Stroke is a very common cause of death, especially in southern Spain. The present study analyses in-hospital mortality associated with stroke in an Andalusian tertiary care hospital.
MethodsWe gathered the files of all patients who had died at Hospital Universitario Virgen de las Nieves in Granada in 2013 and whose death certificates indicated stroke as the cause of death. We also gathered stroke patients discharge data and compared them to that of patients with acute coronary syndrome (ACS).
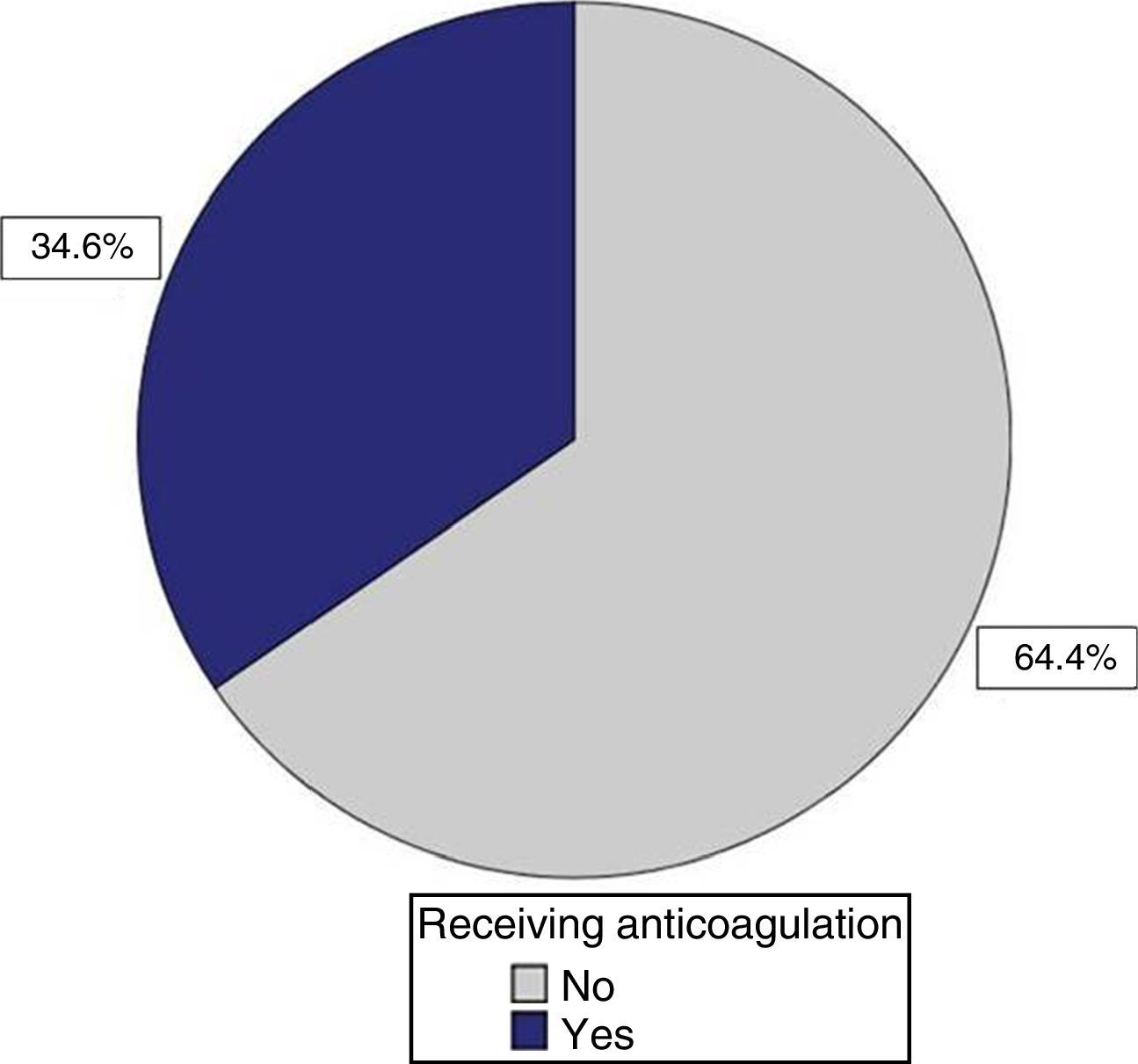
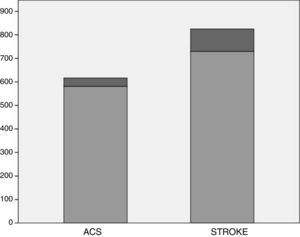
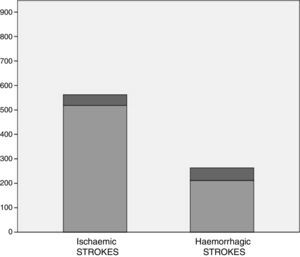
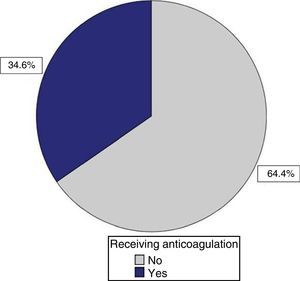
ResultsA total of 825 patients had a diagnosis of stroke (96 deaths, 11.6%); of these, 562 had ischaemic stroke (IS) (44 deaths, 7.8%) and 263 haemorrhagic stroke (HS) (52 deaths, 19.7%). Patients with HS therefore showed greater mortality rate (odds ratio, OR 2.9). Patients in this group died after a shorter time in hospital (median, 4 vs. 7 days; mean, 6 days). However, patients with IS were older and presented with more comorbidities. On the other hand, 617 patients had a diagnosis of ACS (36 deaths, 5.8%). The mortality odds ratio was 2.1 (stroke/SCA). Around 23% of the patients who died from stroke were taking anticoagulants. 60% of the deceased patients with IS and 20% of those with HS had atrial fibrillation (AF); 35% of the patients with IS and AF were taking anticoagulants.
