We report a case of a 71-year-old Caucasian male, with significant past medical history of prostate cancer submitted to radical prostatectomy, chronic obstructive pulmonary disease (stage IIB, non-smoker) and hiatal hernia under omeprazole treatment.
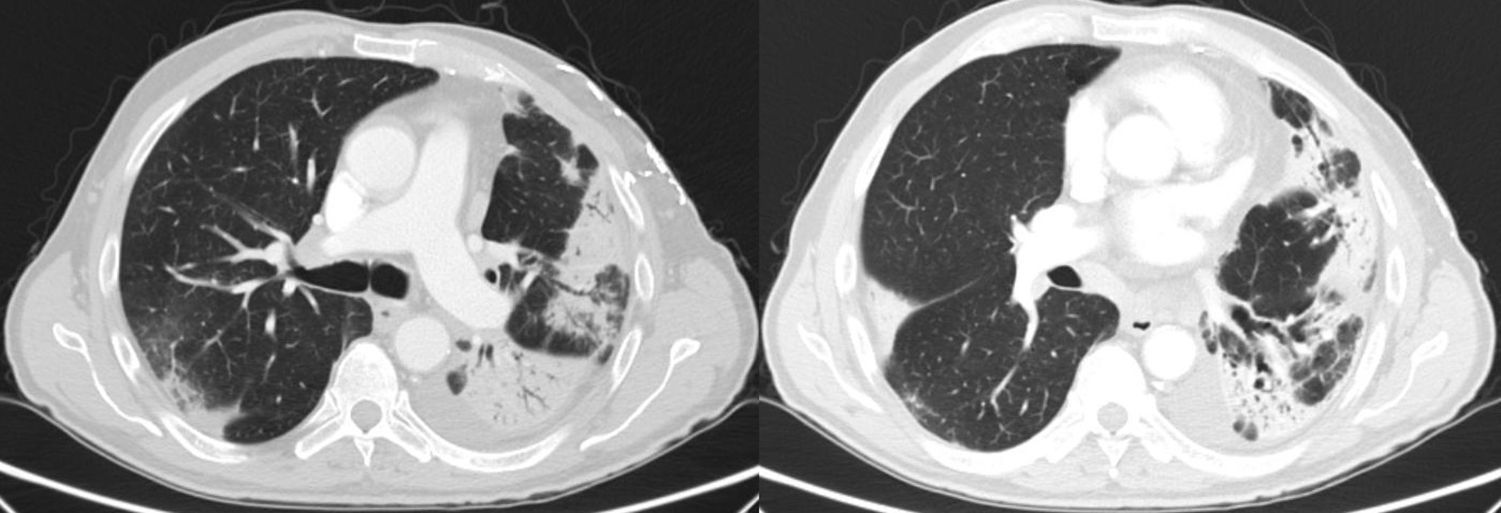
The patient presented to the emergency department complaining of dyspnea, cough, fever, asthenia and weight loss, over the previous 4 weeks. He denied exposure to identifiable allergens. On physical examination he presented fever, marked reduction of breath sounds and crackles more prominent in the left hemithorax. Laboratory assessment showed leukocytosis and neutrophilia, eosinophilia (1466/mm3), elevation of C-reactive protein (160mg/L, reference value <3mg/L) and hypoxemic respiratory failure (ratio pO2/FiO2 197mmHg). Thorax radiograph showed bilateral opacities and computed tomography (CT) revealed bilateral consolidation areas and small pleural effusion (Fig. 1).
