Assess the effects of sensorimotor training on the functional autonomy levels of sedentary elderly people.
MethodsThe sample was composed of 30 women (sedentary, functionally independent, χ=65.03±4.93 year), divided randomly into two groups: control (CG, n=15) and experimental (EG, n=15). Tests developed by the Latin American Development for the Elderly Group (GDLAM) were used to evaluate autonomy. The EG was submitted to a sensorimotor program three times a week, involving 24 thirty-minute sessions. Data were processed using the SPSS program, with a 5% significance level.
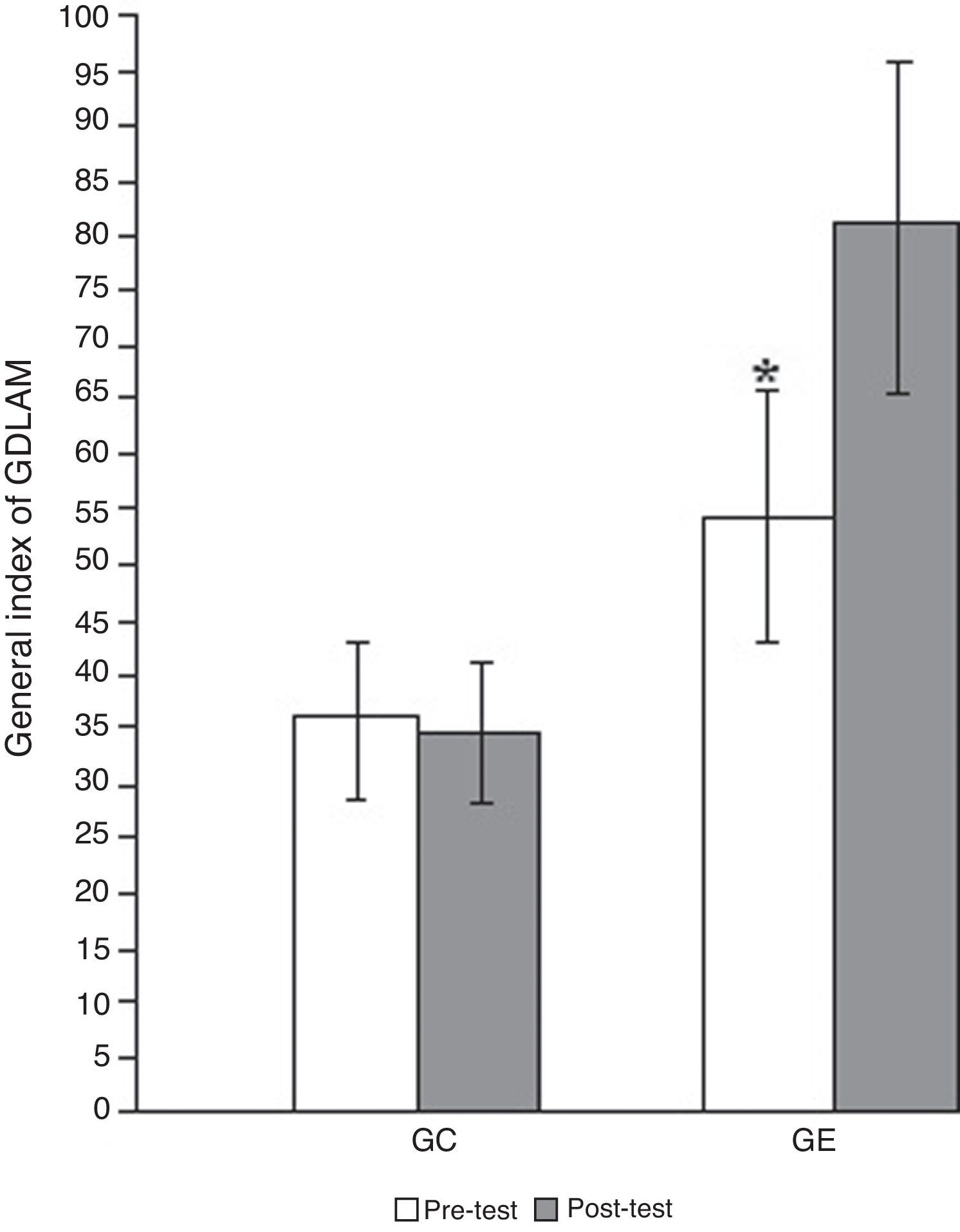
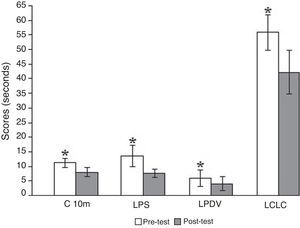
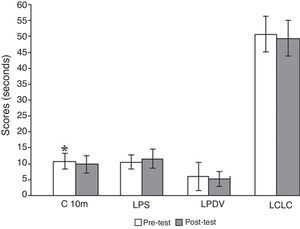
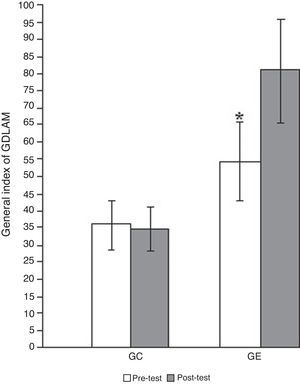
ResultsThe EG showed a significant reduction in execution time in all the tasks, while the CG only obtained a significantly better score on the 10-M walk test. Although the EG improved in the GDLAM index (Δ%=−30, 3%, p=0.0001), it remained at a “weak” level (GDLAM index >27.42).
