The transition from paediatric to adult neurology consultations in patients with epilepsy must be understood as a process in which the patient acquires independence in the management of their disease and faces new issues related to adulthood. The aim of this study is to gather the opinion of experts in epilepsy on this transition in order to issue recommendations.
MethodsUsing a Delphi consensus process, 54 paediatric and adult neurologists with expertise in epilepsy expressed their degree of agreement on 38 statements on about the transition from paediatric to adult consultations, grouped into the following sections: (1) preparation and moments prior to transition; (2) transition process; and (3) moments after the transition and follow-up.
ResultsAfter 2 rounds, consensus was reached for 33 statements (86.8%). For the remaining 5 statements (13.2%), there was neither agreement nor disagreement. Among the subjects for which consensus was strongest was the involvement of the patient and family, who must be provided sufficient information to resolve their doubts and concerns. Before referral, the clinical report must be reviewed to ensure that it contains all relevant information on the disease. During the first follow-up visits after the transition, the patient's knowledge should be brought up to date in order to promote their autonomy.
ConclusionThe clinical report, early preparation, and complete case review are considered fundamental in the process of transition from paediatric to adult neurology care.
La transición desde neuropediatría a las consultas de neurología para adultos en pacientes con epilepsia ha de entenderse como un proceso en el que el paciente adquiere una independencia en el manejo de la enfermedad y afronta nuevos aspectos relacionados con la edad adulta. El objetivo de este estudio es conocer la opinión de expertos en epilepsia sobre esta transición para poder ofrecer recomendaciones.
MétodosMediante un consenso Delphi, 54 neuropediatras y neurólogos expertos en epilepsia mostraron su grado de acuerdo en 38 aseveraciones sobre la transición de pediatría a la consulta de adultos agrupadas en los siguientes bloques: 1) preparación y momento previo a la transición; 2) durante la transición; y 3) momento posterior a la transición y seguimiento.
ResultadosTras dos rondas, se alcanzó un consenso en el acuerdo en 33 aseveraciones (86,8%). En las 5 aseveraciones restantes (13,2%) no hubo ni acuerdo ni desacuerdo. Entre los acuerdos más importantes destaca la implicación del paciente y la familia a los que es necesario aportar información suficiente para disipar sus dudas y miedos. Antes de la derivación, se ha de comprobar que el informe clínico contiene toda la información relevante de la enfermedad. Durante las primeras visitas de seguimiento tras la transición, se han de actualizar los conocimientos de los pacientes para lograr su autonomía.
ConclusiónEl informe clínico, la preparación anticipada y la revisión completa del caso se consideran fundamentales en el proceso de transición de pediatría a la consulta de adultos.
Epilepsy incidence peaks during childhood and adolescence.1–3 The Spanish 2nd National Strategic Plan for Childhood and Adolescence 2013–2016 (II PENIA, for its Spanish initials) establishes a cut-off age of 18 years for the transition from paediatric to adult care.4 However, given the discrepancies between autonomous communities in human and material resources, and with hospitals and primary care centres not yet compliant with this plan, nationwide implementation of this limit is a challenge; in practice, cut-off ages range from 14 to 18 years, hindering the homogenisation of paediatric care in Spain.
This care transition should be understood not merely as the administrative procedure of transferring a patient and their records, but rather as a process in which the patient gains independence to self-manage the control and follow-up of their disease, in a joint undertaking between the patient, the paediatric neurologist, and the neurologist.5,6 During this transition, it is important that we recognise both changes in the patient and the new social demands and situations they will face, and the progression of epilepsy, from both a clinical and an electroencephalographic perspective.7,8 Therefore, every case should be assessed on an individual basis, also reviewing the patient's social, educational, psychological, and psychiatric situation.9
Several authors have developed models to facilitate the care transition of children with epilepsy when they reach adolescence.10–12 All of these emphasise the need for clinical records to include specific data on the process of epilepsy, social/family aspects, the family's level of understanding of and involvement in the process, and the patient's level of education and leisure activities. This information will enable tailored management of each patient, with treatment and follow-up adapted to their personal circumstances.10–12
In Spain, no guidelines are currently available for this transition from paediatric to adult care at epilepsy clinics. For this reason, we designed the present study, a consensus statement developed using the Delphi method, aiming to establish the opinions of a group of experts on epilepsy regarding this healthcare transition, with a view to identifying issues that remain unresolved and establishing recommendations on the following matters: (a) identifying and establishing protocols to assist specialists in transferring patients from paediatric to adult epilepsy care; and (b) offering guidelines for clinicians participating in or who have patients in this situation, in order to improve the circumstances of these patients and their families.