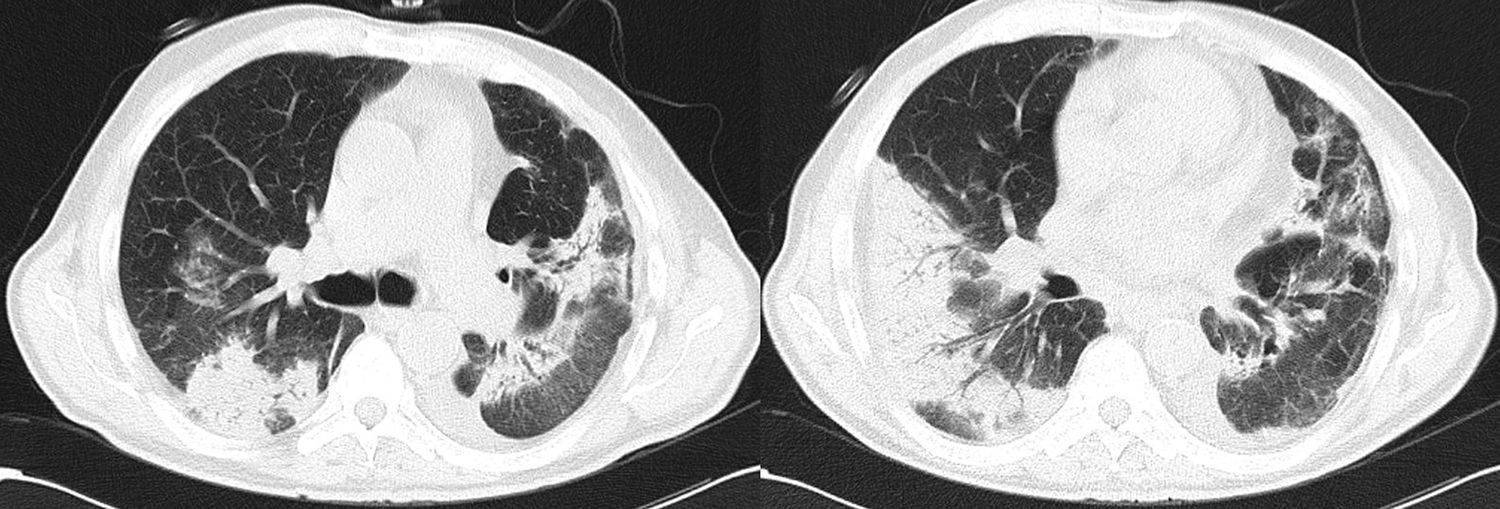
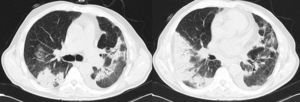
The patient was admitted to the Internal Medicine ward, with the diagnosis of community acquired pneumonia, under amoxicillin/clavulanate plus azithromycin. Treatment was switched to imipenem/cilastatin plus vancomycin due to poor evolution and thorax CT was repeated revealing migratory subpleural consolidations (Fig. 2). Several other tests to exclude infections (blood cultures; sputum Gram and acid-fast stain, bacterial, fungal and mycobacterial culture; sputum polymerase chain reaction for respiratory viruses; urinary pneumococcal and Legionella antigens, HIV) were negative, as well as for connective tissue diseases (antinuclear antibody, rheumatoid factor, anti-centromere antibody, anti-dsDNA, anti-ENA), and neoplasia (esophagogastroduodenoscopy, colonoscopy, abdominopelvic CT, and prostate specific antigen test). Bronchoscopy with bronchoalveolar lavage was not performed due to significant respiratory failure. The diagnosis of organizing pneumonia was confirmed after transthoracic needle biopsy was done, which revealed excessive proliferation of granulation tissue, with bronchiolar intraluminal polyps and mild lymphoplasmocitary infiltrate in the alveolar walls, without eosinophils or giant cells.
