In recent months, doubts have arisen among patients, general practitioners, and neurologists as to whether some drugs commonly used in patients with headaches and neuralgia may favour or complicate the disease caused by SARS-CoV-2.
Material and methodsWe collected information on the opinions of scientific societies and medicines agencies (American, European, and Spanish) to clarify doubts regarding the use of drugs such as lisinopril, candesartan, ibuprofen, corticosteroids, carbamazepine, and monoclonal antibodies targeting the calcitonin gene–related peptide in the context of the COVID-19 pandemic.
ResultsWe make recommendations about the use of standard headache treatments in the context of the COVID-19 pandemic, based on the current scientific evidence.
ConclusionsAt present, there is no robust scientific argument to formally contraindicate any of the standard treatments employed for headaches and neuralgias.
En los últimos meses han surgido dudas por parte de pacientes, médicos de familia y neurólogos sobre la posibilidad de que algunos de los fármacos que habitualmente se utilizan en cefaleas y neuralgias puedan facilitar o complicar la infección por el SARS-COV-2.
Material y métodosHemos recabado información sobre el posicionamiento de sociedades científicas, así como de las distintas Agencias de Medicamentos (americana, europea y española) para poder esclarecer dudas respecto al uso de fármacos como lisinopril, candesartán, ibuprofeno, corticoides, carbamazepina, anticuerpos monoclonales contra el CGRP durante la pandemia por COVID-19.
ResultadosPlanteamos recomendaciones acerca del uso de fármacos habituales en el tratamiento de las cefaleas en el contexto de la pandemia por COVID-19, basándonos en las evidencias de las que disponemos en el momento actual.
ConclusionesActualmente, no existe ningún argumento científico robusto para contraindicar formalmente ninguno de los tratamientos que se emplean en cefaleas y neuralgias.
In the light of numerous questions raised in recent months by patients, family doctors, and neurologists about the possibility that certain drugs habitually used to treat headache and neuralgia may promote or complicate SARS-CoV-2 infection, the Spanish Society of Neurology’s Headache Study Group wishes to make the following statement:
This hypothesis is based on a limited number of studies that do not address this subject as the main objective, and use in vitro or experimental models of poor quality, which do not contribute scientific evidence. Nonetheless, their conclusions have been exaggerated by certain media outlets, causing concern among the general population and healthcare professionals.
No scientific or neurological organisation has yet taken a position on the treatment of existing headache in patients with COVID-19; so far, the literature only includes opinion articles. We also consider it important to address this issue in the light of recent evidence of new-onset headache in patients with COVID-19, and the implications for their treatment.1–3 Therefore, we issue the following detailed recommendations on the drugs concerned.
Lisinopril and candesartanThese drugs are indicated for the preventive treatment of migraine, with level of evidence 2 and grade of recommendation B.4 Lisinopril is an angiotensin-converting enzyme (ACE) inhibitor and candesartan is an angiotensin receptor II blocker (ARB). These are the only renin-angiotensin system inhibitors used in the treatment of migraine.
ACE inhibition prevents the conversion of angiotensin I into angiotensin II, which has potent vasoconstrictive effects and regulates aldosterone release by the adrenal glands.
ACE is produced in various tissues, including in the central nervous system, kidneys, and lungs. ACE2 is an enzyme homologous to ACE, and is responsible for the degradation of angiotensin II to angiotensin; therefore, its physiological effect is opposite to that of ACE. ACE2 is a membrane enzyme that regulates the entry of the SARS-CoV-2 virus into cells. In humans, ACE inhibitors inhibit ACE but not ACE2, although animal studies have found that both ACE inhibitors and ARBs upregulate ACE2 expression when administered in high doses.5–8
International, European, and American organisations9–12 consider ACE inhibitors and ARBs not to be contraindicated in hypertensive patients with suspected or confirmed COVID-19: these drugs may even be beneficial, if upregulation of ACE2 leads to decreased angiotensin II levels in the lungs. Furthermore, withdrawing these drugs may exacerbate the underlying cardiovascular or kidney disease in some patients, leading to greater mortality rates. Therefore, their suspension is also not indicated in patients with migraine.