MethodsStudy designThe study design was based on the Delphi method, a prospective, structured communication technique that seeks to explore and unify the opinions of an expert group on a complex or controversial subject for which insufficient evidence is available or that is not fully or clearly understood. It avoids the difficulties and disadvantages inherent to in-person discussion and consensus processes, such as the need for travel, bias due to influence, or the lack of confidentiality.13,14
The study was conducted in several phases: (1) conception of the project and formation of a scientific committee of experts; (2) creation of a Delphi questionnaire with the controversies deemed most relevant regarding the transition from paediatric to adult epilepsy care; (3) 2 successive rounds of evaluation to gather the opinions of an expert panel; and (4) compilation, analysis, and discussion of the results in order to establish a series of conclusions.
ParticipantsThe study included 3 types of participants: the scientific committee, a technical team, and an expert panel. The former group comprised 7 physicians (4 paediatric neurologists and 3 adult neurologists) with experience in the treatment of epilepsy in children and adults, and was responsible for drafting the Delphi questionnaire. Three members also acted as coordinators, one for each phase of the project. The technical team was formed by the company LET'S HEALTH SL. The team directed and supervised the entire process and was responsible for the instrumental implementation of the method (distribution of the Delphi questionnaire, analysis of responses, and statistical analysis of the consensus). The expert panel was selected by the scientific committee, and was made up of 54 neurologists and paediatric neurologists with recognised clinical experience in epilepsy and in the process of transferring patients from paediatric to adult neurological care. The selection of members of the expert panel sought to adequately represent all autonomous communities of Spain.
Delphi questionnaireThe scientific committee developed a Delphi questionnaire comprising 38 statements, grouped into 3 sections, addressing the most relevant controversies on the 3 phases of the transition from paediatric to adult care: (1) preparation of the patient at the paediatric neurology clinic and the moments prior to transition to adult neurology care (11 statements); (2) transition process (11 statements); and (3) moments after transition to adult neurology care and follow-up by the adult neurology clinic (16 statements).
Statements on the questionnaire were rated with a single 9-point Likert-type scale (1 point: completely disagree; 9 points: completely agree), according to the RAND/UCLA Appropriateness Method for the comparison and prioritisation of different options in healthcare.14 Ratings were grouped according to the level of agreement/disagreement with the statement: scores of 1–3 points were interpreted as rejection or disagreement, 4–6 points as lack of either agreement or disagreement, and 7–9 points as support or agreement.
Phases of the Delphi processIn accordance with the Delphi procedure,15 the questionnaire was distributed to members of the expert panel, who indicated their level of agreement with each statement. In the first round, panellists completed the questionnaire online, and were invited to add their opinions in free-form text. The technical team evaluated the evidence from the first round, presenting results as bar charts to facilitate comments and clarifications from each participant. Statements for which consensus was not reached were sent back to panellists for a second round of assessment. The results from the second round were tabulated and presented descriptively. The project concluded with a meeting of the scientific committee to debate and analyse the results.
Analysis and interpretation of the resultsThe consensus reached on each statement was analysed by calculating medians and interquartile ranges. Consensus was considered to have been reached for a statement if ≥66% of respondents assigned it a score within the same 3-point bracket (1–3 or 7–9 points) as the median. The type of consensus reached for each statement was defined according to the value of the median, with consensus in favour defined as a median score ≥7, and consensus against as a median ≤3. Consensus was considered not to have been reached if at least one-third of panellists assigned scores of 1–3, and another third assigned scores of 7–9. When the median score was in the range 4–6, opinion of the expert panel was considered to be unclear, with no consensus among a representative majority of the group.