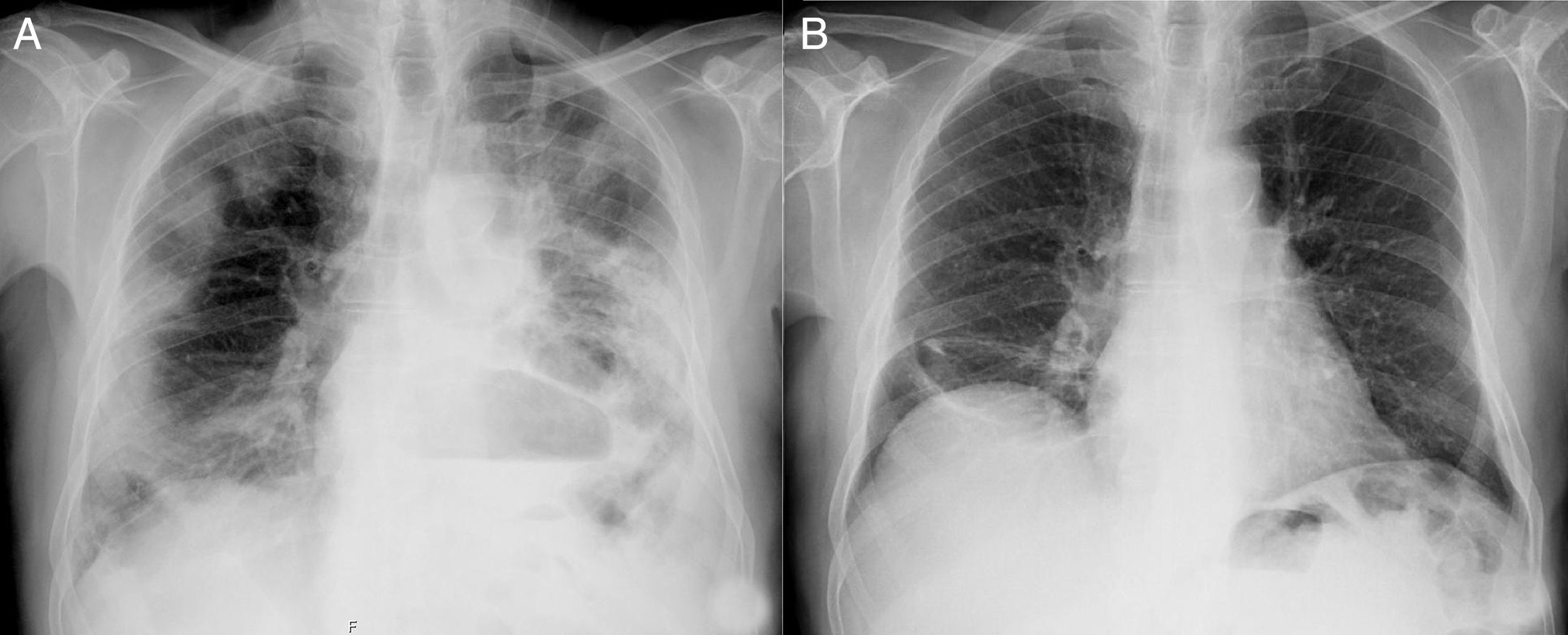
After exclusion of any possible and identifiable cause, a diagnosis of cryptogenic organizing pneumonia (COP) was made. High-dose glucocorticoid therapy with intravenous methylprednisolone 1000mg/day, for five days, was initiated with rapid clinical improvement and reduction of inflammatory biomarkers. Then oral prednisolone 1mg/kg per day was continued and gradually tapered over 6 months. A thorax radiograph was repeated two months after discharge (Fig. 3).
Cryptogenic organizing pneumonia is a subtype of interstitial lung disease and the idiopathic form of organizing pneumonia (formerly called bronchiolitis obliterans organizing pneumonia), affecting distal bronchioles, respiratory bronchioles, alveolar ducts, and alveolar walls.1,2
In a patient with a compatible clinical history, in the absence of a contributing factor, the diagnosis may be suspected from the characteristic radiographic features, such as: the presence of multiple opacities, usually bilateral, peripheral and migratory. However its diagnosis depends upon demonstration of the typical histopathologic features. It is impossible to differentiate COP from secondary organizing pneumonia based on radiologic or histology findings. Hence, a careful review of the patient's history, physical examination, and underlying diseases is needed to determine whether COP is indeed cryptogenic.1–3
Conflicts of interestThe authors declare no conflicts of interest.