Polymyalgia rheumatica is an inflammatory rheumatologic condition that occurs frequently in the elderly. It has been, although infrequently, associated with malignancies, in a synchronous or closely time-related appearance. In such circumstances, polymyalgia rheumatica is considered to be a paraneoplastic syndrome and is often atypical in presentation with poor response to glucocorticoid treatment. We report the case of a 79-year-old woman in which the simultaneous diagnosis of polymyalgia rheumatica and lung adenocarcinoma was made. Rheumatologic symptoms responded partially to anti-inflammatory medication, with further response to lung cancer targeted chemotherapy.
Polymyalgia rheumatica (PMR) is a clinical syndrome that most commonly affects women over fifty and classically associates with giant-cell arteritis.1 It is characterized by stiffness and aching of musculature, predominantly muscles of the pelvic girdle, neck, shoulders and upper arms.1 PMR typically presents with abnormally elevated sedimentation rate (ESR) and/or C-reactive protein (CRP) and frequently responds to small doses of glucocorticoids.1,2 Imaging studies commonly reveal inflammation of the bursas and of the periarticular structures.3 Diagnosis is based on the provisional American College of Rheumatology and on the European League Against Rheumatism classification criteria.1
Besides being a commonly unrecognized condition, it can also be concomitant with occult neoplasia.4 The association between rheumatologic disorders and malignancy – paraneoplastic rheumatologic syndromes – is intriguing and mainly based on the temporal concurrence of both entities.4 In such cases, the classic treatment used for non-neoplastic rheumatologic syndromes often courses with poor response rates, and symptoms more often subside with treatment of the underlying malignancy.5
Atypical PMR is believed to be more frequently associated with malignancy, predominantly when metastatic dissemination has already occurred.5 PMR is considered atypical when younger patients are affected, presentation is with asymmetrical long-lasting myalgia and arthralgia, and with lower or higher ESR and/or poorer or slower response to glucocorticoids therapy than expected.5
We report a case of an elderly woman diagnosed with pulmonary adenocarcinoma which presented concomitantly with a PMR syndrome.
Case reportA 79-year-old female presented to our hospital with one-month progressive pain of the right shoulder and elbow irresponsive to analgesia. She had symmetric polyarthralgias lasting over one year, and shoulder and hip morning stiffness. She complained of asthenia and she had involuntary lost 7kg during the previous year. She neither had history of fever nor other symptoms. She had no past history of autoimmune, infectious or neoplastic diseases, recent trauma or travelling. Furthermore, she had no history of smoking or exposure to known carcinogens. She had arterial hypertension and chronic kidney disease (stage 4 of National Kidney Foundation) attributed to hypertension.
On physical examination, she was hemodynamically stable and had no fever. Her body mass index was 22.9kg/m2. She had an aortic systolic murmur on cardiac auscultation. She had symmetric bimalleolar oedema and a non-pitting oedema from the third distal part of the right arm till the elbow. Extension and flexion of the right arm was painful and limited. There were no other associated local inflammatory signs. No other joints were involved and there were no cutaneous lesions. Physical examination was otherwise normal, namely there were no masses on mammary examination and no palpable adenopathies.
