Subacute combined degeneration and megaloblastic anemia are two complications that result from vitamin B12 deficiency, both being potentially reversible if an early diagnstic and replacement of cobalamin is performed. In the first entity, there are dorsal columns and medullary spinothalamic tracts dysfunctions secondary to a process of demyelination due to synthetic defects in the myelin sheaths. As for the second entity, it courses with hematologic manifestations characterized by macrocytic anemia, and it can coexist with other alterations of both the myeloid and megakaryocytic lineage.
We report a case of simultaneous subacute combined degeneration and megaloblastic anemia as well as a brief literature review.
Clinical caseA 56-year-old man, mestizo, with past medical history significant only for hypertension in treatment with losartan, presented to our clinic for a 4-month history of ascending progressive weakness of all extremities to the point where he was unable to stand or walk, associated to acral paresthesias and micturition difficulty. He presented to the emergency department for worsening symptoms. On examination, there was mucocutaneous pallor, quadriparesis with mild spasticity, normal reflexes without clonus, bilateral Babinski sign, hand and feet hypoesthesia, apallesthesia, altered proprioception predominantly in the lower limbs and rectal sphincter hypotonia, he was unable to stand, thus impossible to assess his gait. The syndromatic approach suggested a possible myelopathy of unknown origin, therefore laboratory studies, an electromyography (EMG), and a contrast MRI (magnetic resonance imaging) of the column were ordered.
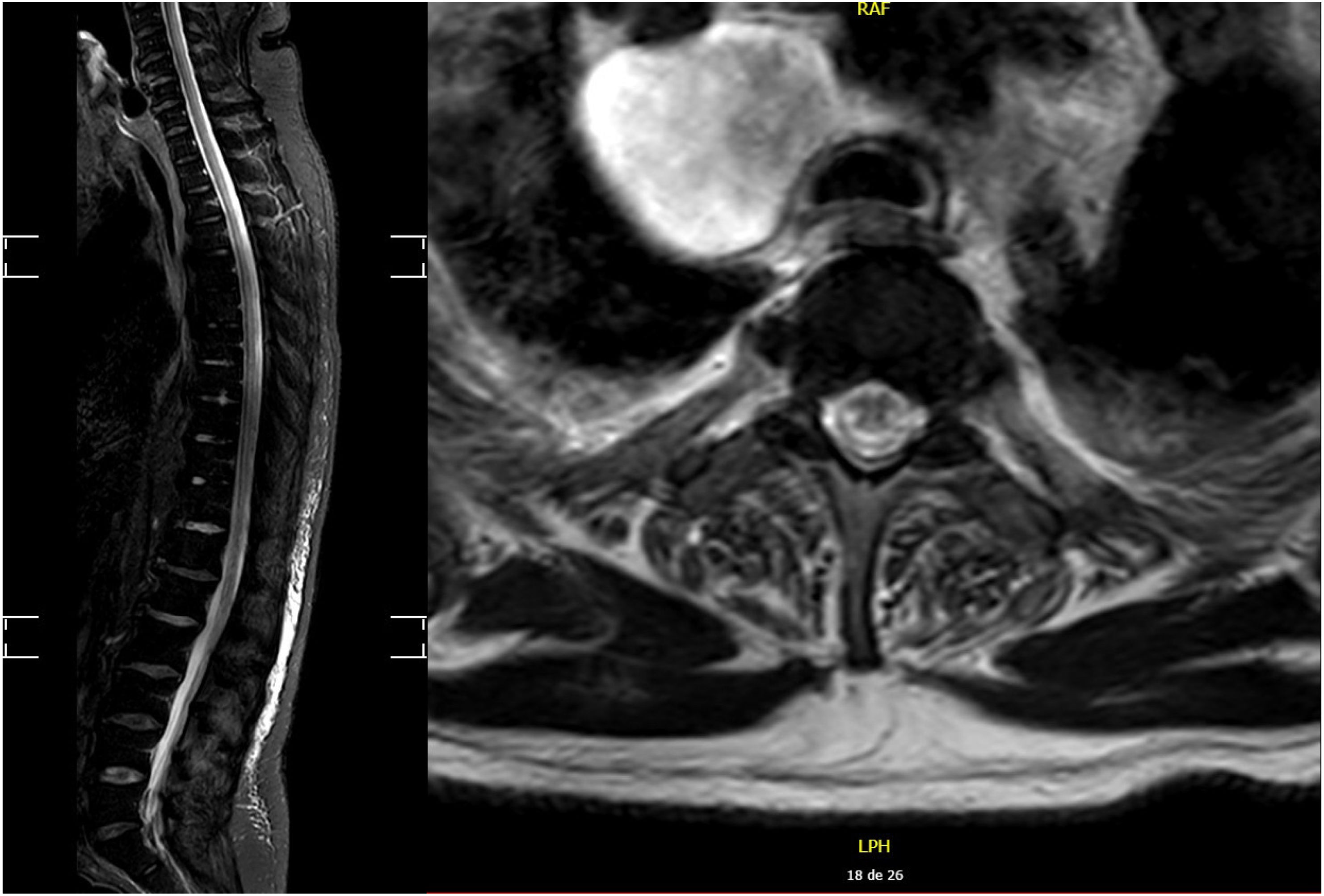
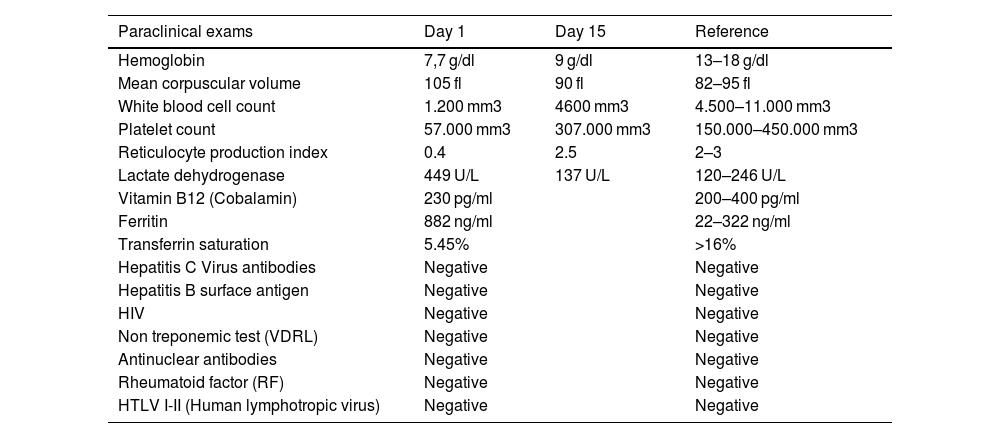
Initial laboratory findings are shown in (Table 1), which demonstrated pancytopenia, for which additional tests were ordered. The EMG revealed a four extremity, pure sensory axonal neuropathy, nevertheless, it only explained the sensitive symptoms, not the motor ones. The MRI (Fig. 1) showed an extensive longitudinal myelitis, from C2 until the conus medullaris, with bilateral and symmetric, posterior and lateral cord involvement, with no contrast enhancement; derived from this finding, additional serum tests were