y el grado de discapacidad mostraron una correlación positiva con la prevalencia y la gravedad de los trastornos del sueño.
Multiple sclerosis (MS) is a chronic autoimmune disease of the central nervous system (CNS) that is increasingly common in young adults. Patients with MS have a significant variety of problems that decrease their quality of life, among which sleep disorders are described.1
Sleep disorders are pervasive in the general population, but they may be more frequent in patients with MS.2 The Prevalence of sleep disorders in patients with MS ranges from 47% and 62% and is higher in women.3 One study found that approximately one-third of people with MS use medications 2–3 times a week for sleep, which is very high compared to the general population.4 These alterations appear in all geographical locations, including areas with a lower prevalence of the disease, as is China.5 These disorders are also not recognized or diagnosed, especially in the early stages of the disease, and are therefore rarely treated in patients with MS.6 This lack of recognition means that their association with other problems, such as fatigue and cognitive decline, is also mostly undiagnosed.7
Patients with MS have many other problems associated with their disease, such as obstructive sleep apnea (OSA), that are not a direct result of the lesions considered characteristic of MS but are very involved in the disease's progression.8 It is well established that the Prevalence of this association was undervalued in the literature on MS.9 Sleep apnea, OSA, and central sleep apnea are the most frequently occurring sleep disorders in MS. OSA is characterized by obstructions of the respiratory tract throughout the night, requiring the patient to wake up several times to achieve the right muscle tone and receive adequate oxygenation.10 Restless leg syndrome (RLS)11 and its treatment may also trigger sleep disorders, especially insomnia, in patients with MS.
In MS patients, sleep disorders include difficulty sleeping that keeps patients awake and waking up very early in the morning and cannot fall asleep again. Patients with sleep disorders complain of excessive daytime sleepiness, memory and learning deficits, impaired concentration, altered mood, and fatigue. Little is known about the management of sleep disorders.12 Chronic insomnia disorder is expected in the general population, and depression, pain, and anxiety can also contribute to insomnia with MS. According to the results of different studies, patients with sleep disorders are at risk of exacerbating other problems, such as vascular diseases, obesity, and diabetes, which further threaten long-term health.13 There are multiple causes of poor sleep in MS patients, and possible triggers may be related to MS-related symptoms, specific sleep disorders, or drug therapy's adverse effects.14 Multiple medications frequently used by MS patients, including stimulants and beta interferons, can also contribute to insomnia, so their use should be evaluated.
It is tough to obtain an accurate picture of the complaints of patients with MS regarding the difficulties of controlling sleep disorders, and one of the most significant difficulties is that we do not know the true prevalence of these symptoms in patients with MS, especially in our setting. Whether sleep disturbance is related to age, gender disability, disease duration, or developmental process, it seems evident that it is necessary to conduct a prevalence study of sleep disorders in patients with MS and attempt to relate these disorders to the disease's characteristics. It will allow us to establish correlations between the different variables and the frequency of sleep disturbances in patients with MS.
MethodPatientsPatients from the Multiple Sclerosis (MS) Research and Treatment Unit of the Vithas Nisa Sevilla Hospital in Spain were contacted by email. All patients with MS had been diagnosed according to the revised 2017 version of the McDonald criteria, the study fully complied with national and international regulations and the Declaration of Helsinki (2000). All participants were fully informed of the research requirements and accepted the privacy and data exchange policy, with the consent of the patients, the Pittsburgh Sleep Quality Index15 (PSQI) was sent to 221 patients; 142 usable questionnaires were returned between September 8 and 30, 2019.
