Cardioembolism may cause 20%–40% of all ischemic strokes. Up to 22% of cardioembolic strokes are associated with intracardiac thrombi and occur in patients with a high burden of comorbid cardiac disease.
Aim and methodsTo describe the in-hospital experience of stroke patients with intracardiac thrombi. A retrospective 1 center study was carried out. Demographic, clinical, stroke, echocardiographic, and outcome data of stroke patients with intracardiac thrombi were extracted.
ResultsFrom 2018 to 2019, 530 stroke patients were admitted. Nine (1.7%) had intracardiac thrombi, 100% males with mean age 63.3 years. There were a high prevalence of cardiovascular risk factors, with anterior circulation stroke in 8 (88%) and large vessel occlusion in 8 (88%). Most had major echocardiographic findings and 8 (88%) had a discharge outcome Rankin scale score > 3.
ConclusionIntracardiac thrombus is not an uncommon cause of stroke. Cardiac ultrasound is a sensitive diagnostic method and should be sought in older patients with high prevalence of cardiovascular risk factors and history of cardiac disease.
Los cardioembolismos son la causa de entre el 20% y el 40% de los ictus isquémicos. Hasta un 22% de los ictus cardioembólicos están relacionados con trombos intracardíacos y afectan a pacientes con una elevada carga de comorbilidad cardíaca.
Objetivo y métodos: Describir la experiencia intrahospitalaria en pacientes con ictus y trombosis intracardíaca. Para ello, realizamos un estudio unicéntrico retrospectivo en el que recogimos datos demográficos, clínicos y ecocardiográficos y los resultados de pacientes con ictus y trombosis intracardíaca.
ResultadosEntre los años 2018 y 2019, ingresaron 530 pacientes con ictus en nuestro centro. Nueve (1,7%) presentaban trombos intracardíacos, siendo todos ellos hombres con una edad media de 63,3 años. Observamos una elevada prevalencia de factores de riesgo cardiovascular, en concreto infarto de circulación posterior en 8 (88%) y oclusión de gran vaso en otros 8 (88%). La mayoría presentó hallazgos ecocardiográficos relevantes y 8 de ellos obtuvieron una puntuación superior a 3 en la escala de Rankin al alta.
ConclusiónLa trombosis intracardíaca no es una causa infrecuente de ictus. La ecografía cardíaca es un método diagnóstico sensible que debe realizarse en pacientes de mayor edad con una elevada prevalencia de factores de riesgo cardiovascular y antecedentes de patología cardíaca.
Cardioembolism accounts for approximately 20%–40% of all ischemic strokes each year. Cardioembolic stroke has a high recurrence rate and poor outcome, but are largely preventable.1–3 Major-risk cardioembolic sources include auricular fibrillation, valvular disease, severe left ventricular dysfunction, endocarditis, cardiac tumors, paradoxical embolism, and intracardiac thrombi (ICT).4,5
Previous studies using transesophageal echocardiography have reported an incidence of 3%–22% of ICT in stroke patients.6,7 Up to 70% of ICT in stroke patients are found in the left auricular appendage and the majority associated with auricular fibrillation.8,9 But left intraventricular thrombi are not uncommon and higher rates of ICT may be detected in patients older than 75 years of age and with cardiac computed tomography (CT) or magnetic resonance imaging (MRI).10–12
ICT are related to higher rates of stroke recurrence, large vessel occlusions, hemorrhagic transformation, multiple territory strokes, symptomatic coronary artery disease, ECG evidence of ischemia, auricular fibrillation, left ventricular dysfunction, and worse clinical prognosis.13,14
The aim of the study is to present a high volume cardiovascular center experience of acute stroke patients with ICT.
