A 55-year-old male without medical co-morbidities was referred to our hospital after presenting to an acute care clinic with confusion. No medical history could be obtained from the patient initially. Collateral history from his wife revealed the patient had a history of alcohol use disorder, and regularly drank at least four cans of beer a night for decades. He had abruptly ceased drinking three days prior to presentation. His wife described him as more irritable, and verbally aggressive, and that he was disoriented on the day of presentation. There was no mention of psychotic symptoms, abnormal speech, or observed seizure activity. He did not take any medications regularly, and was a distant ex-smoker. His wife denied any knowledge of previous hypertension diagnosis, or illicit drug use.
Examination at the time of his admission revealed tachycardia (108 bpm) and hypertension (185/103 mmHg). The patient was cachectic, and although alert, he was disoriented to time and place. His neurological examination was only remarkable for an ataxic gait.
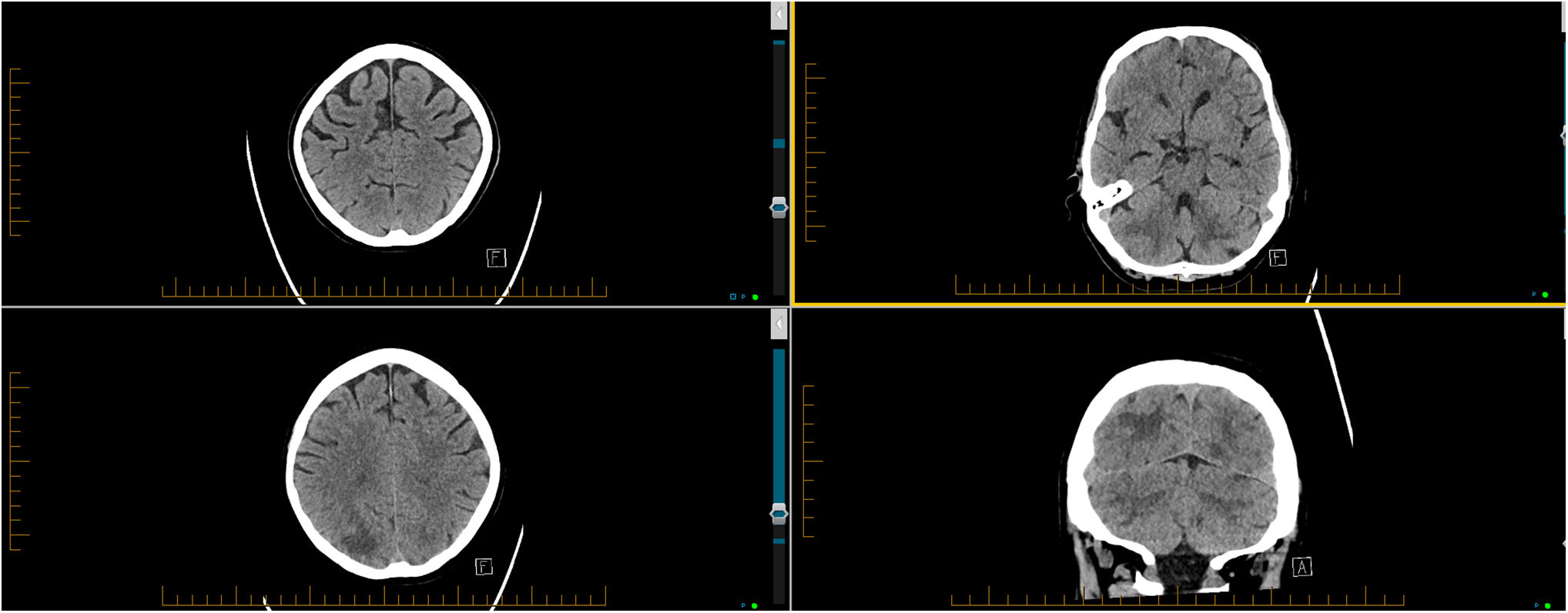
An electro-cardiogram on admission showed a sinus rhythm without voltage evidence of left ventricular hypertrophy. Basic blood tests revealed normal full blood count, renal function, thyroid function tests, and B12/folate. His liver functions tests were only notable for a raised GGT (205 U/L; reference range 10–50), and his fasting ammonia level was only mildly raised (46 μmol/L; reference range 11–32). Blood alcohol levels and urinary toxicology screen were not undertaken. At the time of his admission, he had a normal non-contrast CT brain (see Fig. 1A). The patient was commenced on thiamine and vitamin B-complex replacement, as well as Diazepam (in accordance with our Alcohol Withdrawal Scale protocol).
