The clinical problems of patients with movement disorders (MD) are complex, and the duration and frequency of face-to-face consultations may be insufficient to meet their needs. We analysed the implementation of an e-mail-based query service for our MD unit's patients and their primary care physicians (PCPs).
MethodsWe retrospectively reviewed all consecutive emails sent and received over a period of 4 months, one year after implementation of the e-mail inquiry system. All patients received the e-mail address during consultations, and PCPs, during scheduled informative meetings. We recorded and later analysed the profile of the questioner, patients’ demographic and clinical data, number of queries, reason for consultation, and actions taken.
ResultsFrom 1 January 2015 to 30 April 2015, the service received 137 emails from 63 patients (43% male, mean age 71±10.5) diagnosed with Parkinson's disease (76%), atypical parkinsonism (10%), and others (14%); 116 responses were sent. Twenty (32%) emails were written by patients, 38 (60%) by their caregivers, and 5 (8%) by their PCPs. The reasons for consultation were clinical in 50 cases (80%): 16 (32%) described clinical deterioration, 14 (28%) onset of new symptoms, and 20 (40%) side effects or concerns about medications. In 13 cases (20%), the query was bureaucratic: 11 were related to appointments (85%) and 2 were requests for clinical reports (15%). In response, new appointments were scheduled in 9 cases (14%), while the rest of the questions were answered by email. Patients were satisfied overall and the additional care burden on specialists was not excessive.
ConclusionsImplementing an e-mail-based consultation system is feasible in MD units. It facilitates both communication between neurologists and patients and continued care in the primary care setting.
La problemática de los trastornos del movimiento (TM) es compleja y la duración y frecuencia de las consultas presenciales puede estar limitada por problemas de espacio y tiempo. Analizamos el funcionamiento de un servicio de atención por correo electrónico institucional para médicos de Atención Primaria (MAP) y pacientes en la Unidad de Trastornos del Movimiento (UTM).
MétodosSe revisaron retrospectivamente los correos electrónicos enviados y recibidos en un periodo de 4meses, un año tras su implantación. La dirección se proporcionaba en consulta y mediante sesiones informativas a los MAP del área. Se analizaron datos clínicos y demográficos de los pacientes, tipo de interlocutor, número de consultas, motivo y actuaciones derivadas de ellas.
ResultadosDel 1 de enero al 30 de abril de 2015 se recibieron 137 correos de 63 pacientes (43% varones; edad 71±10,5 años) diagnosticados de enfermedad de Parkinson (76%), parkinsonismos atípicos (10%) y otros (14%), y se enviaron 116 respuestas. En 20 casos (32%) fueron redactados por el paciente, en 38 (60%) por sus familiares y en 5 (8%) por MAP. Los motivos de consulta fueron clínicos en 50 casos (80%): deterioro clínico (16; 32%), nuevos síntomas (14; 28%), efectos secundarios o dudas sobre medicación (20; 40%). Como consecuencia, se adelantó una cita programada en 9 casos (14%), mientras que el resto se solucionaron por correo electrónico. En 13 (20%), el motivo de consulta fue burocrático: relacionado con citas (11, 85%) y solicitud de informe (2, 15%). La satisfacción fue generalizada, sin constituir una sobrecarga asistencial excesiva para los facultativos responsables.
ConclusionesLa implantación de una consulta por correo electrónico es factible en UTM, facilita la comunicación médico-paciente y la continuidad asistencial con Atención Primaria.
The use of e-mail in the doctor–patient relationship has numerous advantages. E-mail is fast, easy to use, inexpensive, and safe, offers a wide range of possibilities, and allows patients more time to reflect on the reason for consultation than do in-person consultations, strengthening continuity of care. E-mails are automatically saved, which helps patients to remember medical advice and provides physicians with a record of their clinical assessment and when it was made, improving the transmission of clinical data and diagnostic test results.1 Institutional e-mail accounts guarantee the protection of clinical data.
