Dermoid cysts of the uterus are extremely rare. A case of an asymptomatic dermoid cyst in the previous caesarean section scar is reported in a 39-year-old woman who presented for pre-conception evaluation. A nodular lesion of the uterus was identified through transvaginal ultrasound examination and magnetic resonance imaging and its characteristics are described. The first treatment option was hysteroscopic resection but complete removal could not be achieved. Surgical excision is likely to be the definitive treatment and a hysterectomy will be proposed to the patient after she completes her family. Our literature review indicates that this is the first case of a dermoid cyst located in the previous caesarean section scar.
Cistos dermoides do útero são extremamente raros. Este é um relato de caso de cisto dermoide assintomático na cicatriz de cesariana preexistente em mulher com 39 anos que se apresentou para avaliação pré-concepcional. Foi identificada uma lesão nodular por exame ultrassonográfico transvaginal e ressonância magnética; descrevemos suas características. A primeira opção terapêutica foi a ressecção histeroscópica, mas não foi possível fazer uma remoção completa. É provável que a excisão cirúrgica seja o tratamento definitivo; será proposta uma histerectomia à paciente, depois de ter completado sua família. Nossa revisão da literatura indica que este é o primeiro caso de cisto dermoide localizado em uma cicatriz de cesariana preexistente.
Dermoid cysts are the most common germ cell tumours and are composed of two or more germ layers (ectoderm, mesoderm or endoderm). In the majority of cases they are located in the testicles or ovaries but extragonadal teratomas can occur in 1–2% of cases and are found in mid-line structures.1 This report examines a rare case of a dermoid cyst located in the previous caesarean section scar.
Case descriptionAn asymptomatic a 39-year-old female patient came to our department for a pre-conception evaluation appointment. She had a medical history of type 1 diabetes mellitus since the age of 28, and autoimmune thyroiditis. She was taking metformin, levothyroxine and insulin delivered through an infusion pump. Regarding her gynaecologic history, she was 10 years old at menarche and her menstrual cycles were regular with 5 days bleeding. She had not had any sexually transmitted diseases. She was a Gravida 1, Para 1 and had been submitted to an emergency caesarean section due to HELLP Syndrome 7 years earlier, giving birth to a healthy female weighing 4160g. No complications during or after the caesarean section were reported. There was no history of other surgical procedures. In the family history, her father had had a gastric malignancy and undergone surgical treatment.
A speculum examination was performed and no lesions were found in the cervix. She did not have any abnormal discharge. On bimanual palpation, the uterus was slightly enlarged but no other anomalies were identified. Her vital signs were stable and the physical exam was otherwise normal.
A cervical smear had been recently conducted and was normal.
A transvaginal scan was performed, revealing a regularly shaped uterus with homogeneous myometrium. A diffusely echogenic avascular ovular mass was identified in the inferior segment of the uterus, in the anterior wall, measuring 37.2mm×18.7mm×29.2mm. The mass did not seem to communicate with the cervical canal. The endometrium was smooth, measuring 15.9mm. Both ovaries had a normal morphology, the right measuring 27.6mm×26.5mm and the left 26.2mm×15.8mm. There was no free fluid in the pouch of Douglas.
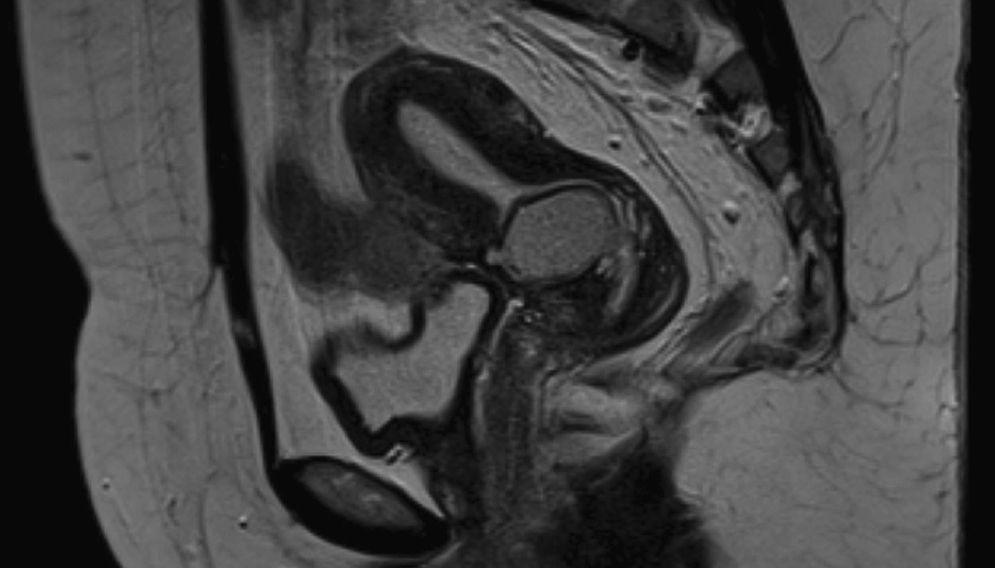
Magnetic resonance imaging of the pelvis was performed in order to further characterise the mass. It showed a 3cm regularly shaped nodular lesion located in the previous caesarean section scar, hyperintense on T2 and with slight hypersignal on T1. The lesion occupied the uterine cavity and extended to the endocervix, was submucous and contained material with high protein content or blood (Fig. 1). Both ovaries looked normal. There were no adenopathies or free fluid.