Evaluation of sleep qualitySleep quality used the PSQI to assess, a self-administered questionnaire used to evaluate sleep quality over the previous month. It comprises 19 self-response questions. PSQI is constructed of 7 components; each component is scored from 0 to 3, giving a total PSQI score ranging from 0 to 21; the higher the score is, the lower the sleep quality. Patients with scores of ≤5 are considered free of sleep disturbances, while scores from 6 to 10 indicate mild alterations in sleep, scores from 11 to 15 indicate moderate sleep disturbances, and scores from 16 to 21 indicate severe disturbances. The validity of the PSQI has been confirmed by several studies in different patient populations.16
The variables included and studied in the survey are as followsAge, gender, duration of disease, MS type (RR, SP, PP), and EDSS when the questionnaire is applied were included in the study.
Statistical analysisThe data were analyzed using the statistical program SPSS 22 for Windows. Quantitative variables are expressed as the means and standard deviations or as medians and 25th–75th percentiles according to whether they meet criteria for normal distribution. Qualitative variables are expressed as numbers and percentages within each group. For the quantitative variables, the approximation of normal distribution was verified by the Kolmogorov–Smirnoff test. Apply a regression method that would allow multivariable models to assess the statistical independence of the associations seen for age, MS type, disease duration, and disability.
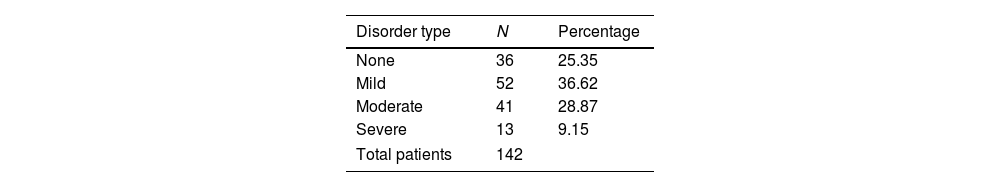
ResultsTable 1 shows the clinical characteristics of the patients.
We sent the questionnaire to 221 patients, and 142 patients responded to this study. PSQI scores were ≤5 in the 36 (25.3%) patients who did not report sleep disorders and >5 in the 106 (74.65%) who reported sleep disorders.
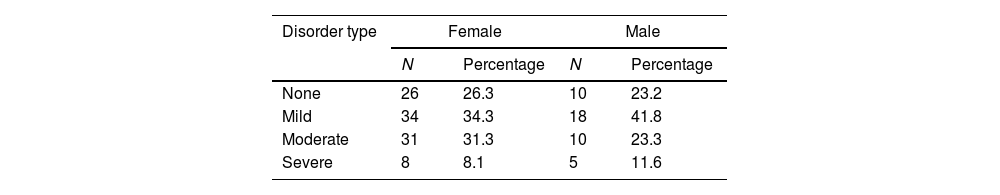
Table 2 shows 43 males and 99 females. There was no significant difference in sleep disorders in terms of gender; 26.3% of females were free of sleep disorders than 23.2% of males. The difference in the presence of severe sleep disturbances was somewhat higher, with 8.1% of women reporting severe alterations, compared with 11.6% of men.
The 142 patients ranged in age between 22 and 68 years and divided into four age groups, find sleep disorder cases gradually increased along with the age growth, in the two age groups (44–54 years and 55–68 years), the proportion of moderate and severe sleep disorders of 42.8% and 53.9% respectively, and the former two groups of (22–31years and 33–43) accounted for 27.8% and 29.7% respectively (Table 3).
Presence of sleep disturbances in the 142 patients according to PSQI and patient age (N: number).
| Disorder type | Age range | |||||||
|---|---|---|---|---|---|---|---|---|
| 22–32 | 33–43 | 44–54 | 55–68 | |||||
| N | Percentage | N | Percentage | N | Percentage | N | Percentage | |
| None | 6 | 33.3 | 10 | 27 | 13 | 23.2 | 5 | 16.1 |
| Mild | 7 | 38.9 | 16 | 43.3 | 19 | 34 | 9 | 29 |
| Moderate | 2 | 11.1 | 8 | 21.6 | 18 | 32.1 | 14 | 45.2 |
| Severe | 3 | 16.7 | 3 | 8.1 | 6 | 10.7 | 3 | 9.7 |
Regarding the duration of MS, the percentage of patients without sleep disorders was lower in the 20–29 year group (11%), while the percentage of patients without sleep disorders was 28, 27, and 30% in the group with a course of fewer than 20 years and more than 30 years, respectively. The fact that there was not a single case of severe sleep disorders in patients with an MS duration of 20 years or more is striking, although it should be noted that only 29 out of the 142 patients included in the study had a disease duration greater than 20 years (Table 4).
