The obstetric hemorrhage is the second cause of mortality in Mexico, and the first in the developing world. Delayed control of obstetric bleeding is the main cause of deaths associated to this complication, which can be attributed to lack of skilled healthcare personnel to implement effective procedures for proper control. According to data from the Mexico's National Health and Nutrition Survey of 2006, 93.3% of maternal death cases received medical care during delivery; 86% of such deaths occur in hospital facilities.1 An irreversible damage leading to patient's death is the result of ineffective hemorrhage control during patient transfer or until control-oriented measures to treat the origin of bleeding are implemented.
The clamping of uterine arteries transvaginally is a simple and effective technique for the control of obstetric hemorrhage. It provides a tourniquet-like effect to contain blood loss, allowing clinician's maneuver for bleeding control to take effect and/or patient transfer. This letter describes in detail the technique.
Clamping of uterine arteries transvaginallyInstruments required:
- •
Two curved Foerster forceps.
- •
Two straight Foerster forceps.
- •
Two Eastman vaginal retractors (or a vaginal speculum if vaginal retractors are not available).
- •
Foley catheter.
Once a uterine bleeding greater than 500mL has been detected, and it is unresponsive to the usual first choice management of uterine massage and oxytocin administration, proceed to the following operations:
- 1.
Place both the anterior retractor and the posterior retractor into the vagina to visualize the cervix.
- 2.
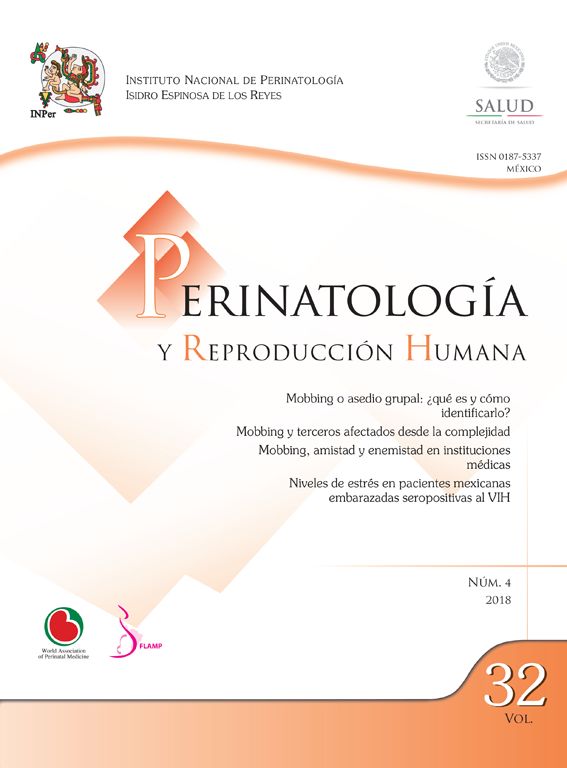
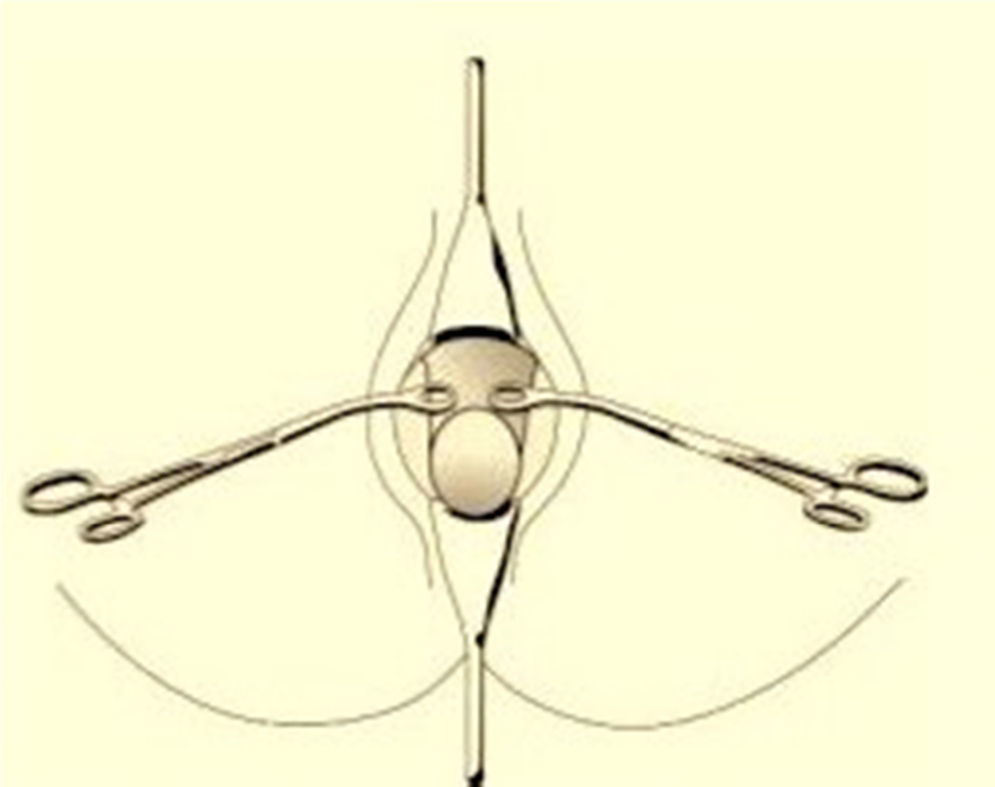
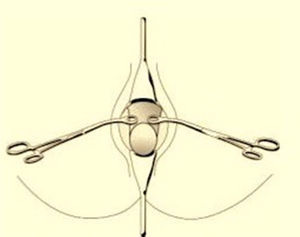
Use a straight Foerster forceps to clamp the anterior lip of the cervix, and the second straight Foerster forceps to clamp the posterior lip, at the middle point of them (Fig. 1).
- 3.
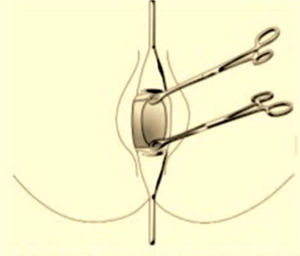
Move the anterior and posterior retractors to the left side of the vagina, sliding both straight forceps to the opposite side until cervical edge is readily observed.
- 4.
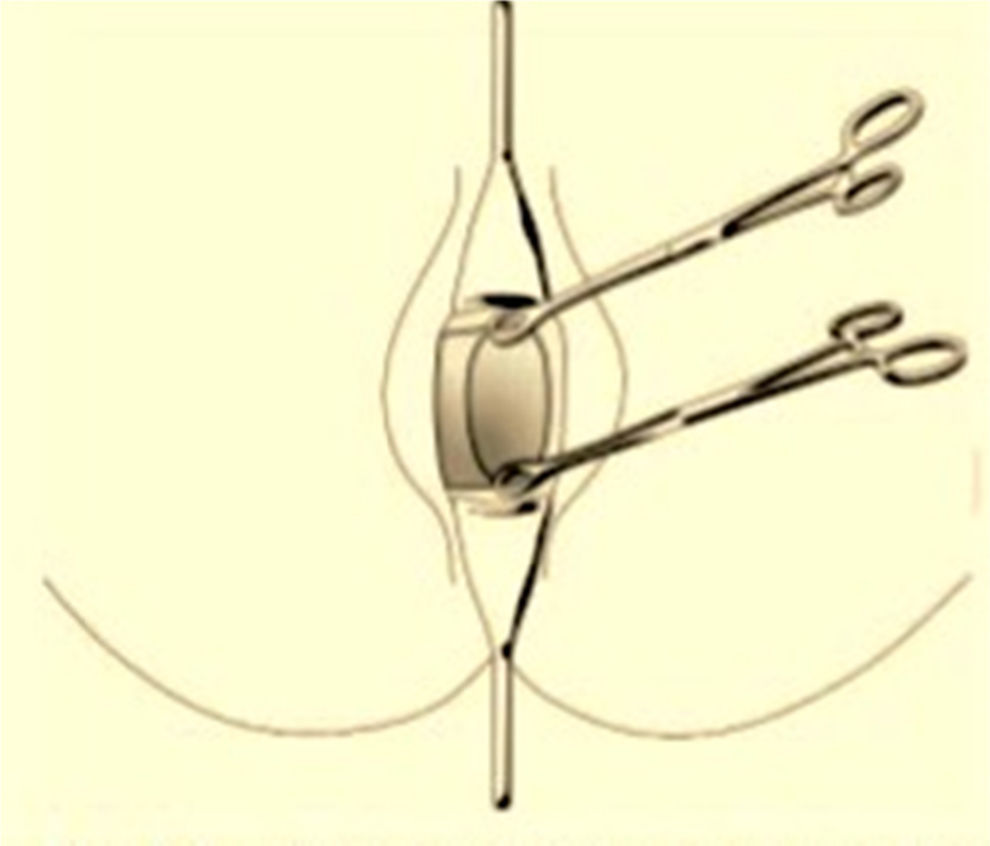
Then the left cardinal ligament is palpated.
