The aim of this study was to evaluate the uterine cavity in cases of endometriosis associated infertility using office hysteroscopy.
Study designA retrospective observational analytical study.
Patients and methodsThe study conducted on 50 women with endometriosis diagnosed by laparoscopy seeking fertility treatment between December 2013 and October 2015. The study was approved from Ethical committee board of the faculty of Medicine Alexandria University. After explanation of the study objectives and procedures to all eligible women, informed written consent was signed. Thorough history taking, clinical examination and vaginal ultrasound examination was conducted to all participants. Office Hysteroscopy was done in the early proliferative phase using normal saline as a distention medium. All data were pulled from the reports at Elshatby Maternity University Hospital.
ResultsThe age of the study group was ranging from 20 to 34 years with the mean of 29 years±3 years. 42 cases were primary infertility counting for 84% of patients and 8 cases were secondary infertility counting for 16% of patients. This reflects the strong impact of endometriosis on fertility. Normal uterine cavity was diagnosed in 35 cases representing 70% of the studied patients group. 10 cases had endometrial polyps representing 20% of the studied patients group. 5 cases had a uterine septum representing 10% of the studied patients group. 2 cases had a hypo plastic uterus in addition to uterine septum representing 4% of the studied patients group. Normal uterine cavity were diagnosed using hysteroscopy in 63.0% (18/23) in women having ovarian endometrioma while this normality was 78.3% (17/27) in women without endometrioma however, The prevalence of endometrial polyp was 25.9% in cases with endometrioma and 13% in cases without endometrioma. Cases with a uterine septum were 7.4% (2/23) of cases having ovarian endometrioma and 13.0% (3/27) of cases without it. Two cases with endometrioma out of 23 cases were diagnosed to have hypoplastic uterus. No uterine abnormalities were found in stage 1 endometriosis in contrast to the presence of 53.2% of patients with a uterine abnormality in stage 2. Also stage 3 patients were all having a normal uterine cavity while only 72.4% of patients with stage 4.
ConclusionFrom the results of this study we can conclude that there is a High prevalence of endometrial polyps in cases of endometriosis. Also there is a High prevalence of uterine anomalies in cases of endometriosis. Still, we neither cannot recommend hysteroscopy as a routine in any endometriosis patient undergoing laparoscopy.
Avaliar a cavidade uterina em casos de infertilidade associada à endometriose, com uso da histeroscopia no consultório.
Modelo de estudoRetrospectivo analítico observacional.
Pacientes e métodosFoi feito em 50 mulheres com endometriose diagnosticada por laparoscopia e que estavam em busca de tratamento de fertilidade entre dezembro de 2013 e outubro de 2015. O estudo foi aprovado pela Comissão de Ética da Faculdade de Medicina, Universidade de Alexandria. Em seguida à explicação dos objetivos e procedimentos do estudo a todas as mulheres qualificadas, foi obtido consentimento livre e informado por escrito. Em todas as pacientes foi obtida uma história minuciosa e foram feitos o exame clínico e um exame vaginal por ultrassom. A histeroscopia no consultório foi efetuada na fase proliferativa inicial; empregamos salina normal como meio de distensão. Todos os dados foram obtidos de prontuários no Hospital Universitário-Maternidade Elshatby.
ResultadosA faixa do grupo de estudo foi de 20-34 anos, com média de 29±3. Foram diagnosticados 42 casos de infertilidade primária (84% das pacientes) e 8 de secundária (16%). Esse achado reflete o vigoroso impacto da endometriose na fertilidade. No grupo de pacientes estudadas, foram observados: cavidade uterina normal em 35 casos (70%), pólipos endometriais em 10 casos (20%), septo uterino em 5 casos (10%) e útero hipoplásico, além de septo uterino, em 2 casos (4%). Cavidades uterinas normais foram diagnosticadas por histeroscopia em 63% (18/23) das mulheres com endometrioma ovariano, mas em 78,3% (17/27) das mulheres sem endometrioma. A prevalência de pólipos endometriais foi de 25,9% nos casos com endometrioma e de 13% nos casos sem endometrioma. Septo uterino foi diagnosticado em 7,4% (2/23) dos casos com endometrioma ovariano e em 13% (3/27) dos casos sem essa doença. Dos 23 casos com endometrioma, 2 mulheres foram diagnosticadas com útero hipoplásico. Não foram observadas anormalidades uterinas nas pacientes com endometriose de estágio I, em contraste com a presença de 53,2% das pacientes com uma anormalidade uterina no estágio 2. Todas as pacientes no estágio 3 tinham cavidade uterina normal, enquanto que esse achado ocorreu em apenas 72,4% das pacientes no estágio 4.