ordered (Table 1), ruling out an infectious, autoimmune or paraneoplastic etiology. It was noted that vitamin B12 levels were within normal limits (200–300 pg/mL), however, it was thought of the possibility that both the pancytopenia and the myelopathy could be explained by the same origin, and homocysteine and methylmalonic acid (MMA) levels were ordered, whose values were 26 μmol/L (normal: 5.56–16.2 μmol/L), and 350 nmol/L (normal: 73–270 nmol/L), respectively; meaning a clear vitamin B12 deficiency. Additionally, anti-intrinsic factor antibodies were ordered, which came back elevated (16.2 U/ml; normal: <6 U/ml); and an upper gastrointestinal endoscopy, which showed atrophic gastritis in the body and fundus. All of the above makes up the diagnstic of subacute combined degeneration, pure sensory axonal neuropathy and pancytopenia secondary to vitamin B12 deficit caused by pernicious anemia. It was initially treated with intramuscular cyanocobalamin together with folic acid.
Laboratory results showing the progression before and after treatment.
| Paraclinical exams | Day 1 | Day 15 | Reference |
|---|---|---|---|
| Hemoglobin | 7,7 g/dl | 9 g/dl | 13–18 g/dl |
| Mean corpuscular volume | 105 fl | 90 fl | 82–95 fl |
| White blood cell count | 1.200 mm3 | 4600 mm3 | 4.500–11.000 mm3 |
| Platelet count | 57.000 mm3 | 307.000 mm3 | 150.000–450.000 mm3 |
| Reticulocyte production index | 0.4 | 2.5 | 2–3 |
| Lactate dehydrogenase | 449 U/L | 137 U/L | 120–246 U/L |
| Vitamin B12 (Cobalamin) | 230 pg/ml | 200–400 pg/ml | |
| Ferritin | 882 ng/ml | 22–322 ng/ml | |
| Transferrin saturation | 5.45% | >16% | |
| Hepatitis C Virus antibodies | Negative | Negative | |
| Hepatitis B surface antigen | Negative | Negative | |
| HIV | Negative | Negative | |
| Non treponemic test (VDRL) | Negative | Negative | |
| Antinuclear antibodies | Negative | Negative | |
| Rheumatoid factor (RF) | Negative | Negative | |
| HTLV I-II (Human lymphotropic virus) | Negative | Negative |
After just 15 days of treatment, all blood counts improved drastically until finally reaching normal levels.
At six months follow up, the patient could stand and walk, although with instability and the need for constant support. No new hematological abnormalities were documented.