- 5.
A curved Foerster forceps is placed medially, starting from the junction of cardinal ligament with the uterus horizontally toward the uterus center itself, in order to achieve clamping of the left uterine arteria (Fig. 2).
- 6.
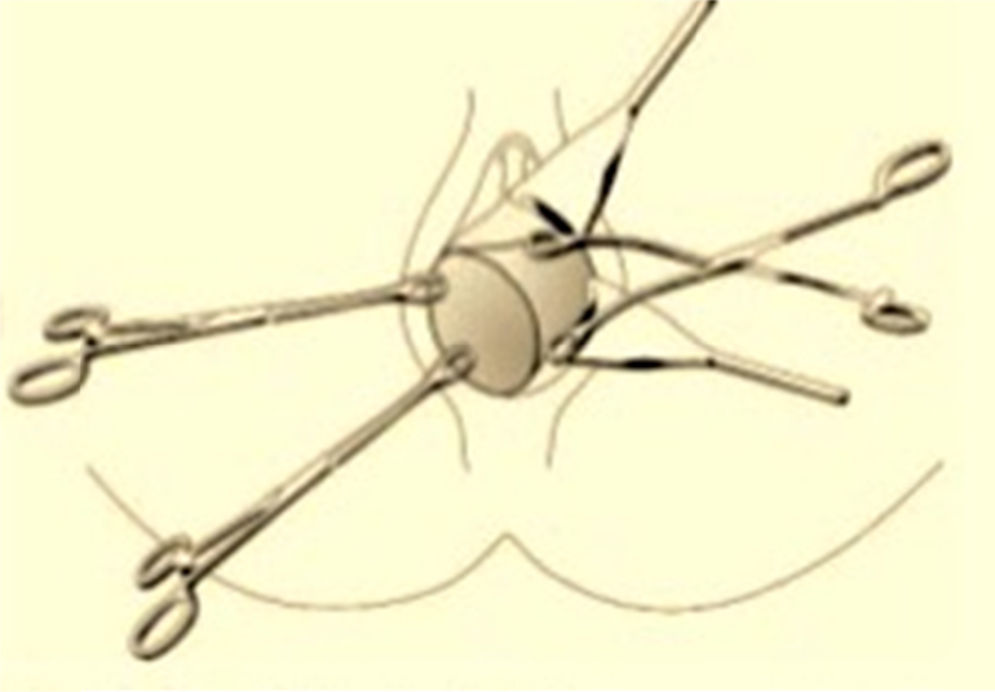
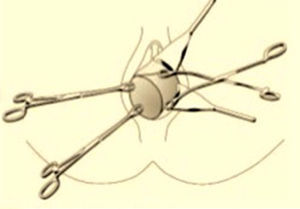
Immediately, vaginal retractors are move to the right side of the vagina along with the straight Foerster forceps to allow visualization of the cervical edge and the right cardinal ligament.