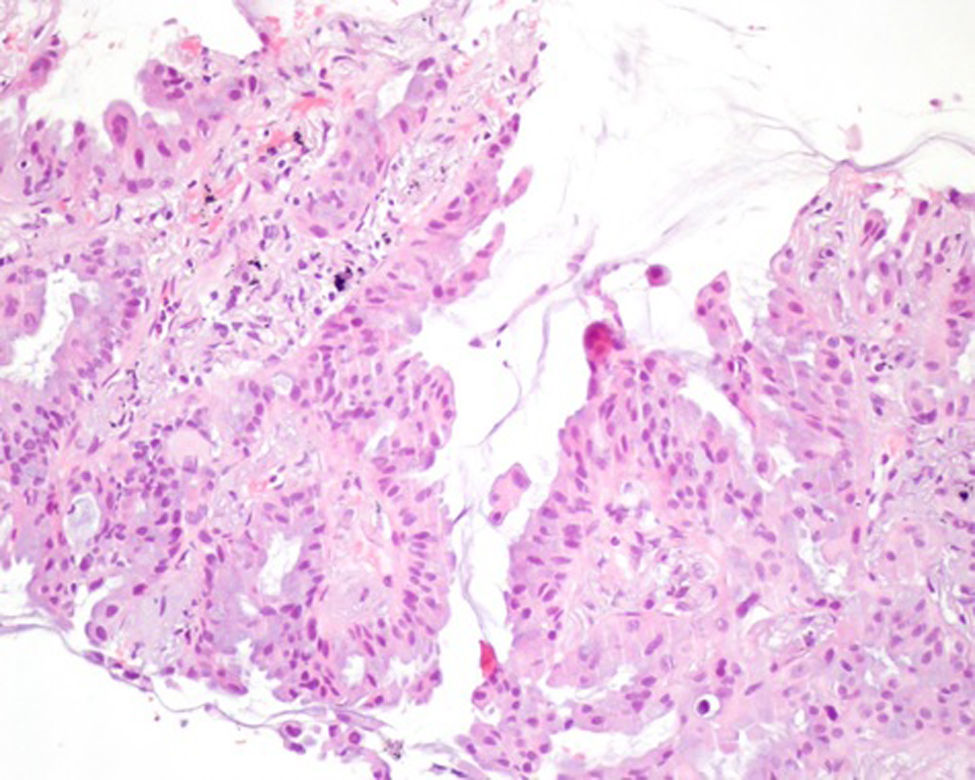
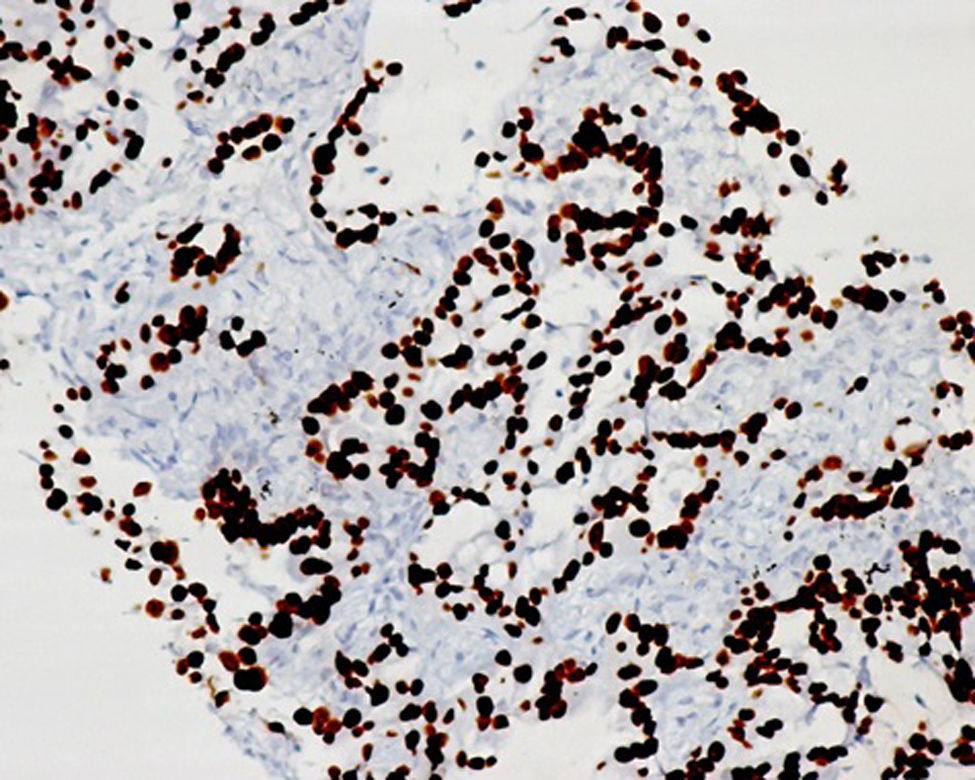
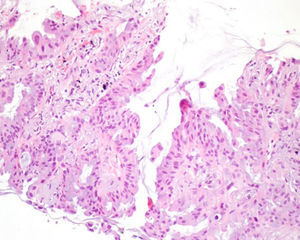
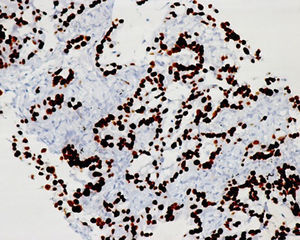
She had a microcytic normochromic anaemia with a haemoglobin of 11.8g/dL, normal leucocyte count and formula, normal platelet count and a CRP of 66mg/L. Urea was 71mg/dL, creatinine level 1.65mg/dL and she had no electrolytic disturbances. An ultrasonography of the right arm revealed a heterogeneous articular effusion of the elbow suggesting arthritis, complete rupture of the supra-spinous tendon and biceps tenosynovitis. The radiographic image of the right arm showed a lesion in the humerus possibly suggestive of a lytic process. Further blood tests showed: hypoalbuminaemia (36.8g/L); total calcium 4.9mEq/L; increased lactic dehydrogenase (396mg/dL); liver enzymes revealed no cytolysis, slightly increased gamma-glutamyl transferase (35U/L) and alkaline phosphatase (125U/L) and normal levels of total and direct bilirubin; ESR was elevated (75mm/h); iron kinetics showed a decreased iron saturation of 11%. The protein electrophoresis was normal. Abdominal ultrasonography showed no lesions or organomegalies. The thoracic radiography revealed a mass in the right pulmonary third, raising the suspicion of a pulmonary neoplastic process (Fig. 1) and transthoracic needle biopsy diagnosed a pulmonary adenocarcinoma (Figs. 2 and 3). Bone radiographies of the hands, feet, ankles, knees and hip showed diffuse osteopenia and degenerative lesions of bone and joints with no clear pathological significance. The immunologic study was unaltered.
Clinical, laboratory and imagiological results led to suspicion of PMR as a paraneoplastic rheumatologic syndrome. Low dose corticotherapy was initiated with only partial relieve of pain and the asthenic symptomatology; analytical inflammatory parameters showed a slight decrease. Since algic complaints of the right arm attributed to the metastatic lytic lesion of the humerus persisted, she was submitted to a course of directed radiotherapy with symptomatic response.
