Central hearing disorders are highly infrequent entities due to the extensive bilateral projection of the auditory system to both temporal lobes.1,2
They are characterised by the inability to understand verbal and non-verbal sounds, while reading and writing abilities are preserved.3
The most frequent cause is cerebrovascular accident, followed by infection, trauma, or tumours.
Four different mechanisms may lead to central hearing disorders: (1) extensive damage affecting both primary auditory cortices, which is the most frequent cause according to the literature;4 (2) a unilateral lesion to the primary auditory cortex associated with other lesions to the associative pathways; (3) cortical/subcortical lesions to both hemispheres affecting auditory pathways; (4) a single lesion to the temporal lobe that disconnects Wernicke area from its auditory afferents.5
According to their symptoms, central hearing disorders are classified into 3 categories.5 The first is cortical deafness, characterised by an inability to understand both verbal and non-verbal sounds despite the preservation of the peripheral auditory system. It is usually caused by an extensive lesion to both primary auditory cortices. Patients present hearing loss but preserve the ability to read and write, which differentiates them from patients with severe sensory aphasia. One-third of these patients will develop word deafness.4
The second category is non-verbal auditory agnosia, characterised by an inability to understand isolated specific sounds (e.g., birdsong). It is caused by a lesion to the right temporal cortex.5
The third is word deafness, which affects the understanding of spoken language, while writing and reading abilities are preserved. The most frequent cause is bilateral damage to the superior temporal gyri, sparing the primary auditory cortices.6 Patients frequently present phonemic paraphasia and behavioural alterations.
Case reportWe present the case of a 58-year-old man with several years' history of arterial hypertension and hypertensive heart disease with left ventricular dilation.
He visited the emergency department due to sudden-onset bilateral hearing loss as the only symptom. An initial neurological assessment revealed inability to understand speech, with preserved reading, writing, and speaking abilities, and some degree of phonemic paraphasia, inattention, and restlessness. The otorhinolaryngology department performed a tone audiometry study that revealed moderate sensorineural hearing loss. A speech therapist administered the Mississippi Aphasia Screening Test (MAST), which showed severely impaired understanding of oral commands but acceptable understanding of written commands.