On the following morning, the patient had some improvement in his mental state, and was able to interact with the medical team during their rounds. He confirmed that his last drink was three days prior to presentation. The medical team noted bilateral dysmetria of the upper limbs, a rest tremor of the right hand, and an ataxic, broad-based gait. On day 2 of his admission, the patient had three generalised tonic–clonic seizures (GTCS) in the space of two hours. The second and third seizures necessitated intravenous Midazolam to terminate. He was commenced on twice-daily intravenous Levetiracetam 500 mg, and the team requested a repeat non-contrast CT brain; this showed new bilateral occipito-parietal and equivocal cerebellar abnormalities (see Fig. 1B–D), raising suspicion for posterior reversible encephalopathy syndrome (PRES). As he remained hypertensive (BP range 140–205/80–108 mmHg), he was commenced on several anti-hypertensives.
The neurology team was then consulted. At this time, the patient was disoriented, and could not follow one-step commands. He had new cerebellar dysarthria, and a lack of spontaneous movement on the left upper and lower limbs was noted. It was difficult to ascertain if he was cortically blind. The neurology team felt that PRES would explain most of his presentation. Differential diagnoses considered included: Non-convulsive seizures, posterior circulation stroke, and infectious meningo-encephalitis.
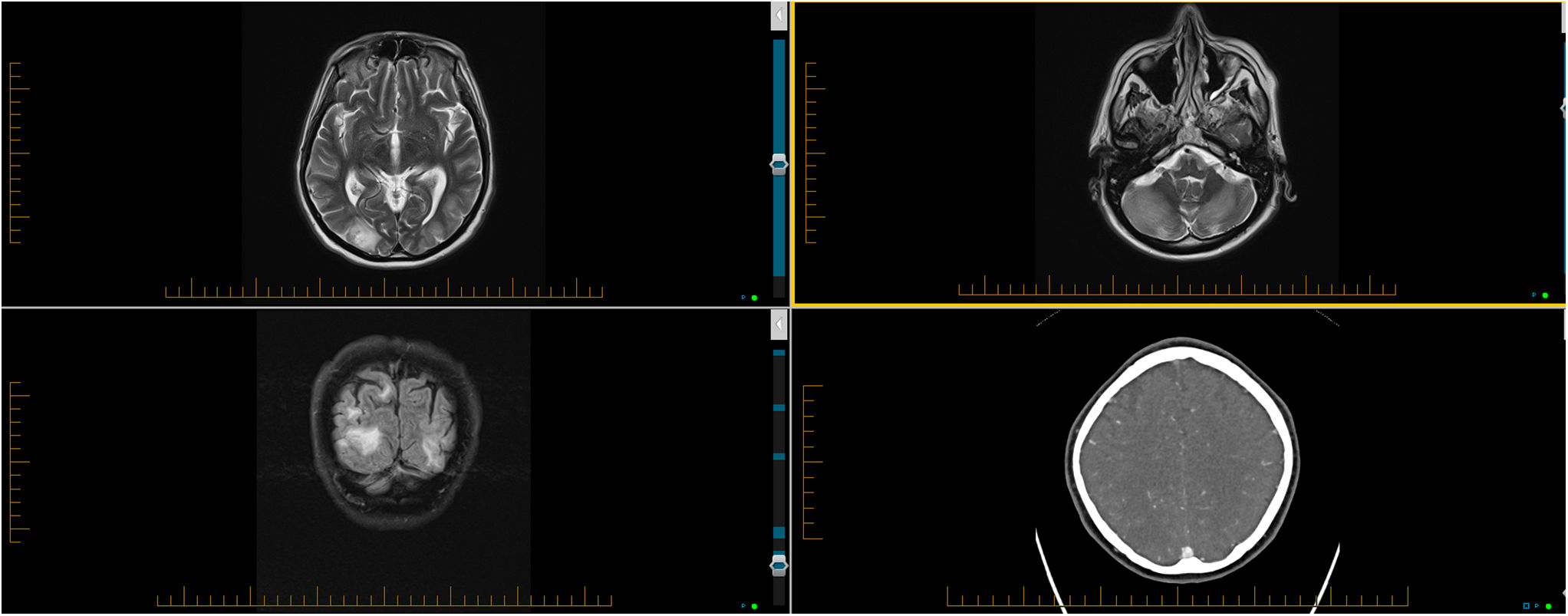
A non-contrast MRI brain revealed posterior white matter abnormalities with some haemorrhagic change in the right occipital lobe. In the clinical setting, the changes were felt consistent with diagnóstico of PRES (see Fig. 2A–C). He has a negative HIV serology test. His cerebrospinal fluid (CSF) was bland, without significant pleocytosis, but had a raised protein (0.72 g/L; no detectable oligo-clonal bands). He also had a repeat CT angiography of the brain which did not show any changes to suggest intra-cranial vasculitis (see Fig. 2D).