Diseases associated with movement disorders (MD) are frequently complex, and the duration and frequency of in-person consultations for these patients may be insufficient. Our movement disorders unit (MDU) decided to implement an institutional e-mail consultation service (e-consultation) within the management protocol for Parkinson's disease (PD) effective in the Region of Madrid2 to improve healthcare and continuity of care with primary care physicians. This study analyses the service and identifies potential areas of improvement to adapt healthcare to the needs of our patients and their general practitioners (GP).
MethodsThis retrospective, observational, descriptive study analyses our experience with e-consultation for GPs and patients of the MDU. Descriptive statistics are used to present data on the variables analysed.
The management and referral protocol for patients with PD in the Region of Madrid2 was designed in 2012 by a multidisciplinary team including neurologists, internists, GPs, psychiatrists, and geriatricians, among others. This protocol included the implementation of systems for information-sharing and communication between primary care departments and MDUs by means of institutional e-mail accounts.
Members of the MDU at our tertiary hospital presented the protocol at our health district's primary care centres between December 2013 and April 2014, informing staff of the institutional e-mail address for electronic primary care consultations. The protocol was implemented in December 2013. Patients were also systematically informed about the new service at in-person consultations; this information appeared in the patients’ clinical reports and referral notes.
Our MDU, which includes 4 specialists in MD, cares for a total of 1109 patients per year, and offers consultations 5 days a week.
We retrospectively reviewed all e-mails sent and received during a 4-month period (January to April 2015), one year after the e-consultation service was fully implemented.
We analysed the patients’ clinical and demographic characteristics and recorded the type of informant, number of e-mail consultations, reason for consultation, and consultation outcomes.
A neurologist specialising in MD replied to all e-mails within 24hours (from Monday to Friday, excluding public holidays). Replies were sent before the opening time for in-personal consultations. The neurologist had access to the patients’ electronic medical records. Any noteworthy interventions were registered in the patients’ medical records.
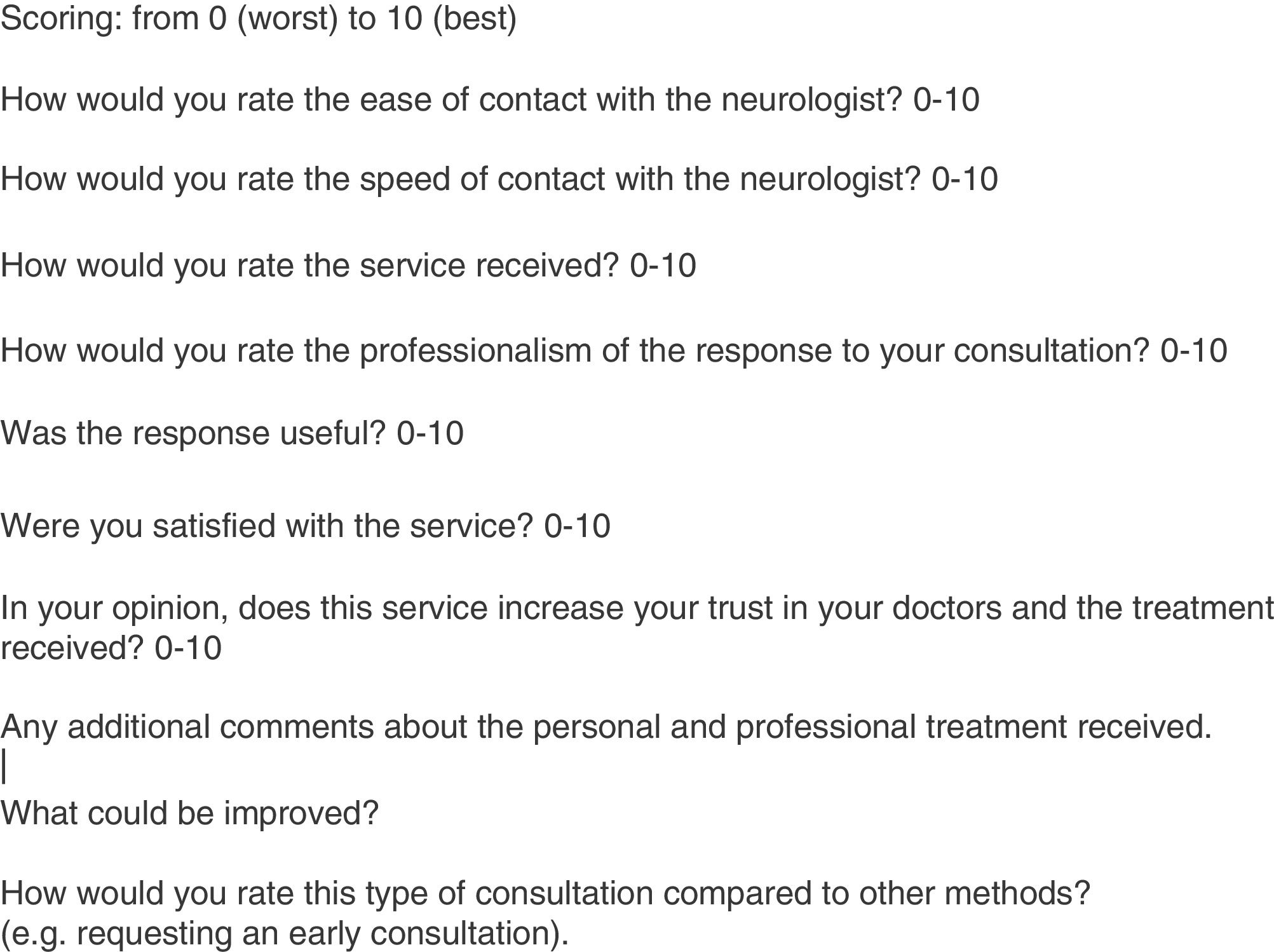
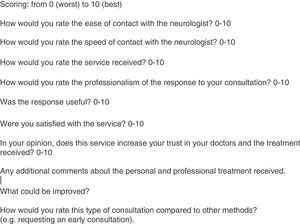
A satisfaction survey was e-mailed to all users of the e-consultation service during the study period (Fig. 1).
ResultsBetween 1 January and 30 April 2015, we received 137 e-mails regarding 63 patients (43% were men; mean age of 71±10.5 years) and sent 116 replies. We received a mean of 1.65 e-mails per weekday and registered a total of 87 episodes (mean, 1.36; median, 1; range, 1–5).
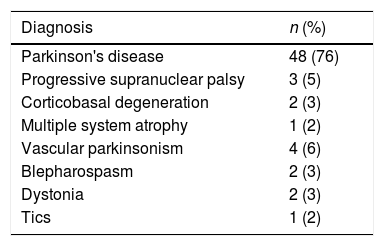
Patients’ diagnoses were PD (76%), atypical parkinsonism (10%), and other disorders (14%) (Table 1).