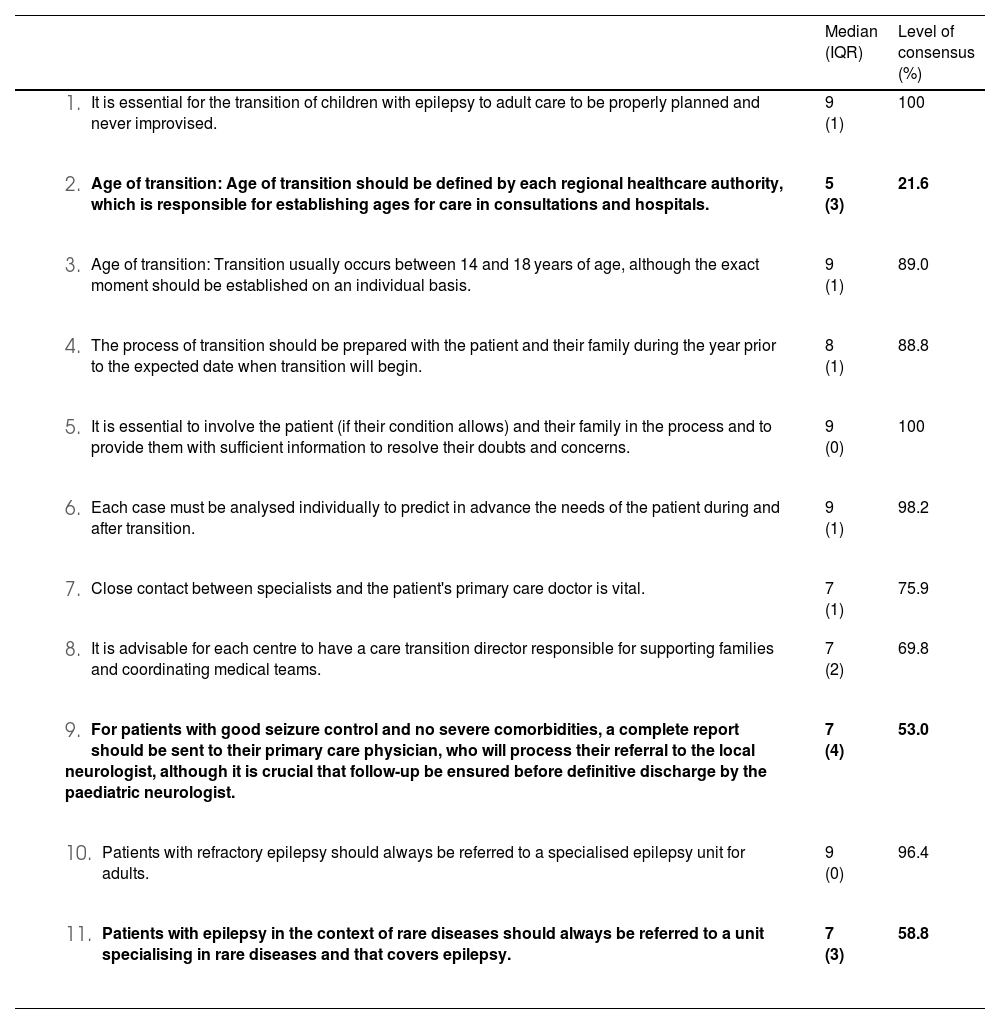
ResultsDelphi consensusOf the 54 experts consulted, 51 completed both rounds of the Delphi consensus process, with no new statements being proposed. In the first round of evaluation, consensus was reached for 33 of the 38 statements (86.8%), with consensus in favour in all cases. The remaining 5 statements were sent back to panellists for reconsideration in a second round, with consensus not being reached. Therefore, after 2 rounds, consensus was reached for 33 statements (86.8%). For the remaining 5 statements (13.2%), consensus was not established either in favour or against. Fig. 1 shows the results from each round; Tables 1–3 show the overall results for each of the statements analysed. Detailed results for each statement are presented in the Supplementary Material.