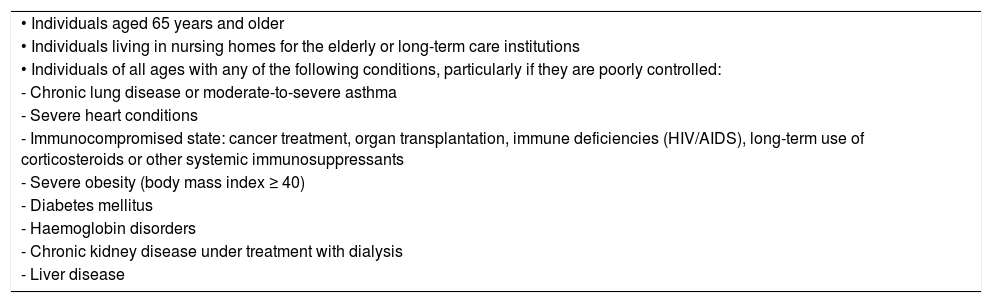
Nonetheless, we recommend not beginning preventive treatment of migraine with these drugs in the context of the COVID-19 pandemic. Other treatment options are available when first-line treatments have been exhausted; these include venlafaxine (level of evidence 2, grade of recommendation B), zonisamide (level of evidence 4), and lamotrigine (level of evidence 4).4 We also recommend evaluating other treatment options in patients already taking lisinopril or candesartan for migraine and presenting risk factors for severe COVID-19 (Table 1).
Risk factors for severe COVID-19 proposed by the United States Centers for Disease Control and Prevention.
| • Individuals aged 65 years and older |
| • Individuals living in nursing homes for the elderly or long-term care institutions |
| • Individuals of all ages with any of the following conditions, particularly if they are poorly controlled: |
| - Chronic lung disease or moderate-to-severe asthma |
| - Severe heart conditions |
| - Immunocompromised state: cancer treatment, organ transplantation, immune deficiencies (HIV/AIDS), long-term use of corticosteroids or other systemic immunosuppressants |
| - Severe obesity (body mass index ≥ 40) |
| - Diabetes mellitus |
| - Haemoglobin disorders |
| - Chronic kidney disease under treatment with dialysis |
| - Liver disease |
Ibuprofen is indicated for acute episodes of migraine of moderate intensity, with level of evidence 1 and grade of recommendation A.4
Without a doubt, this is the drug that has been subject to the greatest controversy and raised the most concern, as it is one of the most widely used drugs worldwide for the symptomatic treatment of migraine attacks. The concerns about ibuprofen originated in an article published in The Lancet on 11 March 2020, warning that ibuprofen may increase ACE2 expression, leading to clinical worsening of COVID-19.13 Eight days later, the World Health Organization announced this finding, but issued a correction shortly thereafter, stating that there was no scientific evidence supporting this claim. The United States Food and Drug Administration, European Medicines Agency, and Spanish Agency of Medicines and Medical Devices have issued statements to the same effect, and recommend that research be done on the subject.14–16 The possible association between exacerbation of SARS-CoV-2 infection and treatment with ibuprofen and ketoprofen is being evaluated by the European Medicines Agency’s Pharmacovigilance Risk Assessment Committee. In rats, ibuprofen increases ACE2 levels in the heart only; this effect has not been observed in other organs.8,17 It should be noted that the dose used in the experimental animals is equivalent to 3 g in humans, whereas the maximum recommended dose for migraine treatment is 1800 g/day.4
Therefore, we recommend avoiding new indication of ibuprofen only in patients with migraine and presenting risk factors for severe COVID-19 (Table 1). In patients already using the drug, we do not recommend changing the treatment, although physicians should advise patients to avoid excess consumption of ibuprofen (more than 15 pills/month).
It should also be noted that alternative drugs are available for treating moderate migraine attacks; these include naproxen, indometacin, and diclofenac. Finally, triptans can also be used: these drugs are indicated for moderate-severe migraine attacks.