ConclusionsStroke is associated with higher admission and in-hospital mortality rates than SCA. Likewise, patients with HS showed higher mortality rates than those with IS. Patients with fatal stroke usually had a history of long-term treatment with anticoagulants; two-thirds of the patients with fatal IS and AF were not receiving anticoagulants. According to our results, optimising prevention in patients with AF may have a positive impact on stroke-related in-hospital mortality.
El ictus constituye una causa muy frecuente de muerte, especialmente en el sur de España; se analiza la mortalidad intrahospitalaria asociada a ictus en un hospital andaluz de tercer nivel.
MétodosRegistro de pacientes con ictus como diagnóstico en su informe de defunción en el Hospital Virgen de las Nieves de Granada durante 2013. Se utilizan además datos globales sobre altas en ictus y se comparan con iguales variables en síndrome coronario agudo (SCA).
ResultadosAltas con diagnóstico de ictus 825 (96 defunciones, 11,6%); 562 isquémicos (44 fallecidos, 7,8%); 263 hemorrágicos (52 muertes, 19,7%). Los hemorrágicos, por tanto, tuvieron mayor mortalidad (OR = 2,9) y más precoz durante el ingreso (mediana 4 vs. 7 días, global 6 días), aunque los isquémicos fueron más ancianos y más pluripatológicos. Altas con SCA 617 (36 fallecidos, 5,8%); OR de mortalidad en ictus/SCA = 2,1. Un 23% de los fallecidos con ictus estaban anticoagulados cuando lo presentaron. El 60% de los ictus isquémicos y el 20% de los ictus hemorrágicos fallecidos tenían fibrilación auricular; solo el 35% de los pacientes con ictus isquémico y fibrilación auricular estaban anticoagulados.
ConclusionesEl ictus supera al SCA en ingresos y mortalidad intrahospitalaria. El ictus hemorrágico supera al isquémico en mortalidad asociada. La anticoagulación crónica es frecuente en pacientes con ictus fatal; 2 tercios de los pacientes con ictus isquémico mortal y fibrilación auricular no estaban anticoagulados. Según nuestros resultados, optimizar la prevención en pacientes con fibrilación auricular podría impactar favorablemente sobre la mortalidad intrahospitalaria asociada al ictus.
Stroke is one of the leading causes of death: the second most frequent in men and the first in women, according to various studies.1 It is also one of the most common causes of sudden disability and dependence in adults. The Andalusian Public Health System has addressed the condition through 2 editions of an integrated care process (ICP) (“cerebrovascular accident” in 20022 and “stroke” in 20153) and the Stroke Plan 2010-2014.1 This is theoretically an adaptation of the national stroke strategy published by the Spanish Ministry of Health,4 although its care proposals diverge both from those of the national strategy and from the stroke care plan published by the Spanish Society of Neurology,5 essentially in that it assigns neurologists little or no role in the management of acute strokes. Death due to stroke is 50% higher in Andalusia than the national average, making the region part of the so-called “Spanish stroke belt”.6,7 More research is needed, particularly studies based on data from Andalusia.8,9 Subjects of interest are the mortality caused by and associated with stroke9–14 and the burden of the condition on hospitals in terms of incidence and mortality. We analysed in-hospital mortality associated with stroke at a tertiary referral hospital in Andalusia over a period of one year, and contextualised this both against stroke admissions in absolute terms and against acute coronary syndrome (ACS), which is comparable to stroke in terms of epidemiology and care requirements.
Patients and methodsThe central offices of the Andalusian Public Health Service issued all hospitals and primary care districts a document listing stroke-related in-hospital deaths in each department in 2013, inviting analysis and proposals for improvement. These series comprise those patients with stroke recorded on their hospital death certificates, either alone or with other diagnoses. This includes both ischaemic stroke (IS) and haemorrhagic stroke (HS) (subarachnoid haemorrhage [SAH], intraparenchymal haemorrhage, and other non-traumatic intra- and extracerebral cranial haemorrhages [ICH]).
The list of deaths at Hospital Virgen de las Nieves in Granada was used to build a database with personal details and data on age, sex, stroke type, unit where the patient died, polypathology (presence of multiple conditions), whether the patient was aged over 80, and whether revascularisation had been carried out for IS. The database also included data on whether patients were receiving anticoagulant treatment and whether the international normalised ratio (INR) at admission was above the therapeutic range. On account of the geographic dispersion of the centres comprising our hospital, we also explicitly noted whether IS patients were admitted to the neurology department on recommendation by the on-call neurologist, who is present 24hours a day, or “by order of the head doctor on call”. This is the case when a stroke patient considered to require admission to the polypathology or palliative care units (located in a separate building) remains in the observation unit for over 48hours. From a clinical perspective, stroke severity at baseline (mild [NIHSS>7], moderate [NIHSS 7-13], severe [NIHSS 14-24], or very severe [NIHSS>24 or profound coma at onset]), stroke topography (carotid or vertebrobasilar for IS; ICH or SAH for HS), IS subtype (atherothrombotic, cardioembolic, lacunar, cryptogenic, or undetermined due to incomplete evaluation), and probable cause of death (neurological deterioration, sepsis, or single or multiple organ failure) were deduced from the hospital death certificate. IS subtype classification was pragmatic: cases were classified as cardioembolic stroke when patients had a compatible clinical and neuroimaging profile and a major risk factor for cardioembolic stroke, generally atrial fibrillation (AF). However, many of these patients did not undergo full evaluation of the circle of Willis and the supra-aortic trunks, as this was not considered productive. Cases classified as atherothrombotic stroke were those where no emboligenic heart disease was detected and where significant stenosis of the blood vessel involved was demonstrated by duplex sonography, CT angiography, or MRI angiography. All data were gathered through case-by-case analysis of hospital death certificates. As the data on discharged patients with stroke included only the total number and not these clinical variables, it was impossible to make comparisons against a control group of non-deceased patients.