Section 1: Preparation of the patient at the paediatric neurology clinic and moments prior to transition to adult neurological care.
| Median (IQR) | Level of consensus (%) | |
|---|---|---|
| 9 (1) | 100 |
| 5 (3) | 21.6 |
| 9 (1) | 89.0 |
| 8 (1) | 88.8 |
| 9 (0) | 100 |
| 9 (1) | 98.2 |
| 7 (1) | 75.9 |
| 7 (2) | 69.8 |
| 7 (4) | 53.0 |
| 9 (0) | 96.4 |
| 7 (3) | 58.8 |
Statements for which consensus was not reached are shown in bold.
IQR: interquartile range.
Section 2: Process of transition from paediatric to adult neurology care.
| Median (IQR) | Level of consensus (%) | |
|---|---|---|
| 7 (2) | 72.2 |
| 8 (1) | 92.5 |
| 8 (1) | 96.3 |
| 9 (0) | 100 |
| 9 (1) | 96.4 |
| 7 (2) | 64.7 |
| 8 (2) | 75.9 |
| 8 (2) | 88.8 |
| 8 (2) | 81.5 |
| 7 (3) | 66.7 |
| 8 (2) | 87.0 |
Consensus was not reached for the statement shown in bold.
IQR: interquartile range.
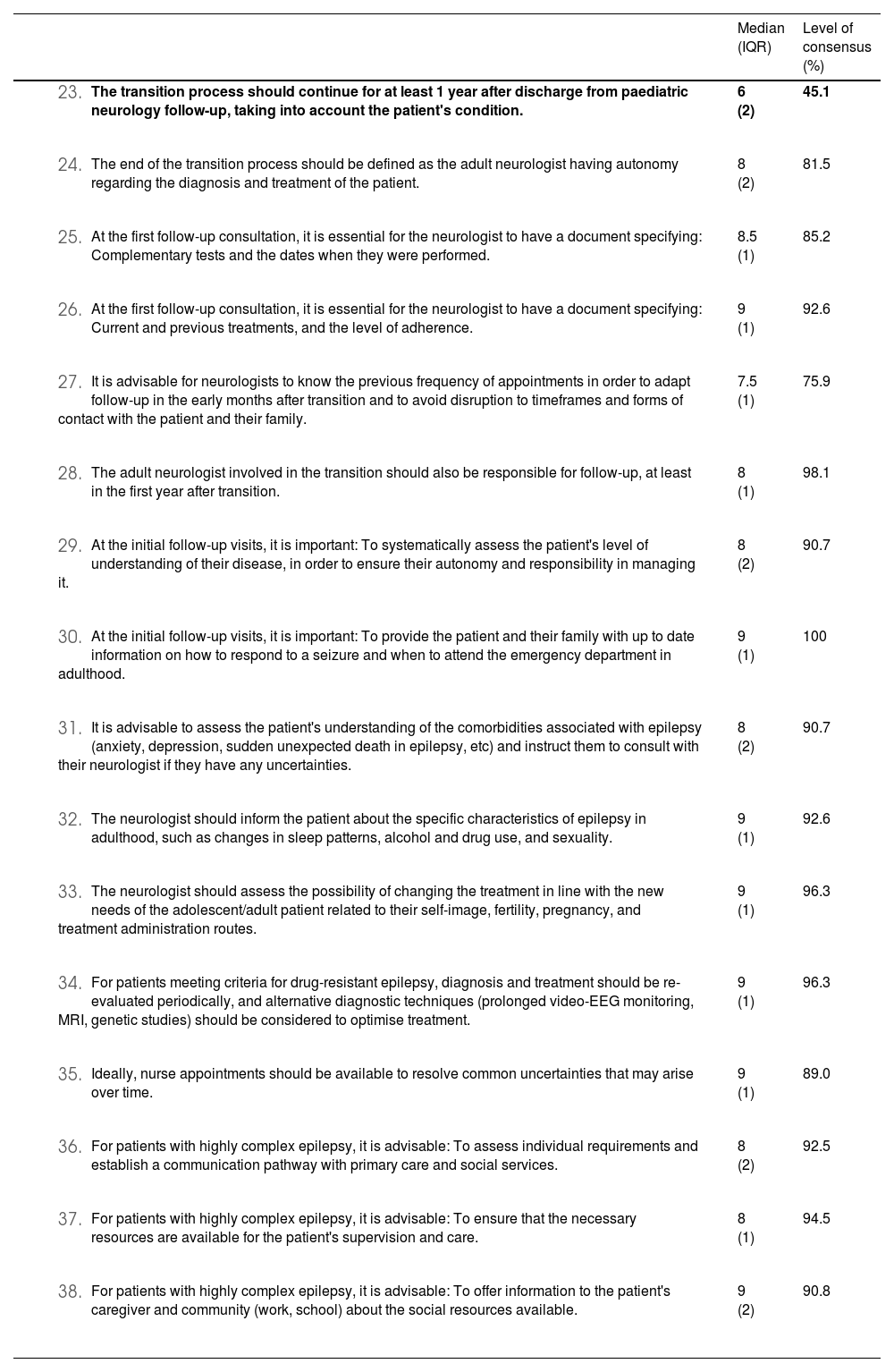
Section 3: Moments after transition and follow-up at the adult neurology clinic.
| Median (IQR) | Level of consensus (%) | |
|---|---|---|
| 6 (2) | 45.1 |
| 8 (2) | 81.5 |
| 8.5 (1) | 85.2 |
| 9 (1) | 92.6 |
| 7.5 (1) | 75.9 |
| 8 (1) | 98.1 |
| 8 (2) | 90.7 |
| 9 (1) | 100 |
| 8 (2) | 90.7 |
| 9 (1) | 92.6 |
| 9 (1) | 96.3 |
| 9 (1) | 96.3 |
| 9 (1) | 89.0 |
| 8 (2) | 92.5 |
| 8 (1) | 94.5 |
| 9 (2) | 90.8 |
Consensus was not reached for the statement shown in bold.
EEG: electroencephalography, IQR: interquartile range; MRI: magnetic resonance imaging.
Of the 11 statements considered regarding preparation of the patient at the paediatric neurology clinic and the moments prior to transition to adult neurology care, consensus was reached in favour of 8, after 2 rounds of evaluation. No consensus was reached for the 3 remaining statements (Table 1).
