Dural arteriovenous fistulas (AVF) account for 10% to 15% of all intracranial vascular malformations.1,2 The overall annual risk of bleeding is approximately 1.5%.3 According to the Cognard classification,4–6 dural AVFs associated with leptomeningeal venous drainage or venous ectasia are considered to pose a high risk of haemorrhage.
Malignant dural AVFs, which are associated with cortical venous reflux, usually have an aggressive presentation, with a 35% risk of rebleeding within the first 2 weeks after the haemorrhage.7
Dural AVFs can be treated with surgery (endovascular treatment) or radiotherapy, the former being the treatment of choice in most cases.8,9 The direct transcranial approach through the parietal and mastoid foramina was developed by Houdart et al.10 Other authors11 have also described different surgical routes, including the dural sinus after craniectomy, the superior ophthalmic vein prior to surgical exposure, the cavernous sinus via the foramen rotundum, and the extracranial segment of the occipital arteries.
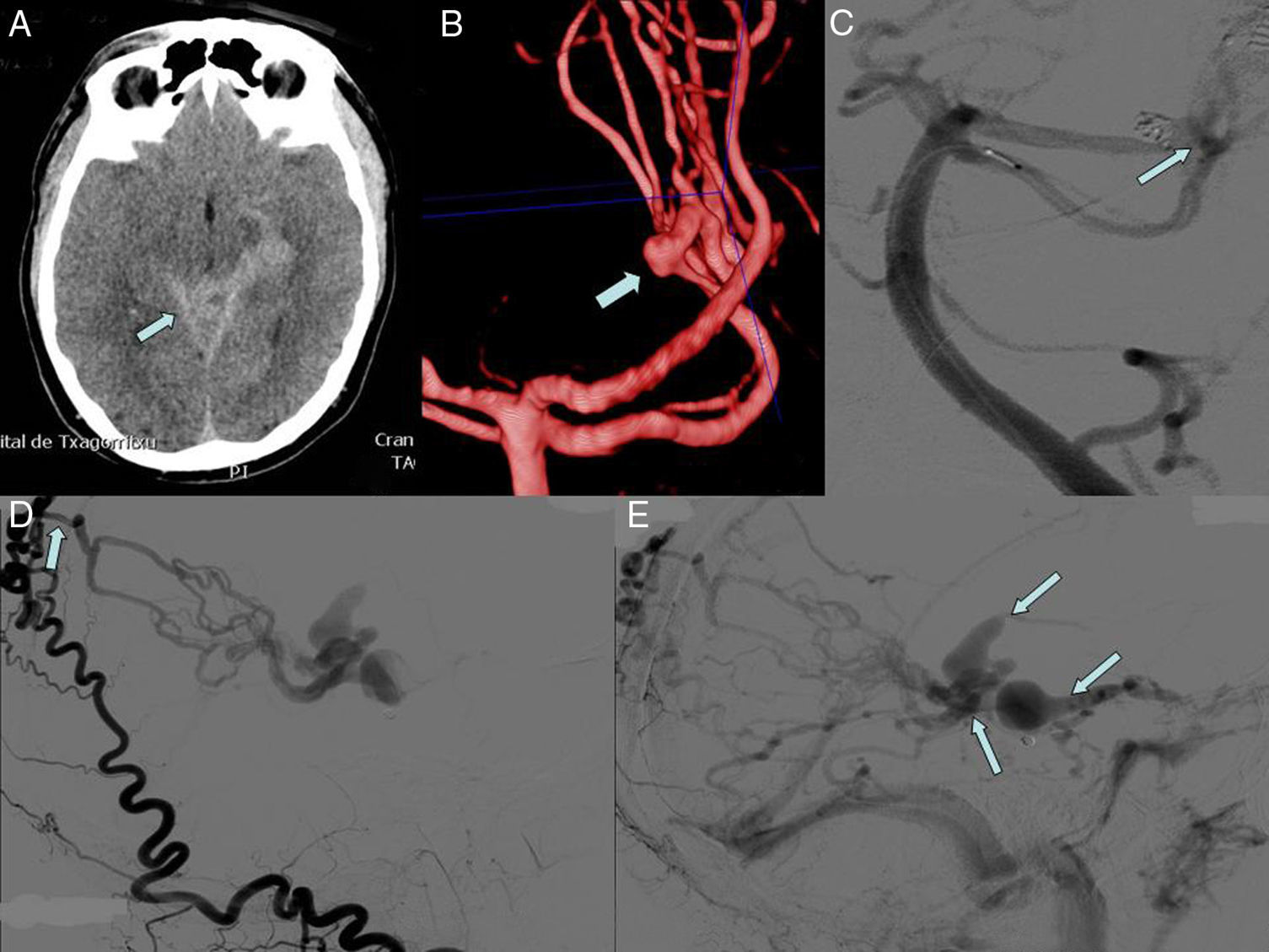
We present the case of a 56-year-old man with grade IV dural AVF according to the Cognard classification who displayed subarachnoid haemorrhage secondary to a ruptured flow-related aneurysm in the ascending artery (Fig. 1). The fistula, located near the tentorium, was supplied by both occipital arteries, the meningeal branches of the vertebral arteries, and the meningeal branches of the right internal carotid artery and the left superior cerebellar artery (the location of the aneurysm undergoing endovascular repair). The arteriovenous shunt was located medial to the attachment of the falx to the tentorium. We found large-calibre veins with retrograde flow draining to the straight sinus and signs of bilateral cortical reflux draining to the superior sagittal sinus.
(A) Cranial CT scan: subarachnoid haemorrhage at symptom onset. (B) 3D reconstruction based on CT: flow-related aneurysm in the left external carotid artery. (C) Aneurysm embolisation. (D) Angiography: arterial supply from the meningeal branches of the external carotid artery; the point where the occipital artery becomes intracranial can be seen. (E) Angiography: thick drainage veins with blood flow inversion and draining to the straight sinus.