‘Polypathological’ patients were considered as an entity because these patients, and patients with HS, are considered ‘marginal limits’ in the 2015 stroke ICP3; patients aged over 80 are also particularly fragile and vulnerable to such a process as severe and acute as stroke. Polypathological cases were those where stroke was accompanied by advanced dementia, uncontrolled neoplastic disease, or severe single or multiple organ failure, with the comorbidity posing a greater risk to the patient than the stroke itself.
The on-call neurologist evaluates all stroke patients arriving at hospital, completes the diagnostic process initiated by emergency department staff, and assesses patient eligibility for repermeabilising treatment; if administered, this is monitored in the intensive care unit (ICU), as the hospital has no acute stroke unit (ASU). If repermeabilisation is considered unsuitable, patients remain under observation in the emergency department until they are clinically stable, at which time the neurologist decides whether the patient should be admitted to the neurology department, depending on diagnosis and treatment expectations. If the stroke is found to be haemorrhagic (intraparenchymal, subarachnoid, or other haemorrhage) during initial assessment, the patient is assigned to the hospital's neurosurgery department, as the neurology department lacks an ASU and for other ‘historical’ reasons. These patients are frequently admitted to the ICU.
As the registry contains only hospital death certificates, it does not include deaths caused by or associated to acute strokes taking place outside of hospital before arrival or after discharge. Nor does it include patients with strokes who died in the emergency department observation unit prior to formal admission, or for whom a medical death certificate including death codification was not required at that time.