This patient presented with a uterine/cervical mass that could be an endocervical or endometrial polyp, a submucous fibroid or other benign neoplasia of the uterus. Although less common, malignant neoplasia of the cervix or uterus was also considered. In view of her history of caesarean section, other possible diagnoses included deficient scar or implanted foetal tissue in the previous caesarean section scar.
Treatment options were discussed with the patient and it was decided to perform a hysteroscopy under general anaesthesia for biopsies and surgical excision of the mass. The patient's consent was obtained.
During the hysteroscopy, a 3cm nodular structure was seen in the anterior aspect of the lower uterine wall, located in the previous caesarean section scar. It contained elastic solid material and a whitish pasty material that seemed to be sebum. The uterine cavity was normal in shape and no intracavitary lesions were seen. The nodular structure in the anterior wall was excised using micro instruments and sent for histological examination. The procedure was uneventful but the complete removal of the lesion could not be confirmed.
Histology revealed endocervical tissue partly coated by endocervical mucosa and by endometrial type tissue under which a lesion with trilinear dermoid cyst characteristics was found. In conclusion, it was a trilinear dermoid cyst in the transition of the endocervix to the inferior segment of the uterus.
In the follow-up period 4 months after the procedure, the patient was asymptomatic and aimed to conceive in the near future.
To assess whether the lesion had been totally removed or not, a hysteroscopy was performed and a small lesion was still identified in the previous caesarean section scar. Given its proximity to the bladder wall, another surgical resection was not recommended to the patient and following discussion of the options she opted for conservative management and surveillance.
Due to the benign nature of the lesion, the patient was encouraged to stick to her plans and attempt to conceive. We will follow her up and a potential pregnancy will be monitored thoroughly. The patient was advised to take medical care if experiencing severe abdominal pain, abnormal vaginal bleeding or fever. Besides clinical surveillance, she was offered transvaginal ultrasound and blood tests every 3 months to monitor her condition. Later on, the treatment options for removing the dermoid cyst may include hysterectomy.
DiscussionThe uterus is a very rare site for the development of a dermoid cyst. The first reported case of dermoid cyst of the uterus was by Mann in 19292 and since then, we have found 21 cases mentioned in English literature.1–9 Most of these were cervical masses or polyps.
The clinical presentation of uterine dermoid cysts includes abnormal uterine bleeding, cervical polyps, pelvic pain, vaginal discharge, and enlargement of the uterus.8 In this case, the patient was asymptomatic and her uterus was just slightly enlarged, which, all together, did not point to suspicious diagnosis. This nodular lesion of the uterus was an unexpected finding in the imaging studies.
Our review of the literature found no description of sonographic appearances of uterine dermoids. In dermoid cysts located in the ovary, the most common ultrasound features are the presence of a ‘white ball’ (consisting of hair and sebum), long echogenic lines and prominent echogenic dots in cyst fluid (caused by hair floating freely in non-fatty fluid), and shadowing.10 None of these features were present in the scan of the dermoid cyst in the previous caesarean section scar. Another case report mentioned that none of typical ultrasound features were seen in a case of uterine dermoid cyst.8
The treatment options for dermoid cysts of the uterus have been tumorectomy and radical hysterectomy with or without pelvic and/or paraaortic lymphadenectomy. Those of the uterine cervix can also be performed by conisation.11
In our case, the patient wished to preserve her fertility and a hysteroscopy was performed. Resection of the uterine mass was attempted but complete removal could not be achieved. The proximity of the lesion to the bladder prevented further resection because of the risk of damage to other organs or hysterectomy.
Hysteroscopy is a minimally invasive procedure that can be used to diagnose and treat many intrauterine and endocervical problems.12 Inspection of the caesarean scar is an indication. Operative hysteroscopy has been used for the treatment of caesarean-induced defects in the uterus,13,14 but we found no mention of this procedure in dermoid cysts.
The occurrence of malignancy arising from a dermoid cyst in any location is a rare phenomenon, estimated to appear in 0.5% of cases.1 Given the benign nature of this lesion, we believe that conservative management and surveillance is a safe option for the time being. Other uncommon dermoid cysts complications include rupture, infection and haemolytic anaemia.15 Although we found no reference to a follow-up plan, we decided to continue to observe the patient and perform transvaginal ultrasound and blood tests every 3 months. Blood tests for germ cell tumours should include complete blood count, liver and renal function, α-fetoprotein, β-human chorionic gonadotrophin, and lactate dehydrogenase.16
Surgical resection is likely to be the definitive treatment and cure for uterine dermoid cysts. A hysterectomy will be suggested to the patient as soon as she completes her family.
The impact of the dermoid cyst of the uterus on pregnancy is uncertain and we found no research information on this topic. As with submucous fibroids, it seems reasonable to assume that in this case implantation and/or placentation could be compromised and thereby predispose to miscarriage.17 We also anticipate a higher risk of uterine rupture and increased likelihood of caesarean section.
Uterine dermoid cysts are extremely rare and their actual incidence is unknown. To the best of our knowledge, this is the first case of a dermoid cyst located in the previous caesarean section scar and this is also the first reported case of a new diagnostic and treatment approach to uterine dermoid cysts, which is hysteroscopy.
Conflicts of interestThe authors declare no conflicts of interest.
The authors thank the members of the Pathology and Radiology Department for histological results and magnetic resonance imaging, respectively.