ConclusãoHá alta prevalência de pólipos endometriais em casos de endometriose. Do mesmo modo, há grande prevalência de anomalias uterinas em casos de endometriose. Ainda assim, não podemos recomendar a histeroscopia como procedimento de rotina em qualquer paciente com endometriose que passe por uma laparoscopia.
The association between endometriosis and infertility is complex and controversial. Virtually every aspect of reproduction in women with endometriosis has been investigated. Although advanced stages of endometriosis may manifest easily recognizable infertility factors, such as tubal distortion/obstruction, the mechanisms underlying reproductive dysfunction in women with minimal or mild endometriosis are more subtle.1
Several studies have suggested an impairment of implantation in patients with endometriosis. This may be due to intrinsic deficiencies within the uterus, extrinsic co-factors such as the peritoneal fluid, oocytes or the embryos themselves.2 Evidence suggests that eutopic endometrium from women with endometriosis has some fundamental differences compared to eutopic endometrium from women without endometriosis. These include a variety of anomalies in structure, proliferation, immune components, adhesion molecules, proteolytic enzymes, steroid and cytokine production and responsiveness, gene expression and protein production.3 The secretory levels of urokinase plasminogen activator and prostaglandin F2α are increased in endometrial tissues of women with endometriosis compared with patients without the disease, which leads to abnormal endometrial growth.4 Elevated 17β-estradiol concentrations in peritoneal fluid of patients with endometriosis have been documented, that stimulates endometrial growth.5
Structural and ultrastructural defects in preovulatory endometrium from women with minimal or mild endometriosis have been identified by light scanning and transmission electron microscopic studies.6 These analyses revealed heterogeneity of the endometrial surface epithelium in 77% of patients with endometriosis and in 16% of the non-endometriosis controls. This suggests that abnormal endometrial growth due to the presence of endometriosis affects not only tissues other than endometrium but also directly affects endometrium itself.7
Endometrial polyps are typically localized overgrowth of the mucosa. Endometrial polyps are a common gynecologic disorder whose incidence is unknown because many polyps are asymptomatic.8 The prevalence of endometrial polyps is increased significantly in infertile women, in one large randomized controlled study conducted on more than 2500 infertile women the prevalence was up to 8%. The similar pathological characteristics of endometriosis and endometrial polyps suggest a possible association between the two pathologies. It is not known whether endometrial polyps are a risk factor or an etiologic factor in endometriotic infertility, and there are very few reports in the literature that investigate this association. Some studies have shown a higher frequency of endometrial polyps in patients with endometriosis compared with those without the disease.9
Anatomical uterine malformations are also linked to endometriosis. Both obstructive and non-obstructive uterine anomalies increase the risk of endometriosis.10 The incidence of congenital uterine anomalies in the general population is 0.1–3%, which is significantly higher in patients with infertility.11
ObjectivesThe aim of this study was to evaluate the uterine cavity in cases of endometriosis associated infertility using office hysteroscopy.
Patients and methodsA retrospective observational analytical study that was conducted on 100 women with endometriosis diagnosed by laparoscopy seeking fertility treatment between December 2013 and October 2015. The study was approved from Ethical committee board of the faculty of Medicine Alexandria University.
Infertile women with proven diagnosis of endometriosis by laparoscopy whom aged from 20 to 35 years were recruited from the reports of ELshatby Maternity University Hospital. Women with previous history of uterine surgeries as well as whom on hormonal treatment within 6 months from the start of the study were excluded from participation. Review of history taking, clinical examination and vaginal ultrasound examination was conducted to all participants. Office Hysteroscopy results were also reported.