- 7.
Proceed to place the other curved Foerster forceps medially, horizontally toward the uterine center, in order to clamp the right uterine artery, leaving enough space to perform instrumented revision of the uterine cavity (Fig. 3).
- 8.
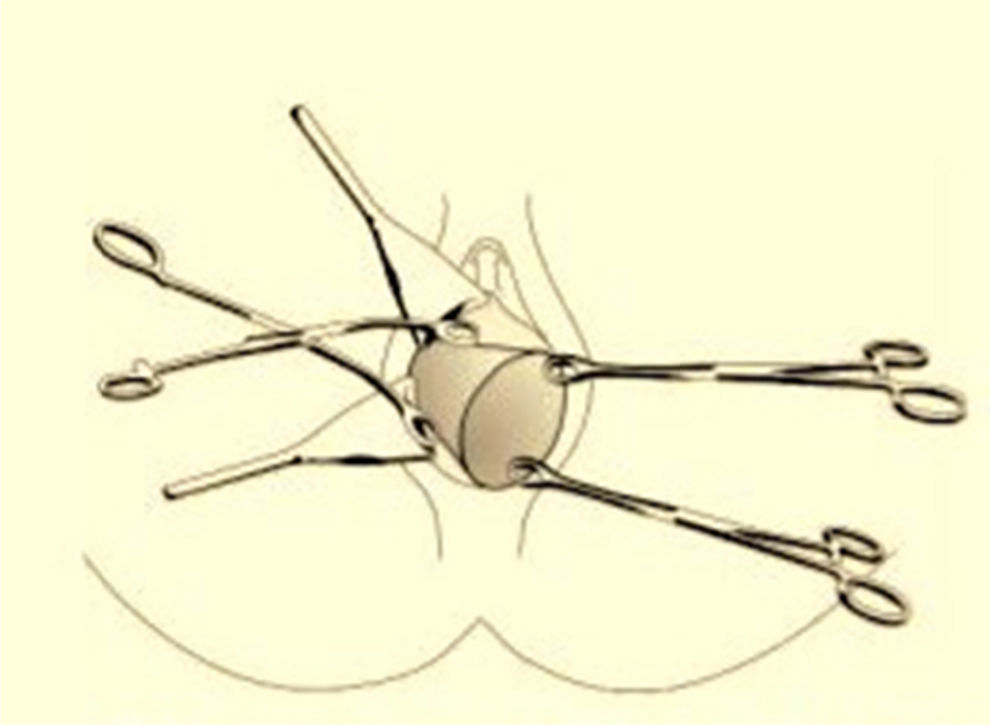
Then place a Foley catheter to control efflux of fluids, since absence of urine and its derivatives should be monitored.
- 9.
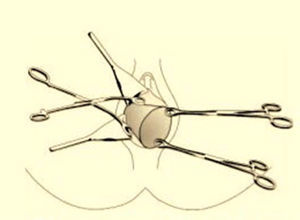
Once hemostasis is verified, the pair of straight Foerster forceps is removed and systematic examination for causes of obstetric hemorrhage is performed (Fig. 4).
- 10.
The clamping is retained until the cause of the bleeding has been solved, then the curved Foerster forceps are removed.
In refractory cases to this therapeutic approach, place again the curved Foerster forceps and transfer the patient to obstetric hysterectomy. Noteworthy, forceps must be removed when each uterine artery has been already ligated via abdominal.
The technique for clamping uterine arteries transvaginally has been used for more than 60 years,2 though several variations of the technique have been described. The above mentioned description of the clamping procedure constitutes a simple and effective technique, attainable by any physician at any healthcare facility. Moreover, neither highly specialized training nor complex resources are required for this technique, because the surgical instruments needed are habitually available at any obstetric care unit. Arterial occlusion by this technique provide the physician with valuable time to stabilize the patient, ensuring that therapeutic handling aimed to solve the origin of the bleeding is taking effect, or transfer the patient to reference centers for proper management.
Conflict of interestThe authors declare no conflict of interest.