In order to evaluate the burden of stroke-associated mortality on hospitals, we gathered data from the hospital's medical records on the number of patients discharged with diagnoses of stroke or transient ischaemic attack (TIA) the same year, and the number of ACSs and associated in-hospital deaths.
A descriptive study of the different variables considered produced several conclusions. Since this is an observational study based on data taken from a registry with limitations, and there is no control group, hypothesis testing was only applied to certain internal comparisons, using the Chi-square test for categorical variables and non-parametric tests for non-normally distributed continuous variables.
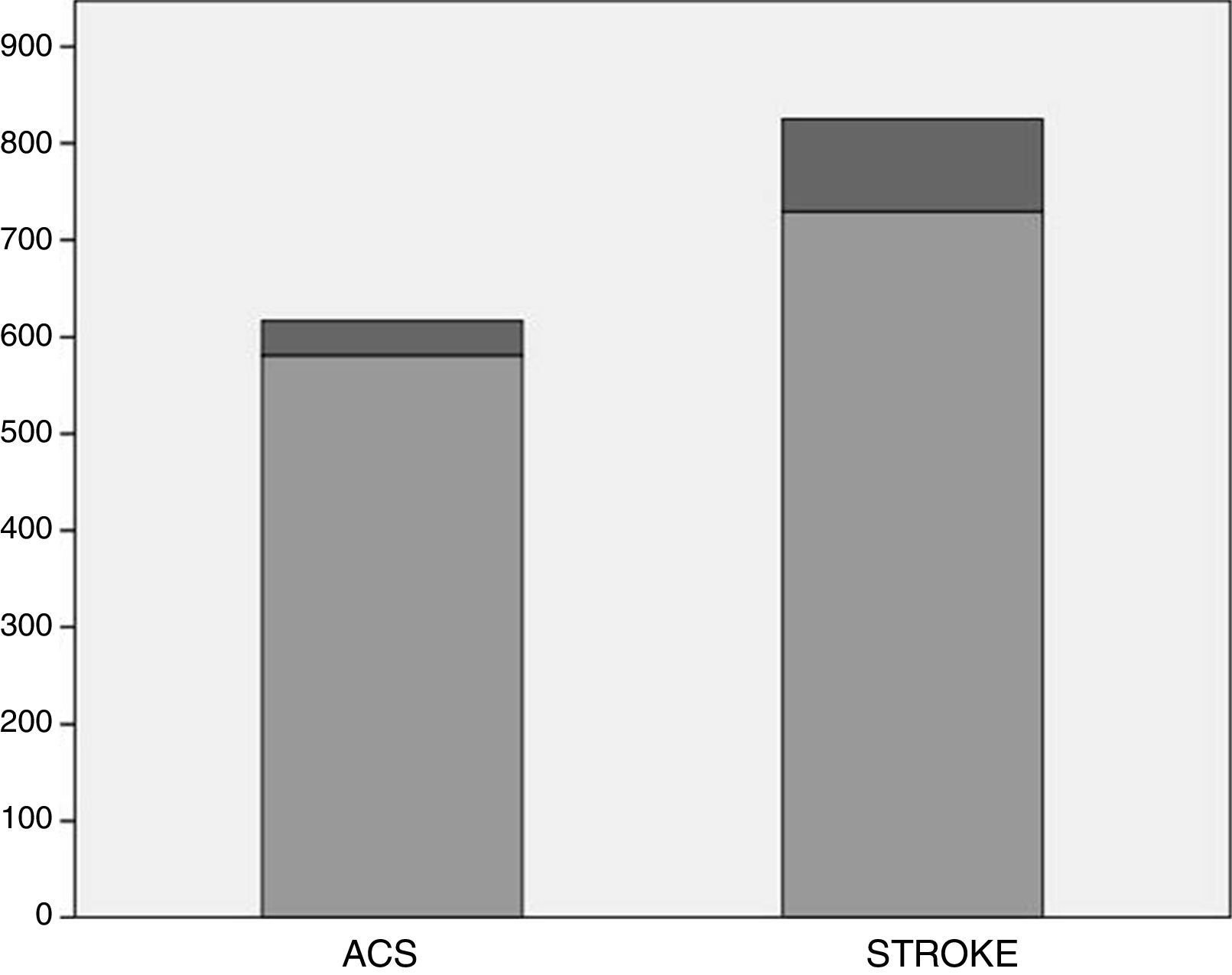
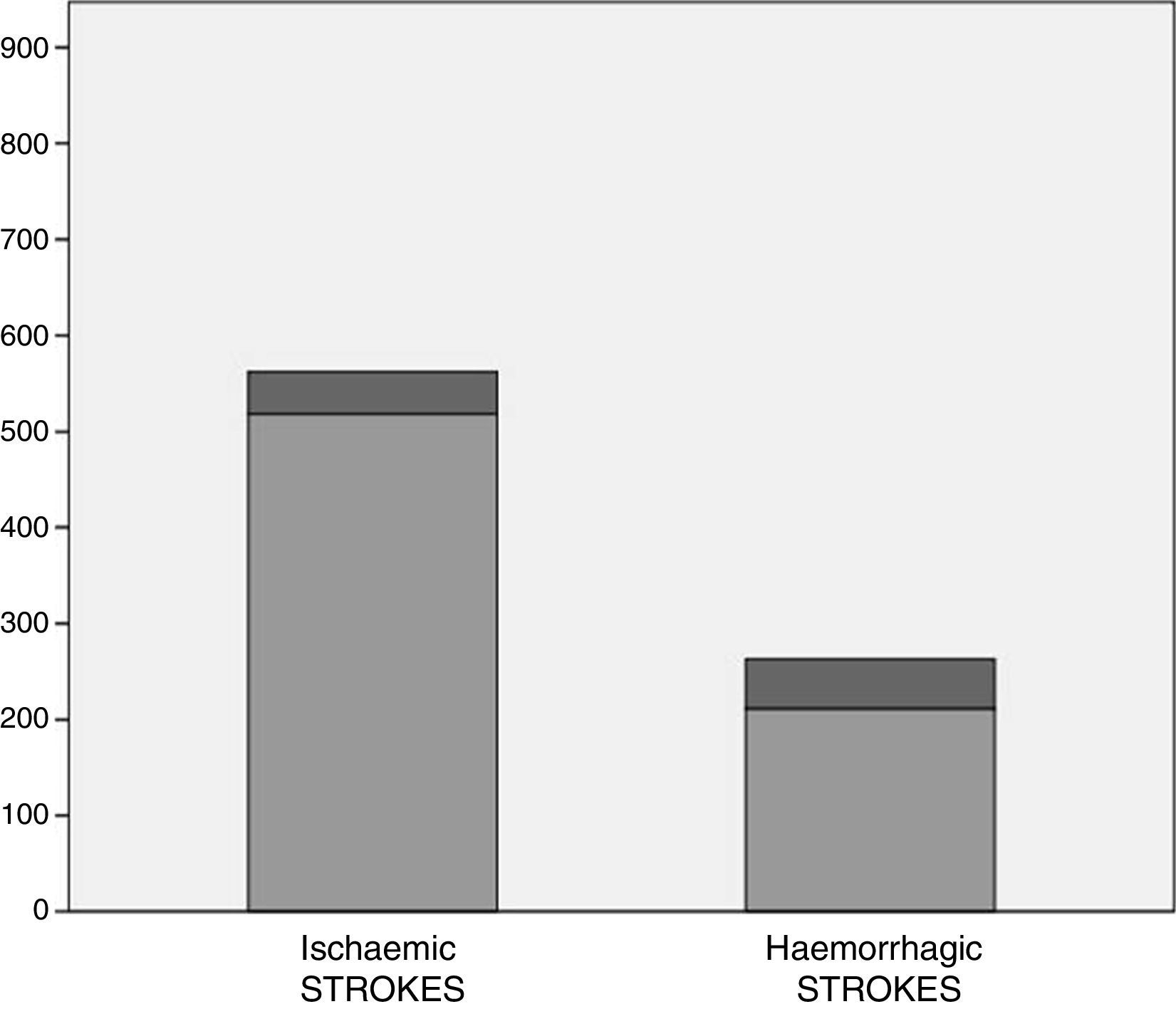
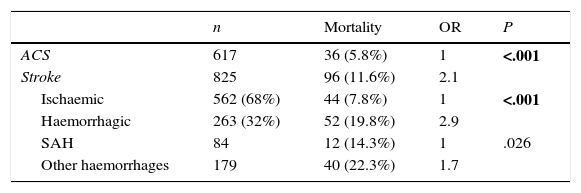
ResultsA total of 825 patients were admitted with stroke or TIA according to diagnoses recorded at discharge or on hospital death certificates (562 IS: 486 established and 76 TIA; 263 HS: 116 intraparenchymal haemorrhages, 84 SAH, and 63 non-traumatic haemorrhages in other locations). Of this total, 96 patients died after formal admission to hospital, representing an in-hospital mortality rate of 11.6% for all strokes, 7.8% for IS, and 19.8% for HS (14.3% for SAH and 22.3% for intraparenchymal and other haemorrhages) (Table 1 and Figs. 1 and 2). Mortality was higher for HS than for IS (odds ratio, OR 2.9, P<.001). In HS patients, mortality due to SAH was lower than that associated with other types of haemorrhage; differences, however, were not significant (OR 1.7).
