Neurophobia describes a fear of clinical neurology and neurosciences. When present in doctors, fear or uncertainty regarding clinical neurology may contribute to inadequate neurological assessments and inappropriate referrals.1,2 Medical students may arrive at their initial clinical neurology rotation, or even in their first year of medical school, with negative preconceptions concerning the difficulty and nature of the specialty.3 There is limited information on the basis for these preconceptions.
A better understanding about how these negative opinions arise may facilitate development of effective interventions that assuage fear of clinical neurology.4 This project aims to evaluate the preconceptions that medical students hold regarding clinical neurology, and what has contributed to their development.
A cross-sectional online anonymous voluntary survey was advertised to medical students at the start of clinical school in the University of Cambridge, United Kingdom. Participants included in the study were consenting ≥18-year-old, year 4 medical students at the participating institution. All students fulfilling these criteria were included, irrespective of previous non-clinical neuroscience, physiology, or psychology teaching. These inclusion criteria were employed to optimise the generalisability of the findings of the study. A raffle for gift vouchers was offered. This study received institutional Ethics Committee approval (PRE.2017.062). The anonymous survey was administered online (Qualtrics.com), and consisted of 30 questions (see Supplementary Information-1). Questions were administered as both Likert-type scales and as free-text. Statistical analysis was conducted using R (version 1.0.153). The relationship between statements about neurology that >50% of students agreed with and proposed factors influencing these preconceptions were analysed using parametric statistics (multiple regression).5
The pre-rotation survey was completed by 131 individuals of a cohort of 260 (response rate 50.4%). 66 (50.4%) were female and 130 were under the age of 26. 39 participants (29.0%) had first degree relatives/close family who were doctors. All students studied preclinical neuroscience as a compulsory component of the course, in year 2. In the student selected third year, 44 (33.6%) chose a degree such as neuroscience or physiology, and 24 (18.3%) studied psychology.
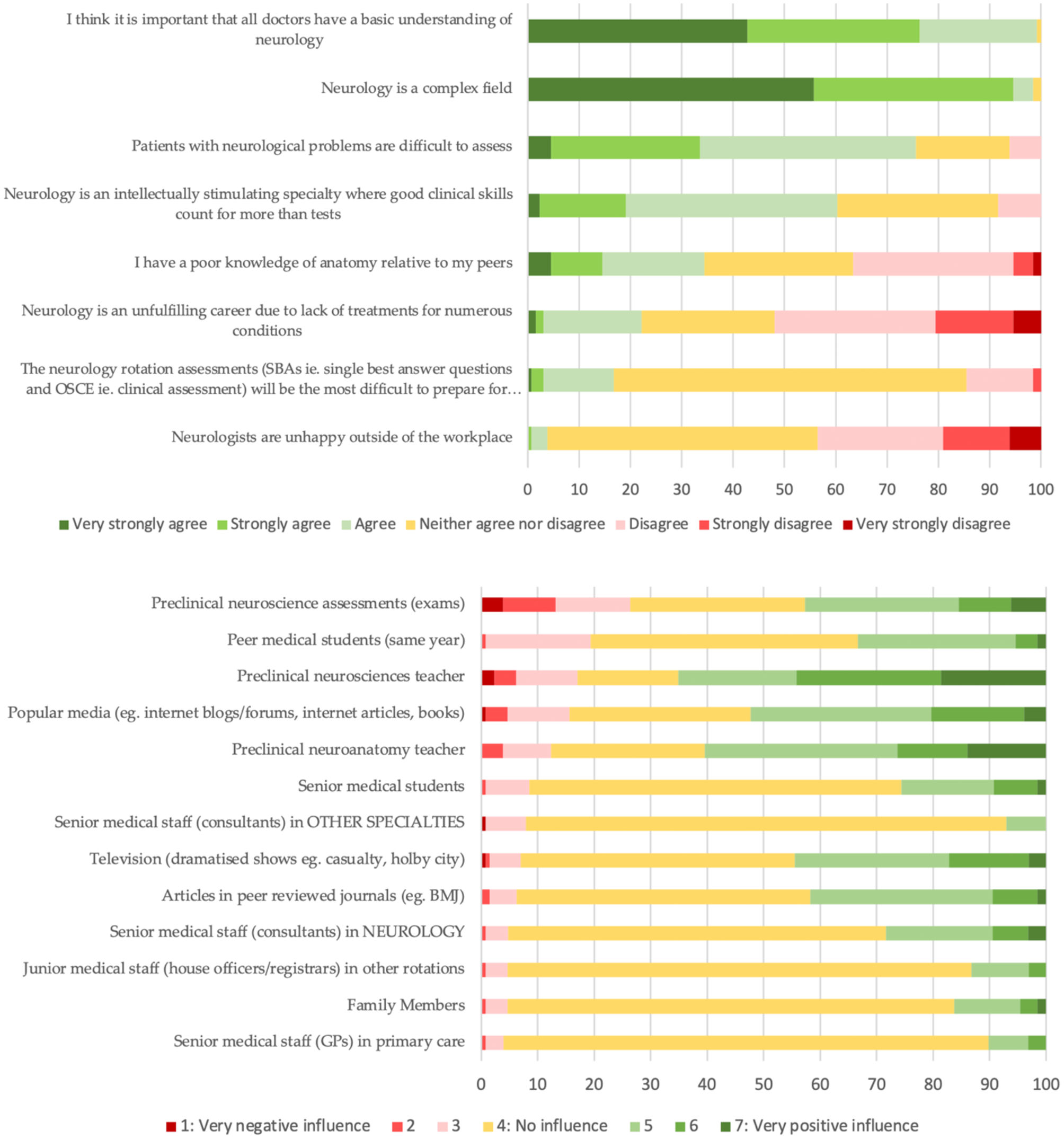
Student responses regarding their preconceptions about neurology supported the claim that there was concern as to the challenging nature of the subject (Fig. 1A). Particularly, 99 participants (75.6%) agreed with the statement that “patients with neurological problems are difficult to assess”. That being said, positive preconceptions were also described, with 60.6% of students agreeing with a statement that “Neurology is an intellectually stimulating specialty where good clinical skills count for more than tests”. Factors that affected opinions about neurology in more than half of the group included preclinical neurosciences (82.2%) and neuroanatomy (72.9%) teachers, preclinical exams (69%), popular media (68%), peer medical students (52.7%) and