Consensus was unanimous for 2 statements: statement 1 (transitions should be properly planned and never improvised), and statement 5 (patients and their families must be involved in the process, providing adequate information to resolve their doubts and concerns).
No consensus was reached on the assertion that the age of transition should be defined by each regional healthcare authority, which is responsible for establishing ages for care in consultations and hospitals (statement 2). The expert panel also reached no consensus on the statement that for patients with good seizure control and no severe comorbidities, a complete report should be sent to their primary care physician, who would be responsible for processing their referral to the local neurologist, although it is crucial that follow-up be ensured before definitive discharge by the paediatric neurologist (statement 9). The third statement for which consensus was not reached was the assertion that patients with epilepsy in the context of a rare disease should be referred to a specialist rare diseases unit that covers epilepsy (statement 11).
Section 2: Process of transitionAfter 2 rounds of evaluation, consensus was reached in favour of 10 out of 11 statements on the process of transition from paediatric to adult neurological care, and was not reached for one statement (Table 2).
Unanimous consensus was reached for the statement that, prior to patient referral, the paediatric neurologist must ensure that the patient's clinical report is up to date and contains relevant information including syndromic diagnosis, progression time, criteria for drug resistance and comorbidities, and current and previous treatments (statement 15).
Consensus was not reached for the assertion that in the exchange of information during transition, it is advisable to create a committee, ideally for all patients and necessarily for patients with highly complex disease, whose opinions would be registered (statement 17).