Materials and methodsAcute stroke patient's in-hospital records admitted at La Cardio from August 2018 to August 2019 were reviewed. Demographic, clinical, echocardiographic, and outcome data of stroke patients with ICT were extracted. Continuous variables are described in medians and qualitative variables in frequencies. The study was approved by the ethics committee and conducted according to the national and international regulations in clinical investigation. Our university hospital is a 350-bed cardiovascular reference center located in the Colombian capital city, Bogota.15
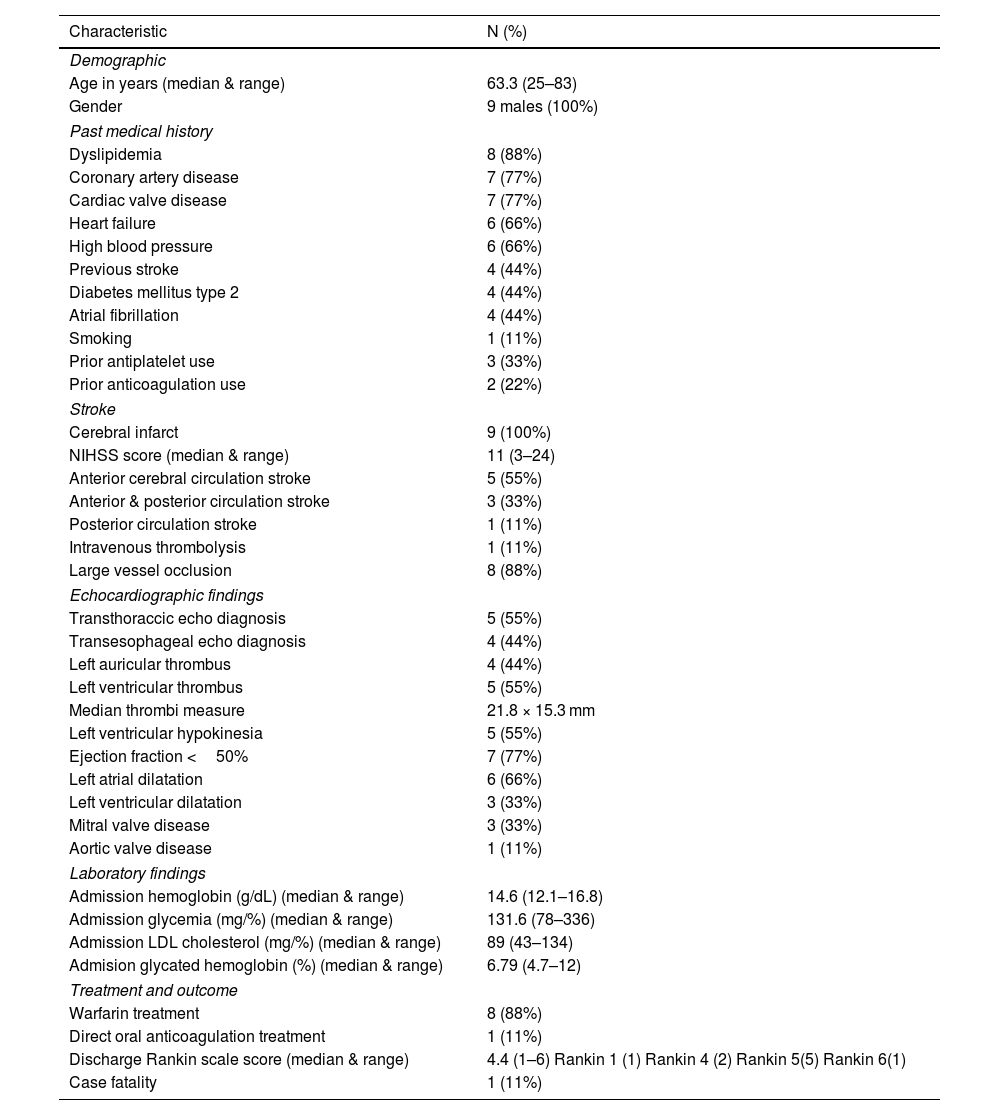
ResultsOut of 530 ischemic stroke patients admitted in the study period, 9 (1.7%) were diagnosed with ICT, mean age 63.3 and 100% males. All ICT were diagnosed with ultrasound and patient's characteristics are shown in Table 1. Four (45%) thrombus were located in the left auricle and 5 (55%) in the left ventricle, with a mean size of 21.8 × 15.3 mm. There was a high incidence of vascular risk factors, anterior cerebral circulation involvement (88%), large vessel strokes (88%), and major echocardiographic findings. All strokes were cerebral infarcts, all received anticoagulation and only 1 (11%) was treated with reperfusion therapy. Median hospital discharge modified Rankin scale score was 4.4 with 1 (11%) in-hospital case fatality.
Main clinical characteristic's of stroke patients with intracardiac thrombi. August 2018–August 2019, La Cardio, Bogota, Colombia.