Presence of sleep disturbances in the 142 patients according to PSQI scores and duration of disease (N: number).
| Disorder type | Range of MS duration | |||||||
|---|---|---|---|---|---|---|---|---|
| 0–9 | 10–19 | 20–29 | 30–39 | |||||
| N | Percentage | N | Percentage | N | Percentage | N | Percentage | |
| None | 18 | 28 | 13 | 27 | 2 | 11 | 3 | 30 |
| Mild | 28 | 43 | 14 | 29 | 5 | 26 | 5 | 50 |
| Moderate | 10 | 15 | 17 | 35 | 12 | 63 | 2 | 20 |
| Severe | 9 | 14 | 4 | 8 | 0 | 0 | 0 | 0 |
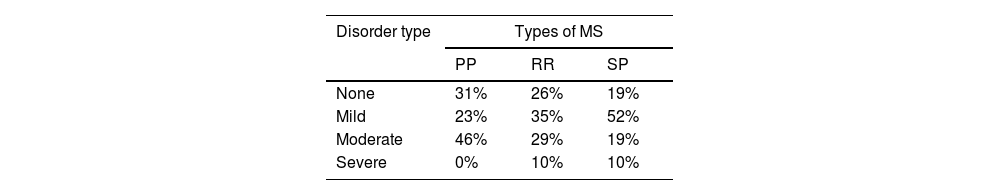
Of great interest is assessing possible differences in the presence of sleep disturbances according to the different forms of disease progression. Due to the lack of subjects with Progressive-relapsing MS (PR), the 3 cases with this type of progression were included in the primary progressive (PP) group (Table 5). In the PP group, 31% of the patients did not have sleep disorders. Among those with the relapsing-remitting (RR) type of MS, 26% did not have sleep disorders, while 19% of patients with the secondary progressive (SP) type of MS were free of sleep disturbances. In PPMS patients, there were no cases of severe sleep disorders. In comparison, 10% and 10% of patients with RR and SP forms of MS, respectively, reported severe sleep disorders.
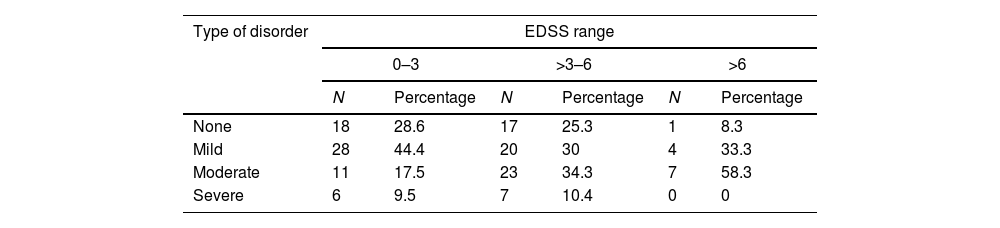
Regarding the relationship between sleep disorders and disability, as measured by the Expanded Disability Status Scale (EDSS), 28.6%, 8.3% of patients with EDSS scores of 0–3 and >6 were free of sleep disturbances, while 25.3% had some intermediate disabilities (scores of 3–6). Moderate and severe sleep disturbances were observed in 27.5%, 44.7%, and 58.3% of patients with EDSS scores of 0–3, 3–6, and >6, respectively (Table 6).