Section 3: Moments after transition and follow-upConsensus was reached in favour of 15 out of 16 statements on the moments after transition from paediatric to adult neurological care and follow-up at the neurology consultation; consensus was not reached for one statement (Table 3).
Consensus was unanimous in favour of the statement that it is important at the first follow-up visits to provide the patient and their family with up to date information about how to respond to a seizure and when adult patients should attend the emergency department (statement 30).
Consensus was not reached regarding the statement that the transition process should continue for at least 1 year after discharge from paediatric neurology follow-up, taking into account the patient's condition (statement 23).
DiscussionOverall, the experts participating in the consensus panel generally shared similar opinions, as suggested by the high level of consensus reached for 86.8% of statements. However, some issues remained unresolved, underscoring the need to establish a standardised protocol.
The panellists agreed on the need for proper planning before the process of transition, with no room for improvisation; where possible, planning should begin a year before the beginning of the transition, and should involve the participation of the patient and their family. Epilepsy is a chronic disease, and patients' parents are in frequent contact with paediatric neurology departments; as a rule, they struggle with the change and will have doubts and concerns. Therefore, it is important that they be provided with sufficient information to address these concerns, and even, where possible, to introduce them to the neurologist who will manage their child after the transition to adult care. Patients and their parents must also adapt to a new form of follow-up, with changes in the duration and frequency of appointments; the focus of care shifts towards different objectives and disease characteristics in adulthood, with the patient (rather than their parents) taking the central role, where possible.
No consensus was reached regarding the statement that defining the age of the transition should be the task of regional healthcare authorities. While the Spanish ministry of health establishes an age of 18 years for the transition to adult care,4 in many autonomous communities this occurs at 14 years of age in practice. Therefore, the panellists suggested that it may be appropriate to establish an interval of 14–18 years, with each case treated on an individual basis according to patient and disease characteristics, and in accordance with the scientific knowledge and available human and material resources in each healthcare district. Overall, the participants believed that in more complex cases, transition should start earlier and be more progressive, with paediatric and adult neurology follow-up overlapping in order to take joint decisions. However, no consensus was reached regarding care transitions in patients with good seizure control and no comorbidities. Some panellists favoured referring them initially to primary care, for subsequent referral to a neurologist. Others preferred direct referral from paediatric to adult neurological care. Another issue on which consensus was not reached was the management of this transition in the context of rare diseases. This was due to the fact that not all healthcare districts have specialised rare diseases units.
In general, there was strong consensus in favour of statements regarding the transition process itself. Before referring the patient, paediatric neurologists should ensure that the clinical file is up to date and contains all relevant information, especially regarding aetiology, and that patients and their families receive all necessary information. Panellists believed that this should not take place during the final paediatric neurology consultation, but rather should be a progressive process, allowing sufficient time for important decisions to be made jointly and on an individual basis. Panellists agreed that a joint consultation should be held between the paediatric and the adult neurologist with the patient and their family for the exchange of information during the transition, and that there must be fluid communication between both physicians until the process is concluded; however, consensus was not reached on the idea of forming a committee. Some panellists supported the idea, suggesting the committee could include other specialists, such as psychologists, social workers, and nurses. Others argued that there was no need for such a committee, except in the most complex cases, as it would add further bureaucratic barriers to the process.
Finally, after the process of transition, neurologists should be aware of the previous frequency of consultations in order to adapt their follow-up, especially in the first months. During the first follow-up consultations, neurologists should have access to documents specifying the complementary tests performed, patients' current and previous treatments (and level of adherence), and should evaluate the patient's level of understanding about their disease, including comorbidities, providing additional education if needed in order to improve the patient's autonomy in managing the disease. In more complex cases, the individual needs of each patient should be assessed, and diagnosis and treatment may even be reconsidered with a view to optimising management. The only point on which no consensus was reached was the duration of the transition process. While some panellists supported a 1-year duration, others considered 3–6 months to be sufficient, mainly in order to avoid overburdening the healthcare system. In any case, the majority agreed that the duration of the process should be tailored to each case.