Patients admitted to hospital in 2013 with diagnoses of stroke or ACS (n=1442).
| n | Mortality | OR | P | |
|---|---|---|---|---|
| ACS | 617 | 36 (5.8%) | 1 | <.001 |
| Stroke | 825 | 96 (11.6%) | 2.1 | |
| Ischaemic | 562 (68%) | 44 (7.8%) | 1 | <.001 |
| Haemorrhagic | 263 (32%) | 52 (19.8%) | 2.9 | |
| SAH | 84 | 12 (14.3%) | 1 | .026 |
| Other haemorrhages | 179 | 40 (22.3%) | 1.7 |
SAH: subarachnoid haemorrhages; ACS: acute coronary syndrome. Statistically significant values are shown in bold.
In the same period, 617 patients were admitted with diagnoses of ACS: 469 with acute myocardial infarction, 62 with angina, and 86 with other forms of ACS; of this total, 36 (5.8%) died in hospital (Table 1 and Fig. 1). As is the case for stroke, this figure does not include patients who died in the emergency department prior to formal admission. The number of patients admitted with stroke was higher than that for ACS and mortality was significantly higher in patients with stroke (OR 2.1, P<.001).
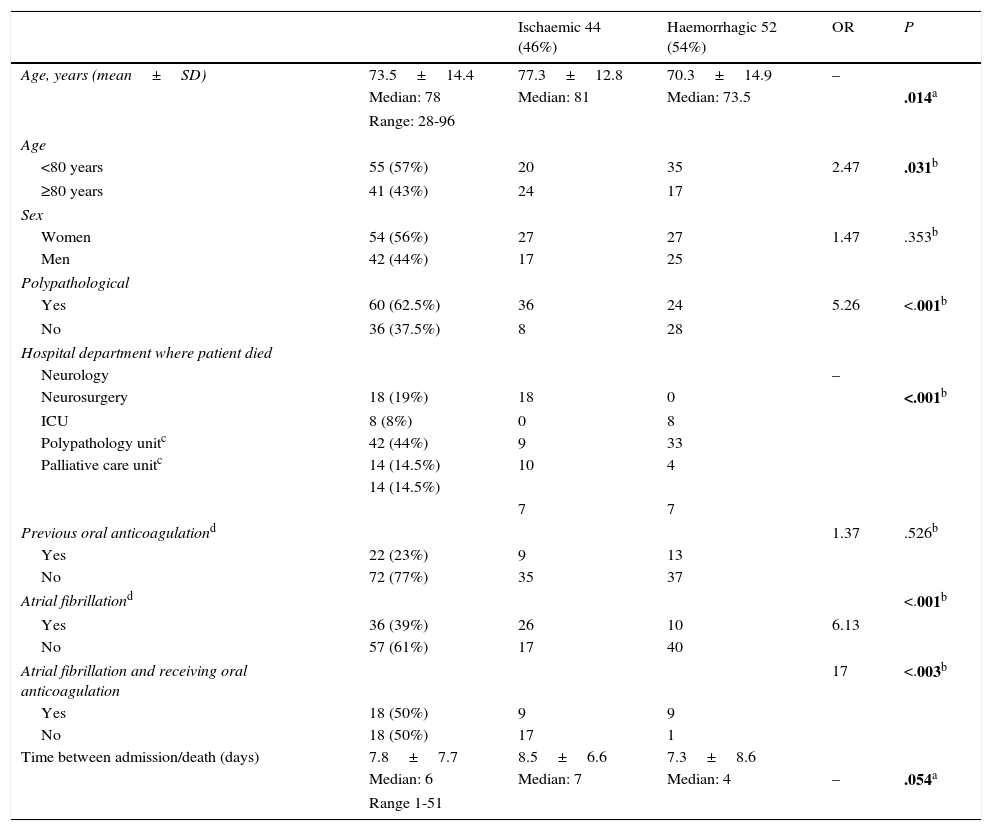
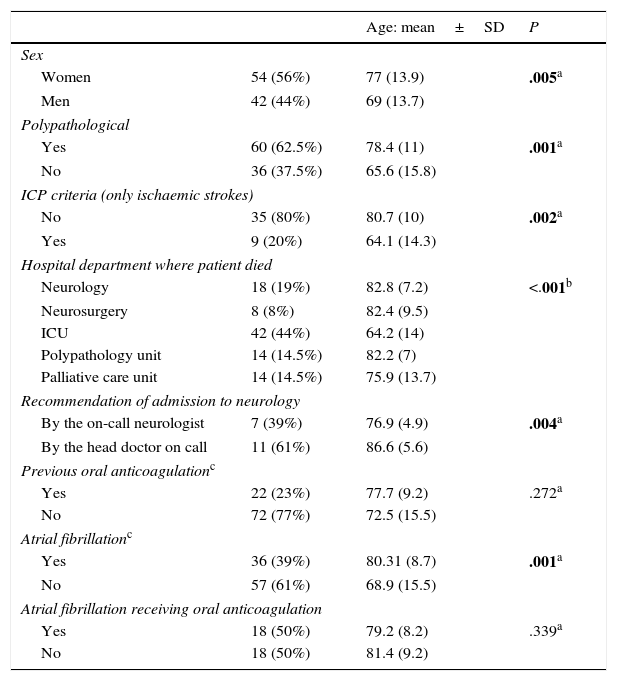
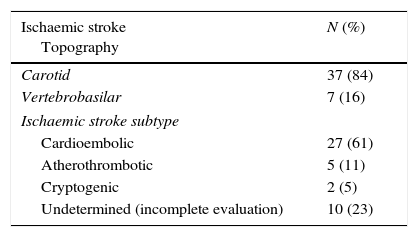
Table 2 summarises the analysis of the variables taken into consideration according to ischaemic or haemorrhagic aetiology of the fatal stroke. Table 3 shows an analysis of the ages of the various subgroups. Of the 18 patients who died in the neurology department, whose mean age was 82.8 years, only 7 had been admitted on recommendation of the on-call neurologist (mean age 76.9 years). Table 4 shows clinical information on the stroke patients who died; the most frequent cause of death both in patients with HS and in those with IS was neurological deterioration, although single or multiple organ failure and sepsis both had a certain prevalence in patients with IS.