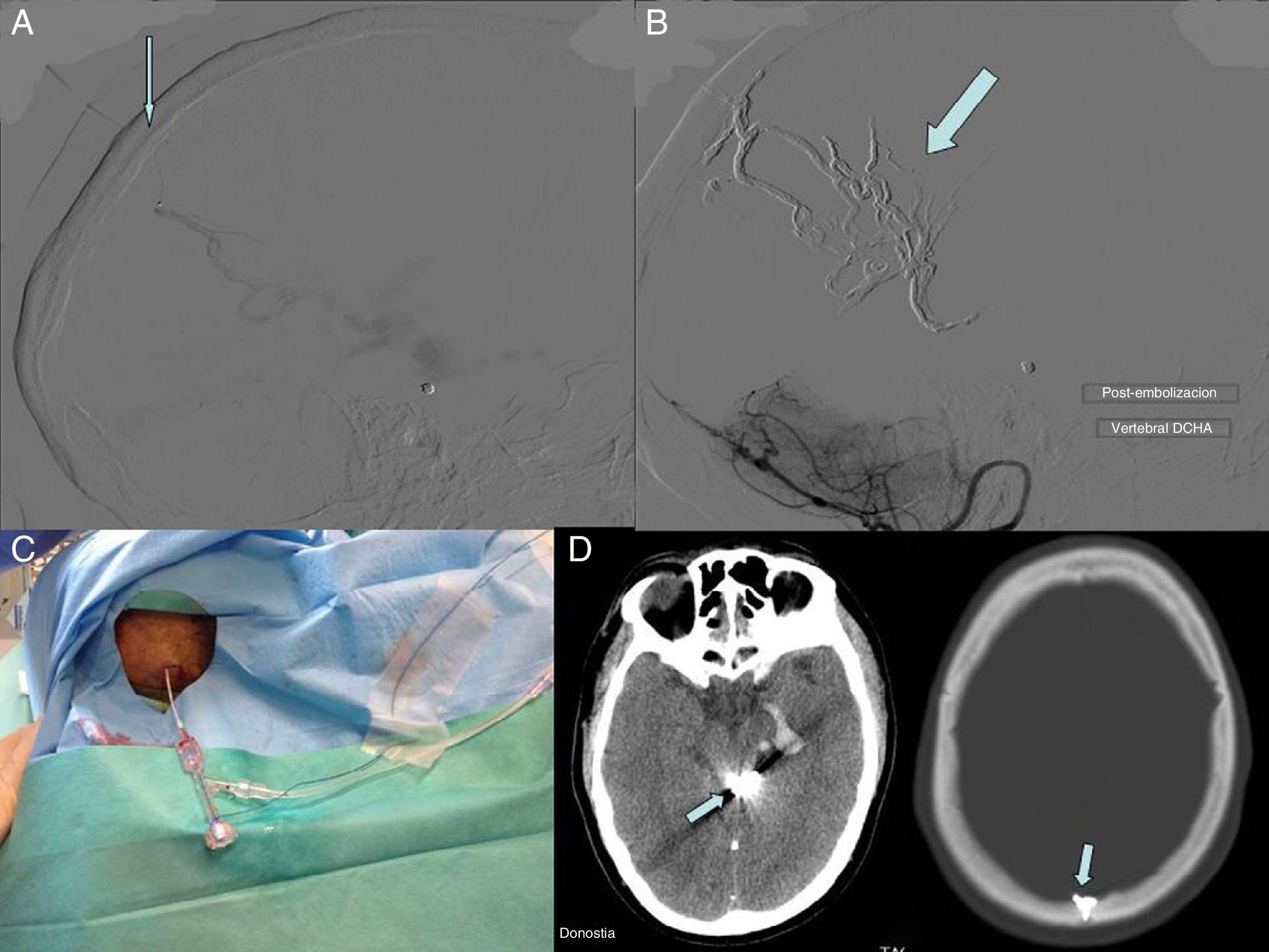
In view of the technical difficulties of performing distal catheterisation (marked elongation of the arteries ascending to the fistula and the tortuosity of the vein), we decided to perform a transcranial puncture of the right occipital artery through the parietal foramen (Fig. 2). After general anaesthesia was administered, the patient was placed in a prone position and the puncture was guided radiographically and angiographically. With an 18-gauge needle guided by direct fluoroscopy, a Marathon microcatheter (Covidien) was advanced to the arteriovenous shunt. After microcatheterisation we injected Onyx,8,12 which achieved complete occlusion of the AVF. The procedure was performed without incidents; at discharge, the patient remained asymptomatic.
In line with other studies,11,13 our case supports the hypothesis that the transcranial route is safe and effective when endovascular access is not viable due to blood vessel tortuosity.
In our view, a transcranial approach reduces treatment risks; in fact, it avoids the need for craniectomy. It also lowers the duration of the procedure and makes it easier to advance the microcatheter to reach the shunt location, which permits greater control over the injected liquid embolic agent.8,14 A possible complication specific to transcranial access is the formation of epidural or epicranial haematomas. The risk can be reduced by conducting a previous CT study of the foramen and performing the puncture using a map delivered by a catheter placed in the carotid.
In conclusion, transcranial puncture for the treatment of dural AVFs may be considered an effective endovascular technique when arterial or venous access is impossible or extremely complex.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Gonzalo N, Navia P, Larrea JA, Massó J. Punción transcraneal arterial microselectiva e inyección de Onyx para el cierre endovascular de fístula arteriovenosa dural. Neurología. 2016;31:505–507.