The limitations of this study are similar to those of other studies following similar designs, as both in Spain and in other countries in the surrounding region, this care transition process is yet to be perfectly established. However, this issue is currently being addressed by important study groups. Difficulties with this transition are common in all settings as a result of the great variability for defining the precise moment of transition; therefore, we must seek to achieve the greatest possible uniformity in developing a protocol for these care transitions. Currently, awareness and concern about this process are growing, as demonstrated by the considerable numbers of articles and consensus statements published in recent years. As no universally accepted clinical practice guidelines are currently available, the most relevant studies are based on expert opinions.
This study is our contribution regarding the paediatric transition process in Spain, and seeks to respect the diversity and clinical variability of the Spanish healthcare system. The recommendations present a high level of expert consensus from specialists in paediatric and adult epilepsy care, from different geographical regions and levels of care. Nonetheless, the responses of our panellists are always subjective, and caution should be exercised in their extrapolation to clinical practice. To minimise the potential influence on the consensus, the promoter took no part in the development of the study.
ConclusionsThis Delphi consensus statement is of particular relevance and represents the opinions of paediatric and adult neurology specialists on the transition from paediatric to adult epilepsy care. Although most panellists agreed on the measures and procedures to be implemented before, during, and after this transition, such as communication with patients and their families, preparation in advance, completeness of clinical reports, and review by the adult neurologist, certain other issues require clarification or are yet to be established. These include the involvement of healthcare authorities in establishing the age of transition, the details of transition in patients with good seizure control and no comorbidities, the involvement of committees in the transition process, and the duration of the transition process. Finally, it is essential for adult neurologists to have access to all information on the patient and their family, shared between professionals through reports or direct communication, and to reassess the patient's diagnosis and treatments.
FundingEISAI Farmacéutica SA funded this project, without participating in any way in study design, data analysis, or drafting of the article. EISAI Farmacéutica SA also funded the assistance with manuscript drafting.
Informed consentThis study did not involve human participants or patients.
Ethical considerationsThis study did not involve human participants or patients.
The authors thank Fernando Sánchez Barbero, PhD, of Springer Healthcare Ibérica SL, for his assistance with drafting the manuscript, and the company LET'S PLAY SL for managing the technical side of the project, including statistical analysis.
We would also like to thank all the panellists who participated in the consensus process: Sergio Aguilera López, Patricia Aguilera López, Helena Alarcón-Martínez, Olga Alonso Luengo, Raúl Amela, Javier Aparicio Calvo, Beatriz Bernardino Cuesta, Bárbara Blanco Martínez, Susana Boronat Guerrero, Pablo Cabezudo García, Rafael Camino León, Verónica Cantarín-Extremera, Amaya Castela Murillo, Cristina Coll, David Conejo Moreno, José Luis Cuevas Cervera, María de Toledo Heras, Verónica Delgadillo, Jana Domínguez Carral, Anna Duat, María Inés Escalza Cortina, José Carlos Estévez María, Joaquín Alejandro Fernández-Ramos, Elena Fonseca Hernández, Dionisio García Álvarez, Juan José García Peñas, Adrián García Ron, María Gómez Eguílaz, María del Carmen Gómez Lado, Verónica González Álvarez, José David Herrera García, Lucas Darío Iacampo Leiva, María Jiménez Legido, Myriam Ley, Francisco Javier López González, Jesús Luis Macarrón Vicente, Marcos Madruga Garrido, Ignacio Málaga Diéguez, Elena Maqueda, Ainhoa Marinas Alejo, Beatriz Martínez Menéndez, Inmaculada Medina Martínez, AlbertMolins Albanell, Laura Pulido Fontes, María Rosa Querol Pascual, Pablo Quiroga Subirana, Julio Ramos Lizana, Xiana Rodríguez Osorio, Juan Rodríguez Uranga, Eliana Rueda, Javier Salas Puig, Pedro Serrano Castro, Víctor Soto Insuga, and Eulàlia Turon Viñas.