Patients diagnosed with strokes who died at hospital in 2013 (n=96): bivariate analysis for type of stroke.
| Ischaemic 44 (46%) | Haemorrhagic 52 (54%) | OR | P | ||
|---|---|---|---|---|---|
| Age, years (mean±SD) | 73.5±14.4 | 77.3±12.8 | 70.3±14.9 | – | |
| Median: 78 | Median: 81 | Median: 73.5 | .014a | ||
| Range: 28-96 | |||||
| Age | |||||
| <80 years | 55 (57%) | 20 | 35 | 2.47 | .031b |
| ≥80 years | 41 (43%) | 24 | 17 | ||
| Sex | |||||
| Women | 54 (56%) | 27 | 27 | 1.47 | .353b |
| Men | 42 (44%) | 17 | 25 | ||
| Polypathological | |||||
| Yes | 60 (62.5%) | 36 | 24 | 5.26 | <.001b |
| No | 36 (37.5%) | 8 | 28 | ||
| Hospital department where patient died | |||||
| Neurology | – | ||||
| Neurosurgery | 18 (19%) | 18 | 0 | <.001b | |
| ICU | 8 (8%) | 0 | 8 | ||
| Polypathology unitc | 42 (44%) | 9 | 33 | ||
| Palliative care unitc | 14 (14.5%) | 10 | 4 | ||
| 14 (14.5%) | |||||
| 7 | 7 | ||||
| Previous oral anticoagulationd | 1.37 | .526b | |||
| Yes | 22 (23%) | 9 | 13 | ||
| No | 72 (77%) | 35 | 37 | ||
| Atrial fibrillationd | <.001b | ||||
| Yes | 36 (39%) | 26 | 10 | 6.13 | |
| No | 57 (61%) | 17 | 40 | ||
| Atrial fibrillation and receiving oral anticoagulation | 17 | <.003b | |||
| Yes | 18 (50%) | 9 | 9 | ||
| No | 18 (50%) | 17 | 1 | ||
| Time between admission/death (days) | 7.8±7.7 | 8.5±6.6 | 7.3±8.6 | ||
| Median: 6 | Median: 7 | Median: 4 | – | .054a | |
| Range 1-51 | |||||
Unless otherwise indicated, values represent mean±SD for quantitative variables and absolute frequencies (percentages) for categorical variables. Statistically significant values are shown in bold.
Patients diagnosed with strokes who died at hospital in 2013 (n=96): bivariate analysis for age.
| Age: mean±SD | P | ||
|---|---|---|---|
| Sex | |||
| Women | 54 (56%) | 77 (13.9) | .005a |
| Men | 42 (44%) | 69 (13.7) | |
| Polypathological | |||
| Yes | 60 (62.5%) | 78.4 (11) | .001a |
| No | 36 (37.5%) | 65.6 (15.8) | |
| ICP criteria (only ischaemic strokes) | |||
| No | 35 (80%) | 80.7 (10) | .002a |
| Yes | 9 (20%) | 64.1 (14.3) | |
| Hospital department where patient died | |||
| Neurology | 18 (19%) | 82.8 (7.2) | <.001b |
| Neurosurgery | 8 (8%) | 82.4 (9.5) | |
| ICU | 42 (44%) | 64.2 (14) | |
| Polypathology unit | 14 (14.5%) | 82.2 (7) | |
| Palliative care unit | 14 (14.5%) | 75.9 (13.7) | |
| Recommendation of admission to neurology | |||
| By the on-call neurologist | 7 (39%) | 76.9 (4.9) | .004a |
| By the head doctor on call | 11 (61%) | 86.6 (5.6) | |
| Previous oral anticoagulationc | |||
| Yes | 22 (23%) | 77.7 (9.2) | .272a |
| No | 72 (77%) | 72.5 (15.5) | |
| Atrial fibrillationc | |||
| Yes | 36 (39%) | 80.31 (8.7) | .001a |
| No | 57 (61%) | 68.9 (15.5) | |
| Atrial fibrillation receiving oral anticoagulation | |||
| Yes | 18 (50%) | 79.2 (8.2) | .339a |
| No | 18 (50%) | 81.4 (9.2) | |
P value: non-parametric tests were used due to the non-normal distribution of age by subgroup. Statistically significant values are shown in bold.
Some clinical details of patients with stroke who died.
| Ischaemic stroke Topography | N (%) |
|---|---|
| Carotid | 37 (84) |
| Vertebrobasilar | 7 (16) |
| Ischaemic stroke subtype | |
| Cardioembolic | 27 (61) |
| Atherothrombotic | 5 (11) |
| Cryptogenic | 2 (5) |
| Undetermined (incomplete evaluation) | 10 (23) |
| Severity P=.005 | Ischaemic* | Haemorrhagic* | Total |
|---|---|---|---|
| Mild (NIHSS<7) | – | – | – |
| Moderate (NIHSS 7-13) | 6 (13.5) | 6 (12) | 12 (12.5) |
| Severe (NIHSS 14-24) | 32 (73) | 22 (42) | 54 (56) |
| Very severe (NIHSS>24 or profound coma) | 6 (13.5) | 24 (46) | 30 (31.5) |
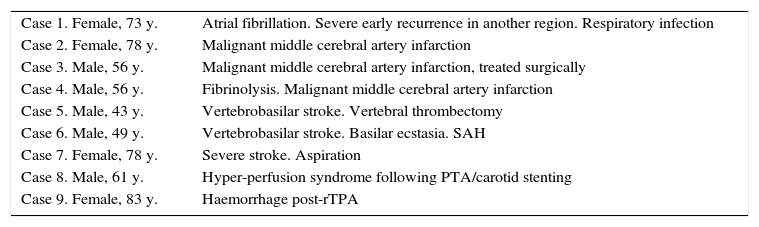
Table 5 describes the clinical characteristics of the 9 patients meeting the stroke ICP who died.