| Characteristic | N (%) |
|---|---|
| Demographic | |
| Age in years (median & range) | 63.3 (25–83) |
| Gender | 9 males (100%) |
| Past medical history | |
| Dyslipidemia | 8 (88%) |
| Coronary artery disease | 7 (77%) |
| Cardiac valve disease | 7 (77%) |
| Heart failure | 6 (66%) |
| High blood pressure | 6 (66%) |
| Previous stroke | 4 (44%) |
| Diabetes mellitus type 2 | 4 (44%) |
| Atrial fibrillation | 4 (44%) |
| Smoking | 1 (11%) |
| Prior antiplatelet use | 3 (33%) |
| Prior anticoagulation use | 2 (22%) |
| Stroke | |
| Cerebral infarct | 9 (100%) |
| NIHSS score (median & range) | 11 (3–24) |
| Anterior cerebral circulation stroke | 5 (55%) |
| Anterior & posterior circulation stroke | 3 (33%) |
| Posterior circulation stroke | 1 (11%) |
| Intravenous thrombolysis | 1 (11%) |
| Large vessel occlusion | 8 (88%) |
| Echocardiographic findings | |
| Transthoraccic echo diagnosis | 5 (55%) |
| Transesophageal echo diagnosis | 4 (44%) |
| Left auricular thrombus | 4 (44%) |
| Left ventricular thrombus | 5 (55%) |
| Median thrombi measure | 21.8 × 15.3 mm |
| Left ventricular hypokinesia | 5 (55%) |
| Ejection fraction <50% | 7 (77%) |
| Left atrial dilatation | 6 (66%) |
| Left ventricular dilatation | 3 (33%) |
| Mitral valve disease | 3 (33%) |
| Aortic valve disease | 1 (11%) |
| Laboratory findings | |
| Admission hemoglobin (g/dL) (median & range) | 14.6 (12.1–16.8) |
| Admission glycemia (mg/%) (median & range) | 131.6 (78–336) |
| Admission LDL cholesterol (mg/%) (median & range) | 89 (43–134) |
| Admision glycated hemoglobin (%) (median & range) | 6.79 (4.7–12) |
| Treatment and outcome | |
| Warfarin treatment | 8 (88%) |
| Direct oral anticoagulation treatment | 1 (11%) |
| Discharge Rankin scale score (median & range) | 4.4 (1–6) Rankin 1 (1) Rankin 4 (2) Rankin 5(5) Rankin 6(1) |
| Case fatality | 1 (11%) |
NIHSS: National Institute of Health Stroke Scale. LDL: Low Density Lipoprotein.
In our study, acute stroke patients had a lower incidence (1.7%) of ICT than previously reported (3%–22%), left ventricular thrombi accounted for 55%5 of the cases and all were men. Nonetheless, other clinical characteristics were similar to the reported in the literature. Acute stroke patients with ICT had a mean age of 63.3 years with high prevalence of cardiovascular risk factors and high burden of cardiac comorbidities. Most strokes involved the anterior circulation of the brain (88%), with large vessel occlusions (88%, mean NIHSS score 11) and greater degree of disability (Hospital discharge modified Rankin scale score > 3 in 88%).
In accordance to recently published guidelines, all stroke patients with ICT, received anticoagulation for secondary prevention.16 Only 1 (11%) patient received reperfusion therapy with intravenous thrombolysis without any serious adverse events.
Although, more than 50% of cardioembolisms are associated with auricular fibrillation, ICT is an important source.16,17 The left auricular appendage is the most common location for ICT, especially in the setting of auricular fibrillation.18 However, left ventricular thrombus is not uncommon in patients with coronary artery disease, heart failure, and ventricular wall dysfunction.19 Major-risk cardioembolic sources are comorbid and some predispose to the formation of ICT.20 The embolus composition varies according to the cardiac pathology and they may reach almost any organ, but more than 80% of symptomatic emboli are in the brain.21,22 Cardioembolic stroke involve the anterior cerebral circulation in approximately 80% and the vertebrobasilar territory in 20%.23 Reperfusion therapies in acute stroke patients with ICT are not contraindicated, but there may be a higher risk of hemorrhagic transformation and thrombus fragmentation with multiple systemic emboli.24,25 Anticoagulation is the secondary prevention therapy of choice, with most clinicians preferring heparinoids and vitamin K antagonist over direct oral anticoagulants.26,27
Clinicians treating acute stroke patients should be vigilant for ICT in older individuals with high prevalence of vascular risk factors and cardiovascular disease, including but not limited to coronary artery disease, heart failure, heart valve disease, auricular fibrillation, and previous recent stroke.28,29 Initial diagnosis should be with transthoracic or transesophageal cardiac ultrasound but a lower threshold for cardiac CT or MRI should be contemplated.30–32
Limitations of the study include a 1 center retrospective experience, small number of included patients, in-hospital follow up, and ICT diagnosis using only ultrasound imaging. But, medical records were thoroughly reviewed, the institution is high volume stroke and cardiovascular reference center with an experienced echocardiography service and, to the best of our knowledge, it is the first Colombian case series of acute stroke patients with ICT.
ConclusionsIntracardiac thrombi (CT) it is not an infrequent cause of stroke. Patients with an acute stroke and ICT tend to be older with a high burden of vascular risk factors and cardiovascular disease. Stroke severity and outcome are usually dismal, initial work up may include cardiac ultrasound, cardiac computed tomography or magnetic resonance imaging. Reperfusion therapies are not contraindicated and anticoagulation is the treatment of choice for secondary prevention.
FundingNone.
Patient consent (informed consent)Ethical approval and consent form are signed in hospital admission.
Ethical considerationsAll authors have followed the protocols according to LaCardio, university hospital, as the institution for the work and publication of the data.