A cranial CT scan showed right temporal hypodensity (Fig. 1).
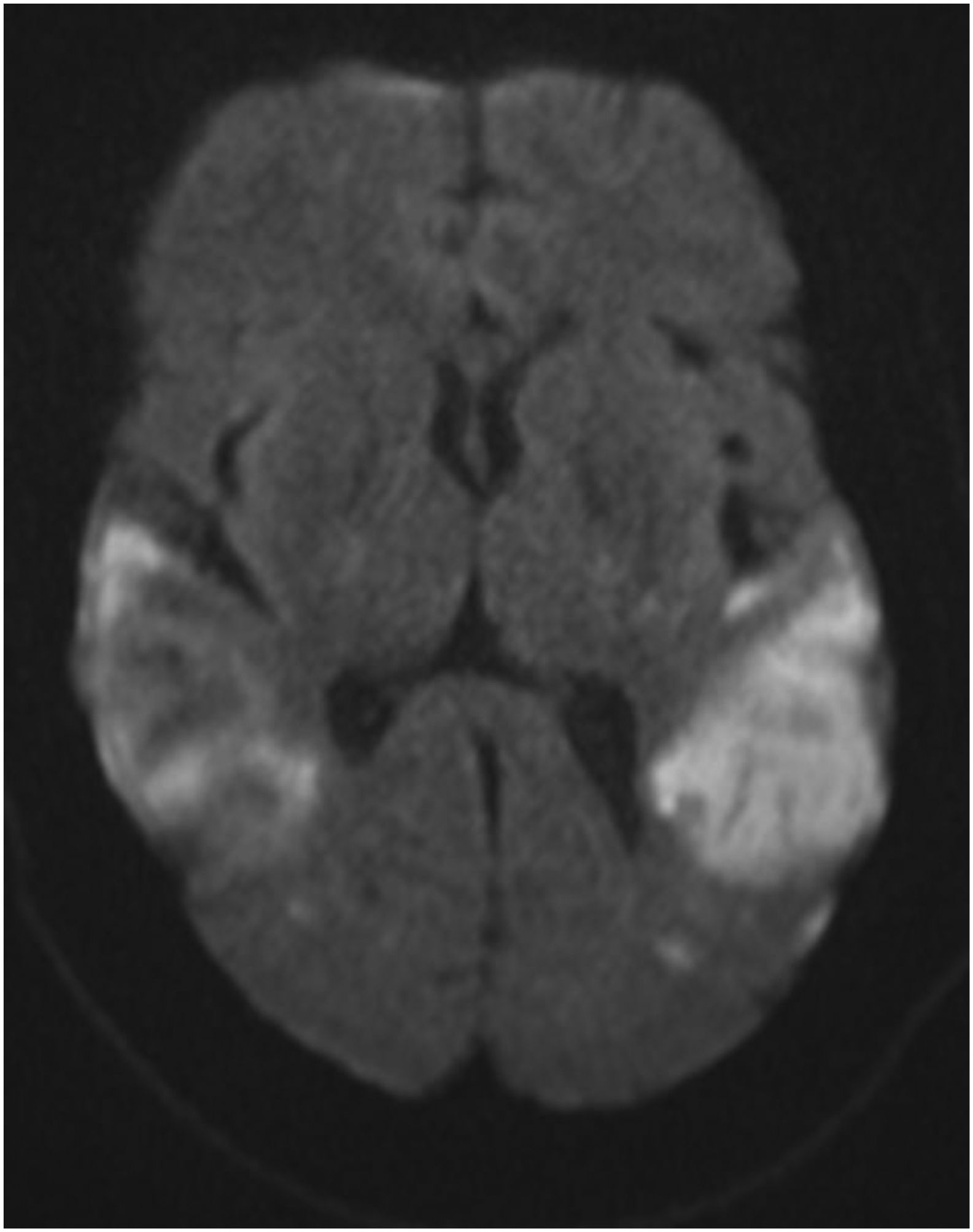
The study was completed with a brain MRI study, which revealed late subacute temporal lobe stroke on the right side, and early subacute stroke on the left; lesions affected both superior temporal gyri but spared the primary auditory cortex (Fig. 2).
Holter monitoring yielded normal results and a transthoracic echocardiography confirmed dilated cardiomyopathy with left ventricular ejection fraction <30%. Administration of anticoagulation therapy was agreed with the cardiology department.
The final diagnosis was bilateral temporal infarction of probable cardioembolic origin, causing an auditory deficit suggestive of pure word deafness.
DiscussionCentral hearing disorders are very infrequent, as they are only caused by extensive bilateral damage to auditory projections in the brain. Vascular aetiology is the most frequent cause, with a first silent temporal stroke followed years later by a second event in the contralateral temporal area, resulting in the manifestation of the hearing loss.7
Contrary to the literature reports, our patient presented strokes in both temporal lobes with similar onset times, which makes our case even more unusual.
According to the symptoms, our case may be classified as pure word deafness (pure verbal deafness), as we observed difficulty in understanding speech but preserved writing and reading abilities, fluent speech with phonemic paraphasia, aggressiveness, and disinhibition.6 Furthermore, neuroimaging revealed involvement of both superior temporal gyri and preserved primary auditory cortex bilaterally; this is consistent with other reported cases.6
ConclusionsDue to the complexity of the auditory cortex and its variability between individuals, as well as the considerable clinical similarity with language disorders, word deafness is underdiagnosed. However, it should be suspected in those patients who, as our case, present difficulties in understanding speech with intact writing and reading abilities. Multidisciplinary management by the neurology, speech therapy, and rehabilitation departments is essential to achieve the maximum recovery possible.
FundingThis study has received no funding of any kind.
Informed consentThis study contains no data or images that may identify the patient; therefore, in accordance with the journal's requirements for publication, no informed consent is provided.
Ethical considerationsThis study involves no experiments with humans.