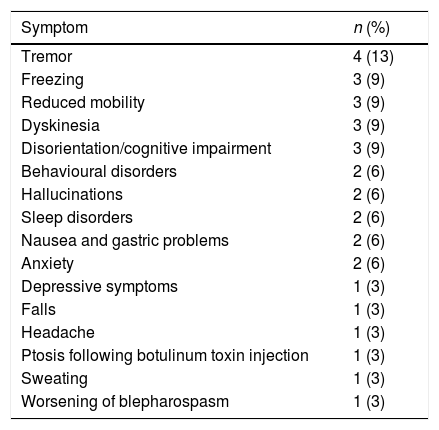
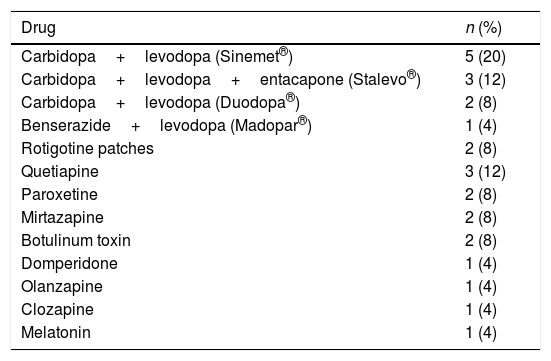
E-mail consultations were written by the patients themselves in 20 cases (32%), by a relative in 38 (60%), and by the patient's GP in 5 (8%). The reasons for consultation were clinical in 50 cases (80%), of which 16 (32%) reported clinical deterioration, 14 (28%) reported new symptoms, and 20 (40%) reported secondary effects or asked questions about the patient's medication (Tables 2 and 3).
Symptoms leading to e-mail consultations.
| Symptom | n (%) |
|---|---|
| Tremor | 4 (13) |
| Freezing | 3 (9) |
| Reduced mobility | 3 (9) |
| Dyskinesia | 3 (9) |
| Disorientation/cognitive impairment | 3 (9) |
| Behavioural disorders | 2 (6) |
| Hallucinations | 2 (6) |
| Sleep disorders | 2 (6) |
| Nausea and gastric problems | 2 (6) |
| Anxiety | 2 (6) |
| Depressive symptoms | 1 (3) |
| Falls | 1 (3) |
| Headache | 1 (3) |
| Ptosis following botulinum toxin injection | 1 (3) |
| Sweating | 1 (3) |
| Worsening of blepharospasm | 1 (3) |
Main drugs involved in e-consultation queries.
| Drug | n (%) |
|---|---|
| Carbidopa+levodopa (Sinemet®) | 5 (20) |
| Carbidopa+levodopa+entacapone (Stalevo®) | 3 (12) |
| Carbidopa+levodopa (Duodopa®) | 2 (8) |
| Benserazide+levodopa (Madopar®) | 1 (4) |
| Rotigotine patches | 2 (8) |
| Quetiapine | 3 (12) |
| Paroxetine | 2 (8) |
| Mirtazapine | 2 (8) |
| Botulinum toxin | 2 (8) |
| Domperidone | 1 (4) |
| Olanzapine | 1 (4) |
| Clozapine | 1 (4) |
| Melatonin | 1 (4) |
The reasons for consultation in the remaining 13 cases (20%) were administrative, related to appointments in 11 cases (85%) and requesting reports in 2 (15%). Appointments had to be moved forward following e-consultations in 9 cases (14%); the remaining problems were solved by e-mail.
Thirty users (47%; 9 patients, 19 relatives, and 2 GPs) completed the satisfaction survey; a high level of satisfaction was seen across all types of informant (Fig. 1). Users rated the service on a scale from 0 to 10, as follows: ease of contact with the neurologist, 9 (p25-p75: 8-10); speed of contact, 8 (8-9); service received, 9 (9-10); professionalism, 9 (8-10); usefulness of response, 8 (8-10); and level of satisfaction, 9 (8–10). Users rated their trust in their physician and the treatment received 9/10 (8-10).
Most users preferred e-consultation over other forms of consultation due to its effectiveness and ease of use, and valued its availability and the fact that recommendations are given in writing. However, some patients stated that they preferred voice recordings due to difficulties using keyboards. One patient suggested using video calls to replace in-person consultations.
DiscussionThis study analyses our experience with e-consultation for GPs and MDU patients.
We feel that our sample is representative of the 2 target populations (patients and GPs), although our data show that patients and relatives are the most frequent users. The volume of consultations was considerable but did not significantly increase neurologists’ workload (a mean of 1.65 e-mails per weekday).