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0.12,13 Qualitative data were described using number and percent. Quantitative data were described using range (minimum and maximum) mean, standard deviation and median.
ResultsThe age of the study group was ranging from 20 to 34 years with the mean of 29 years ±3years. 42 cases were primary infertility counting for 84% of patients and 8 cases were secondary infertility counting for 16% of patients. This reflects the strong impact of endometriosis on fertility.
Regarding the stages of endometriois, 4 cases were diagnosed to have stage one endometriois, 12 cases with stage 2 endometriosis however in 2 cases we found combined abnormalities in he form of uterine septum and hypoplastic uterus, 4 cases were in stage 3 endometriois and finally 30 women were diagnosed to have stage 4 disease. Endometrioma was diagnosed in 23 cases represent 46% of the study sample.
Normal uterine cavity was diagnosed in 35 cases representing 70% of the studied patients group. 10 cases had endometrial polyps representing 20% of the studied patients group. 5 cases had a uterine septum representing 10% of the studied patients group. 2 cases had a hypoplastic uterus in addition to uterine septum representing 4% of the studied patients group as shown in (Table 1).
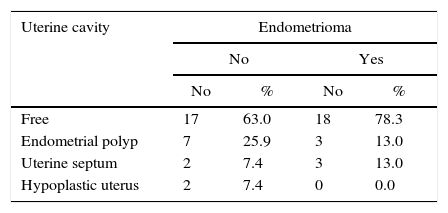
Normal uterine cavity were diagnosed using hysteroscopy in 63.0% (18/23) in women having ovarian endometrioma while this normality was 78.3% (17/27) in women without endometrioma. The prevalence of endometrial polyp was 25.9% in cases with endometrioma and 13% in cases without endometrioma. Cases with a uterine septum were 7.4% (2/23) of cases having ovarian endometrioma and 13.0% (3/27) of cases without it. Two cases with endometrioma out of 23 cases were diagnosed to have hypoplastic uterus as shown in (Table 2).
We also studied the relation between stage of endometriosis and the uterine cavity findings and our results indicated that No uterine abnormalities in stage 1 endometriosis in contrast to the presence of 53.2% of patients with a uterine abnormality in stage 2. Also stage 3 patients were all having a normal uterine cavity while only 72.4% of patients with stage 4. Statistical analysis of these finding showed non-significant results (Table 3).
The relation between type of endometriosis and the uterine cavity findings in the studied group of patients.
| Uterine cavity | Type of endometriosis | |||||||
|---|---|---|---|---|---|---|---|---|
| Stage I | Stage II | Stage III | Stage IV | |||||
| No | % | No | % | No | % | No | % | |
| Free | 4 | 100.0 | 6 | 46.2 | 4 | 100.0 | 21 | 72.4 |
| Endometrial polyp | 0 | 0.0 | 4 | 30.8 | 0 | 0.0 | 6 | 20.7 |
| Uterine septum | 0 | 0.0 | 2 | 15.4 | 0 | 0.0 | 3 | 10.3 |
| Contracted cavity | 0 | 0.0 | 2 | 15.4 | 0 | 0.0 | 0 | 0.0 |
Although many hypotheses exist to explain the relation between endometriosis and infertility, the precise mechanisms by which endometriosis leads to infertility remain unclear. This study was aiming to evaluate the uterine cavity in cases of confirmed diagnosis of endometriosis by laparoscopy.
The present study was a prospective descriptive analytical study while other studies were all retrospective controlled studies.9,12
Regarding the baseline characteristics of women included in the present work, the age of the studied patients group ranged from 22 to 43 years with a mean of 30.6±4.8 years. This agrees with the young age of other studies candidates. Shen et al. (2011) had a mean age of 31.0±4.2 years.9 While Kim et al. (2003) had a mean age of 30.5±3.7 years.14 The study of Matalliotakis et al. (2010) had a mean age of 29.6±4.0 years.15
Cases having primary infertility were 42 forming 84% of patients. 8 cases were having secondary infertility forming 16% of patients. Most of our endometriosis patients were nulliparous. This may reflect the effect of endometriosis on fertility.