Causes of death in patients with ischaemic stroke meeting 2015 integrated care process for stroke.3
| Case 1. Female, 73 y. | Atrial fibrillation. Severe early recurrence in another region. Respiratory infection |
| Case 2. Female, 78 y. | Malignant middle cerebral artery infarction |
| Case 3. Male, 56 y. | Malignant middle cerebral artery infarction, treated surgically |
| Case 4. Male, 56 y. | Fibrinolysis. Malignant middle cerebral artery infarction |
| Case 5. Male, 43 y. | Vertebrobasilar stroke. Vertebral thrombectomy |
| Case 6. Male, 49 y. | Vertebrobasilar stroke. Basilar ecstasia. SAH |
| Case 7. Female, 78 y. | Severe stroke. Aspiration |
| Case 8. Male, 61 y. | Hyper-perfusion syndrome following PTA/carotid stenting |
| Case 9. Female, 83 y. | Haemorrhage post-rTPA |
Ischaemic strokes without “multimorbidity and/or polypathology”.
PTA: percutaneous transluminal angioplasty; SAH: subarachnoid haemorrhage; y: years.
Taken from Jiménez Hernández.3
Of the 22 patients who were receiving anticoagulation at the time of stroke, only one, with HS, had an INR higher than 3. However, in 12 of the 22 cases, data for this variable was either unavailable or was irrelevant since vitamin K antagonists (VKA) were not administered (2 dabigatran in patients with IS; one low-molecular-weight heparin [LMWH] for HS).
DiscussionEven without a record of patients who died prior to formal admission to hospital (which may be somewhat higher for ACSs than for stroke, on account of the former's greater rate of immediate mortality), it seems evident that the number of patients with stroke admitted to our hospital is greater than that of ACSs, and that the impact of stroke on in-hospital mortality is twice that of ischaemic heart disease.
Our data reflects a trend, also shown by other studies, according to which mortality due to stroke is higher and occurs at older ages in women than in men; this is true both for IS and for HS.1,4
Haemorrhagic stroke were more severe than IS; mild severity at stroke onset was not observed in any patient. Due to the lack of a control group, it was not possible for this study to analyse individual variables that may have contributed to the final outcome, such as age, comorbidity, stroke type and IS subtype, or initial severity.
The first striking detail in this series is the high proportion of deceased patients who had HS: while around 80% of strokes are estimated to be ischaemic and 20% haemorrhagic (with SAH accounting for one quarter of these), the number of patients with HS in our series who died was slightly larger than those with IS. This supports the hypothesis that mortality associated with HS is far higher than that of IS (OR 2.9, according to our data). It is necessary to qualify these raw figures: ours is the only hospital in our setting which offers neurocritical care, neurosurgery, and interventional neuroradiology, and draws patients with HS from other centres in the area and bordering provinces. In contrast, according to the Andalusian stroke plan's1 recommendations on IS management, other hospitals without neurology departments are considered autonomous in treating those patients, and make few referrals. In fact, 263 patients were admitted with HS, compared to 562 with IS and TIA, a higher ratio of haemorrhagic to IS than the estimated incidence (68% IS). These figures stand in contrast to those published by another hospital in Granada, lacking the specialities mentioned above, where 87.5% of a series of 100 consecutive patients admitted in 2000 had IS.8
Secondly, we should note the high incidence of polypathology in stroke patients who died (62.5%), particularly patients with IS: 81% of deceased IS patients and 46.1% of deceased HS patients had multiple conditions (OR 5.26, P<.001). This is at least partly due to the more advanced age of patients with IS: patients were aged 80 or over in 54.5% of IS and 32.7% of HS cases (OR 2.47, P=.031); these patients would therefore be fragile or vulnerable and display the high mortality rate that would be expected.15 HS-related mortality was higher despite the fact it affected younger patients with fewer comorbidities.
Of the patients with IS meeting the criteria of the stroke ICP, few died (9 of the 44 IS patients who died, of 562 IS patients admitted). The stroke ICP3 considers HS and polypathology (comorbidity) to be ‘marginal limits’, although it does not define these concepts, for which reason we formulated an ad hoc definition for this analysis. The clinical characteristics of these deaths are summarised in Table 5. Given the severity of the clinical situations, it seems these deaths would have been difficult to prevent, with the possible exception of one case where the intermediate cause was aspiration of vomit in a patient with severe stroke. Only one death is attributable to haemorrhage due to intravenous thrombolysis (the procedure was carried out in 62 patients during the year studied), and 3 were caused by malignant middle cerebral artery infarction, of which one was associated to intravenous fibrinolysis and another occurred despite decompressive craniectomy.