(clockwise from the left upper image): MRI revealed predominant posterior white matter abnormalities within the occipital lobes and cerebellum, and some haemorrhagic change right occipital lobe (A–C). A repeat CT angiography three days after the MRI showed no features of vasculitis (D).
Over the ensuing days, his blood pressure had improved (BP range 103–154/51–87 mmHg). However, on day 5, the patient developed a fever, with a subsequent chest X-ray confirming a left-sided pneumonia, and an associated pleural effusion. He was commenced on intra-venous antibiotics, and supplementary oxygen. Despite these measures, the patient's responsiveness, gas exchange, and haemodynamic parameters continued to deteriorate. Due to the lack of clinical improvement, a decision was made to change treatment to a palliative approach, and he passed away on day 9.
The posterior reversible encephalopathy syndrome is a clinico-radiological diagnosis, based on a constellation of signs, and characteristic brain imaging features.1 Classically associated with hypertension and immune-suppressive medications, PRES has also been described in relation to several other medical conditions. Although the pathophysiology of PRES remains somewhat controversial, prominent theories suggest that vascular endothelial disruption is central to the pathophysiology of the disease.1
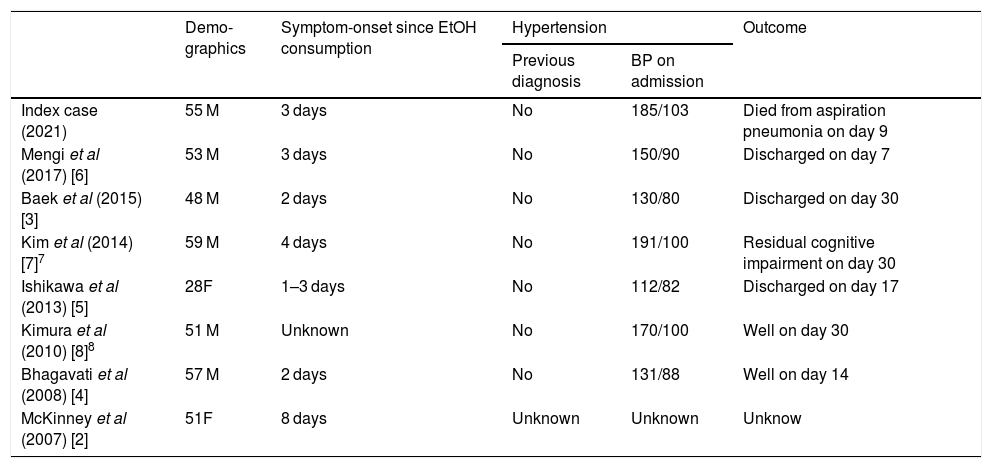
Only a handful of alcohol withdrawal-related PRES have been described in the literature (Table 1). Most of the cases are of men in their middle age (range, 28–59). Although the symptoms of alcohol withdraw may manifest as early as 6–24 h following last consumption, the withdrawal period varies, but may extend to as long as 10 days.