DiscussionSubacute combined degeneration is a condition that affects the posterior and lateral columns of the spinal cord, derived from a demyelination process caused by the deficit of cobalamin, which entails a series of hematological and neurological manifestations.1
Vitamin B12 is used as a cofactor for two essential enzymes, both for synthesis of myelin and hematological products: homocysteine methyltransferase and methylmalonyl-coa mutase. The former turns homocysteine into methionine, which is the precursor for S-adenosylmethionine, required for the maintenance of myelin sheaths and synthesis of purine bases. Additionally, the second enzyme makes succinyl-Coa from methylmalonyl-Coa, a necessary step for the synthesis of myelin, therefore, the absence of these processes, results not only in an altered myelin synthesis but also in the incorporation of abnormal lipids. Consequently, a demyelination process takes place. Furthermore, the altered production of purine bases affects DNA repair processes leading to an abnormal cytoplasmic cellular maturation demonstrated by the nuclear-cytoplasmic dissynchrony, which is the basis for an inefficient erythropoiesis and megaloblastic changes in the bone marrow.2–4
The pathological changes that occur in subacute combined degeneration encompass a multifocal and diffuse demyelination process along with axonal loss, specially in the spinal white matter. These changes are seen predominantly in the posterior columns (proprioception and vibration), lateral corticospinal tracts (movement) and, occasionally, in the spinothalamic tracts (pain and temperature sensitivity).5
Neurological syndromes potentially associated to vitamin B12 deficit include: myelopathy, neuropathy, neuropsychiatric abnormalities, and less frequently, optic nerve atrophy. Nevertheless, there's no clear description of the relative distribution of each condition, it is only described that around 25% of patients with cobalamin deficit course with peripheral neuropathy, but this data is not established in other conditions, therefore we're unaware of their exact frequency and in what degree they appear simultaneously, as described in our case, which coursed with sensory neuropathy and myelopathy.6,7 It can be inferred by the study carried out by Krishan et al. that of patients with subacute combined degeneration, only 14% could show altered signal on MRI, which demonstrates a low sensitivity for a clear documentation of this condition and thus the difficulty to establish the diagnóstico.8
Subacute combine degeneration will demonstrate a series of clinical and semiological findings according to the spinal cord involvement. In case of dorsal columns' affection: discriminatory touch, and proprioception and vibration will be altered; in case of lateral corticospinal tract dysfunction: paresis, hyperreflexia, spasticity and Babinski sign will predominate as manifestations of upper motor neuron syndrome; and in more severe cases, sphincter dysfunction will be present.1 It's interesting to note that various studies suggest that the degree of the hematological changes is inversely proportional to the neurological involvement,4,7,9 however, in this case both were markedly severe and simultaneous.
Even though the estimated sensitivity of tests that measure vitamin B12 levels is around 95%, up to 10–20% can have normal levels, which is why it is only possible in such cases to identify the true deficiency by measuring methylmalonic acid (MMA) and homocysteine levels, which would be high in case of cobalamin deficiency. All of the above is explained under certain conditions that alter and falsely exhibit normal or high levels of cobalamin, for instance, occult malignancies, myeloproliferative neoplasms, alcoholic liver disease, renal disease and some inborn errors of metabolism, but the most significant scenario is in context of pernicious anemia, where anti-intrinsic factor antibodies compete with vitamin B12 to bind with the binding protein used during the chemiluminescence technique, this antibodies being interpreted as cobalamin, resulting in erroneously normal or high values,10,11 this phenomenon occurred in this case and only by measuring homocysteine and MMA could the deficiency be confirmed.
Normally, in most patients cobalamin replacement stops the progression and results in radiological and neurological improvement, besides the normalization of the hematological abnormalities. Notwithstanding, the neurological recovery's magnitude depends on the degree of initial involvement, entailing that 86% show partial improvement and only 14% achieves complete neurological recovery. Some characteristics associated with better prognosis and neurological outcomes after the start of treatment are described, such as: being under 50 years of age, short course of disease, no sensory deficit, Romberg and Babinski sign not present, less than 7 medullary segments affected on MRI and no medullary atrophy.12,13 In our case, the patient was over 50 years old, severe neurological impairment and large longitudinal compromise on MRI, which conferred a poor prognosis for neurological recovery, however, he has presented slight improvement achieving standing position and walking with support.
In light of the above, the intention of this description is to emphasize the importance of early identification of a potentially reversible cause of myelopathy and pancytopenia, taking into account that vitamin B12 deficiency is highly prevalent in developing countries, such as ours, with prevalences as high as 40% being recorded.14 The appropriate request and interpretation of diagnostic tests is crucial for the establishment of therapeutic measures and thus have a positive impact on this entity.
Informed consentVerbal and written consent was obtained, in addition to approval by the institution's research and ethics committee.