Presence of sleep disturbances in the 142 patients according to PSQI and EDSS scores (N: number; EDSS: Expanded Disability Status Scale).
| Type of disorder | EDSS range | |||||
|---|---|---|---|---|---|---|
| 0–3 | >3–6 | >6 | ||||
| N | Percentage | N | Percentage | N | Percentage | |
| None | 18 | 28.6 | 17 | 25.3 | 1 | 8.3 |
| Mild | 28 | 44.4 | 20 | 30 | 4 | 33.3 |
| Moderate | 11 | 17.5 | 23 | 34.3 | 7 | 58.3 |
| Severe | 6 | 9.5 | 7 | 10.4 | 0 | 0 |
In this study, we descriptively analyzed the presence of sleep disturbances in patients with MS about the disease's characteristics. All our data were obtained by email, the questionnaires were valid, but there is a lack of clinical diagnostic techniques that can be used to confirm and verify sleep disorders. Of course, this study has other limitations. First, a control group was not included, and the number of patients included was limited. Second, due to the cross-sectional design of the current study, it was impossible to obtain information on long-term changes in patients with MS, which could be related to sleep disorders.
The overall prevalence was higher than those described in the literature to date, and previous studies have shown a prevalence ranging between 25.2% and 67.1%5,8,17–24 (Table 7). Therefore, sleep disorders can be considered a prevalent disease in patients with MS; three-quarters of patients suffer from them; the prevalence is significantly higher than that of people not affected by it. This apparent discrepancy in frequency can be explained by the MS populations studied, which were based on small samples, or by differences in the definition of sleep disorders and the methods used to assess sleep quality.
Prevalence of sleep disturbances with MS, medical journals (1994–2018).
| Years | Authors | Journal | Place of study | Number of patients | Age | Gender (sleep disturbance) | Forms studied | Prevalence (sleep disturbance) |
|---|---|---|---|---|---|---|---|---|
| 1994 | Tachibana N.18 | Eur Neurol | London, UK | 28 | – | – | – | 25.2 |
| 2004 | Lobentanz I.S.24 | Acta Neurol Scand | Vienna, Austria | 504 | – | – | All | 61.9 |
| 2004 | Alarcia R.17 | Neurologia | Zaragoza, Spain | 100 | – | – | RR, SP | 36.0 |
| 2007 | Merlino G.8 | Sleep Med | Udine, Italy | 120 | 46.1 | M: 26.3 | RR, SP | 47.5 |
| 2008 | Bamer A.M.21 | Mult Scler | Washington, USA | 1063 | – | – | All | 64.8 |
| 2012 | Aarseth J.19 | PLoS One | Bergen, Norway | 90 | 46.2 | F: 78; M: 53.1 | All | 67.1 |
| 2012 | Neau J.P.20 | Eur Neurol | Poitiers, France | 205 | – | – | RR, SP, PP | 54.3 |
| 2016 | Ma Shengli5 | Sleep Breath | Zhengzhou, China | 231 | 42.2 | F: 65.2; M: 34.8 | All | 64.9 |
| 2017 | Garland S.23 | Int J Behav Med | St. John's, NL, Canada | 743 | 64.6 | F: 79.8; M: 20.3 | All | 43.0 |
| 2018 | Alhazzani A.22 | J Neurol Psychiatr Neurosurg | Riyadh, Saudi Arabia | 112 | 32.8 | F: 8.3; M: 20 | RR | 12.5 |
The prevalence of moderate and severe sleep disturbance in men and women is 51.5%, according to Bamer et al.21 However, our study's prevalence was 38%, perhaps due to the use of different scales to evaluate sleep quality. In particular, Alhazzani et al. assessed the prevalence of insomnia symptoms in non-depressed patients in Saudi Arabia and found that only 12.5% of non-depressed patients had insomnia.22 However, none of our previous studies excluded MS patients with depression, suggesting that depression may be related to insomnia. Aside from the comorbidities, no demographic or clinical variables were associated with sleep problems in individuals with MS.