The patient was diagnosed with a stage IV lung adenocarcinoma, with positivity to epidermal growth factor receptor, and started therapy with erlotinib with further clinical response of algic symptoms and partial imagiological response.
She was hospital-readmitted four months after initiation of chemotherapy because of erlotinib-related toxicodermia and concomitant fungal infection, with worsening of her algic complaints and of her ability to perform daily life activities. Erlotinib was discontinued and palliative care was optimized. She died at home, two-months later.
DiscussionAlthough possibly associated with many types of malignancies, the most frequent malignant neoplasm associated with paraneoplastic syndromes is lung cancer, occurring in 10% of these patients.6 Several rheumatologic syndromes have been reported to be associated with lung malignancy.6 Rare cases of concurrent presentation of pulmonary cancer and PMR have been reported in the literature.7,8 The association of PMR and malignancy is still controversial. Some authors have reported an increased risk of cancer in the first six months to one year after the diagnosis of PMR and giant cell arthritis while others have found no association.4,9 This association seems to be particularly true in patients presenting with atypical PMR.4,9
In our patient, there was temporal association between the onset of rheumatologic symptoms and the diagnosis of lung cancer, although cause-and-effect relation cannot be established. Symptoms partial improvement with low-dose corticosteroid therapy and further relieve with chemotherapy supports the diagnosis of atypical PMR, which is a recognized cancer associated rheumatologic syndrome.
Extensive search for occult malignancy is not recommended in PMR; however, its association with malignancy should be kept in mind, particularly in the case of atypical PMR.
Conflict of interestsThe authors have no conflict of interests to declare.