Clinical details of reported cases of alcohol withdrawal-associated PRES. BP = blood pressure; EtOH = ethanol; F = female; M = male.
| Demo-graphics | Symptom-onset since EtOH consumption | Hypertension | Outcome | ||
|---|---|---|---|---|---|
| Previous diagnosis | BP on admission | ||||
| Index case (2021) | 55 M | 3 days | No | 185/103 | Died from aspiration pneumonia on day 9 |
| Mengi et al (2017) [6] | 53 M | 3 days | No | 150/90 | Discharged on day 7 |
| Baek et al (2015) [3] | 48 M | 2 days | No | 130/80 | Discharged on day 30 |
| Kim et al (2014) [7]7 | 59 M | 4 days | No | 191/100 | Residual cognitive impairment on day 30 |
| Ishikawa et al (2013) [5] | 28F | 1–3 days | No | 112/82 | Discharged on day 17 |
| Kimura et al (2010) [8]8 | 51 M | Unknown | No | 170/100 | Well on day 30 |
| Bhagavati et al (2008) [4] | 57 M | 2 days | No | 131/88 | Well on day 14 |
| McKinney et al (2007) [2] | 51F | 8 days | Unknown | Unknown | Unknow |
How alcohol withdrawal could cause PRES remains unclear. Autonomic dysregulation of cerebral blood flow, with incipient endothelial dysfunction have been proposed to play major roles in the pathogenesis on PRES.2 Withdrawal of alcohol, a depressant substance, is associated with autonomic over-activity. This is commonly observed in the form of tachycardia and hypertension—features that were present in our patient on admission. The blood pressures of at least three of the patients presented in Table 1 were in the normal range.3–5 However, in two of those cases,3,5 patients had concomitant acute pancreatitis (often associated with hypotension).
The history obtained from our patient, and later his wife, made such precipitants as acute alcohol intoxication, and illicit drugs (including cocaine and cannabis) less likely, although no laboratory confirmation was sought. We postulate that alcohol withdrawal (or, less likely, toxicity) led to a sympathetic surge (including hypertension). This, in turn, disrupted cerebral vascular auto-regulation/endothelial function, which eventually culminated in PRES.
Treatment of PRES is generally supportive.1 In hypertensive patients, blood pressure-lowering medications should be promptly instituted. Where possible, other inciting factors (e.g., calcineurin inhibitors) should be discontinued.1 In patients with alcohol withdrawal, management is best done pro-actively (i.e., prior to the development of complications). Several instruments exist (e.g., CIWA-Ar score) 6 to aid clinicians in the early identification (and treatment) of such complications.
As the name suggests, reversibility of clinical and neuro-radiological deficits in PRES is the expectation for most patients.1 However, permanent neurological sequalae and death have been reported in several patients, generally because of intra-cerebral haemorrhage, cerebral oedema, or complications related to the underlying aetiology.
DeclarationsEthics approvalNot required.
Consent for publicationWritten informed consent was obtained from the patient's wife for publication of this case report and any accompanying images.
Availability of data and materialNot applicable.
Competing interestsNone to declare.
FundingNone received.
Authors' contributionsSole author.
None.