The distribution by gender did not show a significant difference between men and women, which is similar to the results of Vitkova et al.12 thus, sleep disorders seem to affect both genders similarly. Perhaps it is necessary to conduct more research to confirm this fact since there are limited data in this study. Concerning the patients’ age, we found a clear relationship between age and sleep disorders in MS patients, with an increased rate of sleep disorders occurring with age,25 severity was also positively correlated. Moreover, as the hormone production decreases with age, an inverse correlation with the frequency of low sleep quality, it has been suggested that melatonin deficit is at least partly responsible for sleep disorders.26
The reviewed literature that addresses the subject under study suggests that poor sleep is more common in women and patients with a longer duration of illness.10,18 However, our cross-sectional sample showed that poor sleep was not significantly associated with the duration of the disease, nor was it associated with the gender of the patients. Although in the first three decades of living with MS, sleep disturbances increased with the duration of disease, none of the patients in our study indicated having severe sleep disorders after 20 years of disease duration. There are no data in the literature related to this point. It is likely that patients with more extended progressions better accept the disease's symptoms, including sleep disturbances, but we do not have enough consistent data to confirm this hypothesis. In this study, it can be interpreted that as the disease progresses, and the patient becomes accustomed to living it, severe sleep disorders disappear.
A critical point of this study is the relationship between sleep disorders and the developmental form of MS. It is evident that patients with the PP form are least likely to report sleep disorders (31%), and no patients in this group had severe alterations, which were frequent in the RR and SP forms (10% and 10%, respectively, in the RR and SP). Only 19% of patients with the SP form did not report sleep disturbances; that is, more than 4 out of every five patients were affected by sleep disturbances, which is a much higher proportion than observed in the rest of the disease type groups. These disorders, especially the most severe ones, affect patients with the SP forms of MS significantly.
Some studies suggest that higher EDSS and shorter duration of MS are associated with a higher prevalence of sleep disorders,16,24 but the majority of authors5,17,27,28 did not find these relationships. In our study, it has been shown that low sleep quality was directly correlated with a higher degree of disability, as measured by the EDSS. Maybe the higher the disability, the more complications the patient has, Such as fatigue, spasm, etc.; these factors should also be considered. Sleep disorders worsen and are strongly related to other MS symptoms, especially fatigue, which is very relevant to diffuse symptomatology, i.e., symptoms not clearly related to localized lesions. Additionally, sleep disorders aggravate fatigue in patients with MS. Sleep disturbance might trigger an acute MS exacerbation.27 The presence of some associated symptoms (such as fatigue, spasm, and nocturia), which can be the leading causes of sleep disturbance among MS patients, was not evaluated.
In this study, some symptoms could be explained by demographic characteristics, which vary among countries and prevent the extrapolation of the results from one country to another; thus, the study may not be very generalizable. However, knowing sleep disturbances are essential for the management of MS patients. This data must be communicated to the general physicians who generally manage these symptoms in MS patients. Enhancing the awareness and knowledge of the modifiable risk factors for poor MS sleep may be necessary for programming early therapeutic and prophylactic interventions.
ConclusionsThe results of our study indicate that sleep disorders in MS patients are more common than in other populations. Patients with SP forms of MS present more frequent sleep disturbances, while patients with PP forms report less frequently. Age and degree of disability were positively correlated with the prevalence and severity of sleep disorders in MS patients. Gender and time of disease progression show less related to the presence and severity of sleep disturbances in MS patients; some data suggest that poor sleep is more common in women and patients with longer illness duration but less severe sleep disturbances.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributionsGuo-Xun Zhang and Guillermo Ayuso Izquierdo conceived and designed the study. Guo-Xun Zhang responsible for data collection and analysis and drafted the manuscript. Guillermo Ayuso Izquierdo reviewed and revised the paper. All authors read and approved the manuscript.
Conflict of interestAuthors declare that they have no conflict of interest or financial ties to disclose.
This study was supported by the Multiple Sclerosis Unit, Neurology Service, Vithas Nisa Hospital, Seville, Spain.