CorticosteroidsCorticosteroids are indicated as a transitional preventive treatment for cluster headache and for the treatment of status migrainosus (level of evidence 4 and grade of recommendation C for both indications).4
Indication of these drugs to treat COVID-19 is controversial. The United States Centers for Disease Control and Prevention contraindicate corticosteroids based on previous experience with the 2003 SARS-CoV epidemic, when several articles reported that early use of corticosteroids was associated with higher plasma viral load and delayed viral clearance.18 However, they may be beneficial in the early stage of SARS-CoV-2 infection, reducing the duration of mechanical ventilation and overall mortality rates in patients with established moderate-to-severe adult respiratory distress syndrome19; no randomised studies have been performed, however.20
As corticosteroids are known to cause immunosuppression, we recommend avoiding the habitual indication of 1 mg/kg orally in patients with cluster headache during the pandemic and extending the use of occipital nerve block with triamcinolone, methylprednisolone, or betamethasone; these drugs have the same level of evidence and practically no systemic effects, since the corticosteroid is injected locally.4 Clinical guidelines also mention other treatment options for delayed preventive treatment, including verapamil (level of evidence 1, grade of recommendation A), lithium carbonate (level of evidence 2, grade of recommendation B), topiramate (level of evidence 2, grade of recommendation B), valproic acid (level of evidence 4, grade of recommendation C), gabapentin (third-line treatment), and botulinum toxin A.4
Parenteral or oral corticosteroids are also used to treat status migrainosus in emergency departments4; however, as they are prescribed for very short schedules, we do not recommend avoiding them, except in cases of strong suspicion or diagnosis of severe COVID-19 (Table 1).
CarbamazepineCarbamazepine is indicated for the treatment of trigeminal neuralgia, with level of evidence 1 and grade of recommendation A.4
No study has addressed the relationship between the drug and COVID-19; however, given that its potential adverse effects include leukopaenia, we recommend considering other options before indicating it as a new treatment, especially in patients with risk factors for severe COVID-19 (Table 1). COVID-19 typically presents with lymphocytopaenia, which may be exacerbated by carbamazepine-induced leukopaenia. Patients not presenting risk factors for severe COVID-19 (Table 1) and who have already been receiving the drug for over 3 months should be monitored with laboratory blood analyses. This recommendation should also be extended on an individual basis to patients with trigeminal neuralgia taking sodium channel blockers: eslicarbazepine acetate, oxcarbazepine (level of evidence 4, grade of recommendation C), and lamotrigine (level of evidence 2, grade of recommendation B). Other treatment options are available, including pregabalin, gabapentin, baclofen (level of evidence 4, grade of recommendation C), and botulinum toxin A.4
Anti-CGRP monoclonal antibodiesPublished trials and clinical experience have shown that treatment of migraine with anti-CGRP monoclonal antibodies does not increase the risk of infection or immunosuppression, as they seem not to compromise the immune system. Therefore, we do not recommend suspending this treatment during the pandemic.
The literature includes studies of MERS-CoV and SARS-CoV infection in patients receiving immunomodulatory or immunosuppressive treatment. Disease progression and mortality rates were not worse in patients receiving immunosuppressants, chemotherapy, or organ transplants.21
In the current pandemic, case series have been published of patients undergoing organ transplantation22,23 or receiving immunomodulatory treatment for multiple sclerosis24; poorer prognosis is not reported in these patients.
Furthermore, it has been suggested that these treatments may have a protective effect: through their influence on lymphocytes, they may block the cytokine storm occurring in the most severe cases of infection. A clinical trial is also underway into the treatment of COVID-19 with fingolimod, which induces lymphocytopaenia through lymphocyte sequestration.25 However, insufficient information is available to support or reject this hypothesis.
Interactions between preventive drugs for headache and COVID-19 drugsIt is essential to take precautions against potential interactions between preventive treatments for migraine, such as amitriptyline, beta blockers, verapamil, mirtazapine, and valproic acid, and drugs used to treat COVID-19, such as lopinavir/ritonavir, hydroxychloroquine, chloroquine, and azithromycin.26
The majority of these drug-drug interactions are classed as risk category C; therefore, the joint use of these drugs is not contraindicated, but close monitoring is needed to prevent adverse reactions or loss of efficacy.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Morollón N, Belvís R, De Dios A, Pagès N, González-Oria C, Latorre G, et al. Tratamientos habituales utilizados en cefaleas, neuralgias y SARS-CoV-2. Posicionamiento del grupo de estudio de cefaleas de la Sociedad Española de Neurología. Neurología. 2020;35:628–632.