One striking detail is the high number of deceased patients, with both IS and HS, who were receiving anticoagulant treatment (23%). There was a non-significant trend for anticoagulation to be more frequent in patients who died with HS. Almost all these patients were treated with VKA, with the exception of one who received a therapeutic dose of LMWH. Considering that AF, the most frequent cause of anticoagulation, has a prevalence of 5%-6% in those aged over 65,16,17 and that only half of patients with AF are estimated to receive anticoagulation, then the prevalence of patients receiving anticoagulation in the general population of over-65s should be 2%-3%. However, the proportion of patients receiving anticoagulation among those whose deaths were related to stroke was 23%, implying a strong association between oral anticoagulation with VKA and the risk of fatal stroke. In 2013, when the cases in this series were gathered, direct anticoagulants were less frequently used than today; therefore, only 2 patients in the IS group were treated with dabigatran. A total of 20.4% of the patients with IS who died received anticoagulation, mostly due to AF. However, only 34.6% of patients with FA and IS were receiving anticoagulant treatment when the stroke occurred; therefore, almost 70% of these patients had fatal IS when they were not receiving anticoagulation (Fig. 3). It is known that cardioembolic stroke is the most severe and the most fatal IS subtype,12–14 and that presence of AF is an aggravating factor in the progression of both cardioembolic and atherothrombotic stroke progression.18 The number of patients with atherothrombotic strokes who died was far lower than that of patients with cardioembolic strokes; this group represented a very large proportion (61%) in this series, around twice that typically observed in hospital registries. No patients with lacunar stroke died (Table 4).
Current standard treatments for IS, such as intravenous thrombolysis,19 are known to have an effect on functional prognosis (which is not taken into account in our analysis), but have little impact on mortality. The same is true of the new forms of endovascular treatment, which are and have been available only periodically at our centre; these have recently shown promising results for functional prognosis20 but have limited impact on mortality rates. Four of the 44 patients with IS who died received fibrinolysis; 2 of these were in the subgroup of 9 patients meeting the criteria of the stroke ICP. Thrombectomy was performed in a vertebral artery of another patient.
Although efficient, extensive use of revascularisation treatments may not alter the crude mortality rate, optimised management of both IS and HS in an ASU (which our hospital lacks, despite repeated applications made since 1995) may improve mortality rates and functional outcomes. Expert neurological care, which should be provided early,21 during admission,10,22 has a known impact on the mortality and functional prognosis of stroke. In our centre, patients with strokes are treated by neurologists from the moment they arrive; with the exception of terminal or polypathological patients, cases of IS are evaluated and treated in the cerebrovascular pathology section of the neurology department, by neurologists who work exclusively with stroke. For this reason, our mortality data cannot be extrapolated to other centres in Andalusia, where neurologists have little or no participation in this process.8–10 The 2015 ICP3 recommends only that patients with stroke be evaluated by neurologists in the first 3 months following the episode “in order to complete the aetiological study”. Our mortality figures are comparable to those observed in other Spanish registries, although it is difficult with hospital records to adjust for the differing clinical characteristics of each hospital's patients, which sometimes also include TIAs.23,24
As shown in Table 3, the patients with strokes who died in the various departments were of similar age, with the exception of patients who died in the ICU, who were of significantly lower age, and those who died in the palliative care unit, who were also younger (Table 3). In these patients, the stroke diagnosis was often combined with advanced cancer. Patients who died in the neurology department were of more advanced age because a large number were not admitted on recommendation of the neurologist, due to a shortage of beds in the polypathology unit. Patients who were admitted on express recommendation of the on-call neurologist were significantly younger (76.9 years vs 82.8 years for all patients admitted to the department [Table 3]).
In conclusion, mortality due to stroke would appear to be high both in absolute terms and in comparison to acute ischaemic heart disease, a similar process. Women of more advanced age tend to be more affected. Mortality associated to HS is far higher than IS-associated mortality, even taking account of the fact that polypathology and the fragility associated to advanced age were less prevalent in the HS patients who died.
We consider that in order to reduce stroke-associated mortality, it is necessary to reduce incidence by emphasising primary and secondary prevention of both ischaemic and HS. In line with our data, this may more specifically include more rational, extensive use of oral anticoagulation in candidate patients and wider use of the new alternatives to VKAs, which in this series are associated to stroke-related mortality. Compared to VKAs, the new direct oral anticoagulants achieve equal or lower IS incidence rates in patients with AF, and reduce risk of HS by up to and additional 60%.25–29
No conclusions can be drawn regarding the impact on mortality of potential measures to optimise the management of the acute phase of HS. We are not able to assess whether the lack of an ASU and the consequent management of these patients in other departments (emergency department observation unit, ICU, etc.) influences mortality. However, should such an influence exist, it may be less pronounced in our centre, at least for IS, the main form treated in the neurology department. Our department is in a better position than those of other hospitals in the region, which in addition to ASUs, also lack vascular neurologists, or indeed any neurologists, to treat acute stroke.8–10 It should be noted that according to the results of the PRACTIC study, the involvement of neurologists in the diagnosis and treatment of acute stroke would lead to annual reductions in Spain of over 1933 deaths, 1859 new strokes, 2778 vascular episodes, and over 5520 deaths or cases of functional dependency caused by cerebrovascular disease.22,30 If the health authorities wish to see a reduction in deaths caused by or associated to stroke, then some of the steps to be taken are clear.
Finally, we would comment that 19 of the 96 patients who died after suffering a stroke, that is almost one fifth, died in shared rooms in general wards (11 in neurology, 8 in neurosurgery) with limited nursing and auxiliary staff. The days between admission and death (mean 7.8 days, median 6; Table 2) can help calculate the resources required to care for these patients, whose deaths are often unavoidable, with the dignity they deserve.
FundingThis study has received no funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.
Dr. Antonia Fernández Valdivia, of the Hospital Virgen de las Nieves’ Admissions and Medical Records service, for providing us with the invaluable data that made this study possible. Dr. Cristóbal Carnero Pardo, from the hospital's neurology department, for his helpful comments on a previous version of the manuscript.
Please cite this article as: Maestre-Moreno JF, Fernández-Pérez MD, Triguero-Cueva L, Gutiérrez-Zúñiga R, Herrera-García JD, Espigares-Molero A, et al. Mortalidad asociada al ictus en un hospital andaluz de tercer nivel. Análisis y reflexiones. Neurología. 2017;32:559–567.