television shows (51.6%) (Fig. 1B). The only factor that generated a more negative than positive response was consultants in other specialties (7.9%), but few students picked this as a relevant factor overall (15%). The most frequently cited negative influence was preclinical neuroscience assessment (26.4%), followed by input from peer medical students (19.4%) and preclinical neuroscience supervisors (17.1%). In the participating institution, these supervisors teach medical students in groups of 3–4, alongside their lectures and practicals in pre-clinical neuroscience.
Conversely, the most commonly cited factor having a positive influence was preclinical neuroscience supervisors (65.1%), followed by preclinical neuroanatomy supervisors (60.5%) and popular media e.g., Internet blogs/forums, Internet articles, books (52.3%).
In free-text responses describing how students felt they had formed their opinions regarding neurology, some students demonstrated awareness of their lack of clinical exposure; e.g., “I don't feel like I've had enough exposure to neuroscience to have formed any opinions yet”. Students also provided further details regarding the “popular media” category, demonstrating use of a range of resources: “Mainly TV shows to be honest… make it seem like the coolest job in the world”.
Agreement with the statement ‘Neurology is a complex field’ was associated with the influence of senior medical students (p = 0.00314), close medical relatives (p = 0.00185) and studying a non-neuroscience related subject in the third year (non-medical degree p = 0.00626; non-neuroscience medical related degree p = 0.00977). No significant associations were found for the statement ‘Patients with neurological problems are difficult to assess’.
The influence of junior doctors was found to be positively associated with student opinions regarding the importance of having a basic understanding of neurology (p = 0.0153). Students who chose a degree including a neuroscience module in third year (p = 0.0183) or psychology (p = 0.0245) were more likely to agree with the statement regarding neurology being intellectually stimulating. Preclinical neuroscience teachers also affected this positive opinion (p = 0.0371).
It should be noted that the cross-sectional nature of the study means that causation cannot be determined. Longitudinal changes in student opinion could not be assessed. Non-response bias may also have influenced results.
Medical student preconceptions are frequently based upon preclinical academic experiences, particularly small group teaching, but television and popular media are also influential. Neurophobia remains a significant issue. However, many students also hold positive preconceptions regarding clinical neurology. Further study is warranted to assess whether student preconceptions are modifiable and how strongly they affect students' opinions following clinical neurology rotations.
Patient consentParticipants (medical students) provided consent to participate in the study.
Ethical considerationsThis study received Cambridge Psychology Research Ethics Committee approval (PRE.2017.062).
Jesus College provided funding for the raffle prizes.