According to our results, the reason for e-mail consultation was clinical in most cases; questions about medication (adverse effects, doses, dosage information) were very frequent. The drugs associated with e-mail consultations were those traditionally indicated for PD; nearly half of patients were receiving levodopa preparations (e.g. Duodopa®) (Table 3). The symptoms leading to e-mail consultations with neurologists were typical PD symptoms, especially those occurring in advanced stages: freezing, motor fluctuations, dyskinesia, and neuropsychiatric complications (Table 2).
E-consultation has numerous advantages. Firstly, the tool may reduce the impact or incidence of drug adverse effects since it allows early dose adjustment or drug switching. The system may also improve treatment adherence as it allows neurologists to more rapidly solve patients’ doubts about treatment, which is often complex in MD. Clinical worsening or the onset of new symptoms were also frequent reasons for consultation; in most cases, these problems could be solved by e-mail, reducing the number of rescheduled appointments and visits to the emergency department.
This practical, convenient system is most probably less costly than in-person consultations (saving the costs associated with transportation, ambulances, and work absences on behalf of patients’ relatives) and reduces the costs associated with emergency care and iatrogenesis. Further studies into the socioeconomic impact of this system are necessary to confirm this hypothesis.
Strikingly, only 32% of e-mails were sent by the patients themselves. This may be due to advanced age, difficulty using a keyboard, or cognitive impairment.
Users reported a high level of satisfaction with the service. Replying to e-mails did not significantly increase neurologists’ workload since they had access to the patients’ electronic medical records.
Few studies have addressed this topic, and have mainly focused on e-mail communication between GPs and specialists, which in many cases enables patient referral to be avoided. These studies have reported satisfactory results, mainly improved access to specialised care (shorter waiting times) and a decrease in healthcare costs (avoiding unnecessary referrals to specialists).3–10 Keely et al.4 reported their experience with an e-consultation service between GPs and a wide range of specialists (both clinical medicine and surgery specialists) in Ottawa, Canada. Similarly to our approach, these researchers recorded the activity of the service for 14 months; they analysed all consultations and replies, the outcomes of these consultations, and GPs’ satisfaction according to the results of a satisfaction survey. In the study by Keely et al., users reported a high level of satisfaction, and referrals were avoided in half of the cases.
The novelty of our e-consultation service resides in that patients (and their relatives) are its main users, which promotes patients’ independence and increases their control over their disease; this is especially valuable in the context of chronic diseases. Much emphasis is currently being placed on educating patients about their disease and promoting active involvement, helping them understand their health behaviour and develop strategies to live as fully and productively as possible; this is known as patient self-management training. This, in turn, promotes patient empowerment by engaging patients in their treatment and developing and stimulating their skills.11–14
Our study has several limitations, including the fact that the study period comprised 4 randomly chosen months (seasonal factors may have an impact on the use of the e-consultation service) and the low participation in the satisfaction survey (under 50% of users). This low response rate may have biased our results on user satisfaction: the survey may have been completed by satisfied users only. Another limitation of our study is that the survey was not anonymous (it was sent by e-mail), which may also have biased user satisfaction results.
Lastly, the inclusion of a control group with no access to the e-consultation service may have been useful to analyse differences in such variables as the incidence of drug adverse reactions, costs, visits to the emergency department, and user satisfaction. E-consultation may also be compared to other means of consultation, such as telephone consultations, to analyse these variables.
ConclusionsIn our experience, implementing an e-consultation service in MDUs is a viable option since it does not significantly increase specialists’ workload and results in high user satisfaction. E-consultation is a useful tool for improving patient-neurologist communication and the continuity of primary care.
FundingThis study received no funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Viedma-Guiard E, Agüero P, Crespo-Araico L, Estévez-Fraga C, Sánchez-Díez G, López-Sendón JL, et al. El correo electrónico en la consulta de Parkinson: ¿soluciones a un clic? Neurología. 2018;33:107–111.
This study was featured as an oral presentation at the 67th Annual Meeting of the SEN, 2015.