In this study, we found that 30% of cases had abnormal uterine cavity. We found 10 patients having endometrial polyps representing 20%, 5 patients were having uterine septum representing 10% and 2 patients were having a contracted uterine cavity representing 4% of patients.
Endometrial polyps are typically localized overgrowth of the mucosa. The prevalence of endometrial polyps in infertile women varies greatly in the literature. In one study conducted upon 1000 infertile patients in 2004 the prevalence was up to 35%.16 A larger study was conducted upon 2500 infertile patients in 2010 reported a prevalence of 7.86% only.17
Endometrial polyps have a typical composition of glands, stroma and fibrous tissue. It has a typical pattern of vascular axis of arterialized spiral arteries that involves fibrous stroma and/or irregular glands. Functional endometrial polyps which are confined to hormonally responsive layer of the uterus are estrogen dependent. The exact pathogenesis of these benign lesions is not well known but hormonal dysfunction is the most accepted theory.18 Also, the similar pathological characteristics of endometriosis and endometrial polyps suggest a possible association between the two pathologies. It is not known whether endometrial polyps are a risk factor or an etiologic factor in endometriotic infertility, and there are very few reports in the literature that investigate the prevalence of endometrial polyps in cases of endometriosis. Kim et al. (2003) studied One hundred eighty-three infertile women, 92 with endometriosis and 91 controls without the disease. Endometrial polyps were found in 43 women (46.7%) with endometriosis and in 15 controls (16.5%).14 Shen et al. (2011) studied 431 infertile women, 158 cases with endometriosis and 273 without endometriosis. Endometrial polyps were found in 108/158 women cases (68.35%) with endometriosis and in 56/273 of the control participants (20.51%).9 These results agree with our results in the high prevalence of endometrial polyps in endometriosis patients. The difference in the prevalence of endometrial polyps between these studies could be the result of the number and study population of participants. Both studies were held in china with a consideration of the high prevalence of endometrial polyps in the control group.
Our study was not limited only to the prevalence of endometrial polyps but also we evaluated the uterine cavity for uterine anomalies, of which we found 7 cases representing 14% of the studied patients group. 5 cases were having uterine septum (10%) and 2 cases were having a contracted uterine cavity (4%).
Uterine septum is a congenital malformation of the uterus which is the most common mullerian duct anomaly constituting about 55%.19 The incidence of congenital uterine anomalies in the general population is 0.1–3%.20 Jayaprakasan et al. (2011) studied 1385 infertile cases of which 7 cases (0.5%) were having a uterine septum.21 Ioannis et al. (2010) studied 425 cases with endometriosis and 200 without endometriosis. They found 13 cases from 425 having a uterine septum representing 3%. The control group had only one case representing 0.5% of the studied patients group.15 This agrees with our results in having a higher incidence of uterine anomalies in relation to endometriosis.
Ovarian endometriomas are common manifestations of endometriosis. In our study, 23 cases were having ovarian endometrioma representing 46% of the studied patients group. The percentage of normal uterine cavity was high 78%.
All cases were classified according to the ASRM classification of endometriosis into 4 stages I, II, III and IV. We analyzed the frequencies of different uterine abnormalities in the four stages. When comparing the uterine cavity findings in the four stages, there was no statistical significance in the prevalence of uterine cavity findings in the four stages of endometriosis. This agrees with the results of Shen et al. (2011) and Kim et al. (2003) as they reported no statistical difference in prevalence of endometrial polyps with different stages of endometriosis.9,14
ConclusionFrom the results of this study we can conclude that there is a High prevalence of endometrial polyps in cases of endometriosis. Also there is a High prevalence of uterine anomalies in cases of endometriosis. Non-significant relation between uterine cavity pathology and presence of ovarian endometrioma in cases of endometriosis was demonstrated. And that the Stage of endometriosis does not affect uterine cavity findings in cases of endometriosis. We cannot recommend conducting hysteroscopy as a routine with laparoscopy in cases of endometriosis.
Conflicts of interestThe author declares no conflicts of interest.