ConclusionThe results demonstrate that sensorimotor training reduces the execution time of tasks, as well as improving functional performance in activities of daily living.
Evaluar los efectos del entrenamiento sensorio motriz en los niveles de autonomía funcional del anciano sedentario.
MétodoLa muestra se compuso por 30 mujeres (sedentarias, independientes funcionalmente, 65,03±4,93 años) divididas al azar en 2grupos: control (CG, n=15) y experimental (EG, n=15). Para la evaluación de la autonomía se utilizaron las pruebas del Grupo del Desarrollo Latinoamericano para la Madurez (GDLAM) antes y después de la intervención. El EG fue sometido a un programa de entrenamiento sensorio motriz, 3veces a la semana, la duración de cada sesión fue de 30 minutos y realizaron 24 sesiones. Los datos se procesaron con el programa SPSS, versión 19, adoptando nivel de significación de la p<0,05.
ResultadosEn el grupo experimental se constató una reducción significativa del tiempo de ejecución en todas las tareas, mientras el CG solo obtuvo resultado significativamente mejor en la prueba de caminata de 10m. En el índice general de GDLAM, el grupo experimental presentó mejora (Δ%=-30, 3%, p=0,0001), pero se mantuvo en un nivel «débil» (Índice GDLAM > 27,42).
ConclusiónLos resultados muestran que la práctica del entrenamiento sensorio motriz influye de forma positiva en la reducción del tiempo de ejecución de las tareas, lo que se relaciona con el mejor rendimiento funcional de las actividades cotidianas.
Avaliar os efeitos do treinamento sensório-motor sobre os níveis de autonomia funcional de idosos sedentários.
MétodosA amostra foi composta por 50 mulheres (sedentárias, funcionalmente independentes, 65,03±4,93 anos) divididas aleatoriamente em 2grupos: controle (CG, n=15) e experimental (EG, n=15). Para a avaliação da autonomia funcional foi utilizado o teste Grupo de Desenvolvimento Latino-Americano para a Maturidade (GDLAM) antes e após a intervenção. O grupo EG foi submetido a um programa de treinamento sensório-motor, 3vezes por semana, com duração de 30 minutos cada sessão, e foram realizadas durante 24 sessões. Os dados foram processados através do programa SPSS, versão 19, adotando nível de significância de p<0,05.
ResultadosNo grupo experimental foi constatada uma redução significativa do tempo de execução em todas as tarefas, enquanto que o grupo CG obteve resultados significativamente menores no teste de caminhada de 10m. No índice geral do GDLAM, o grupo experimental apresentou melhora (D%=-30, 3%, p=0,0001), porém se manteve em nível «fraco» (índice GDLAM >27,42).
ConclusãoOs resultados mostraram que a prática do treinamento sensório-motor influência de forma positiva na redução do tempo de execução das tarefas, relacionando-se com melhor rendimento funcional das atividades cotidianas.
Mobility is one of the most important aspects of physical function, especially as a prerequisite for executing activities of daily living (ADL) and maintaining independence.1 Thus, a significant decrease in the gait pattern of elderly individuals hinders the execution of activities such as walking, climbing up and down stairs, moving in and out of bed or a chair, personal hygiene, shopping and remaining active, thereby progressively compromising functional capacity.2,3
The elderly have reduced muscle strength, suffering from negative influence on the ability of sensory discrimination, with consequent loss of motor coordination, balance and proprioception.4–6
Likewise in elderly autonomous, there is a possibility that these defects, over time, may occur, affecting the pattern of movement and decreasing the individual's ability to walk and minimize the risk of falls. Since gait is a complex motor phenomenon, resulting from the interaction of neurological, musculoskeletal, vestibular and somatosensory systems and is one of the most important aspects of physical function and prerequisite for the execution of daily living (ADLs) activities, there may arise disability and functional dependence7–9 is important to test the efficacy of interventions aimed recover and extend the good operational status of the march, aiming to promote functional autonomy of the elderly.
During the aging process these suffer impairment due to various mobiles, joint, muscle and nerve factors, and also because of balance disorders6,10 resulting in limitations in ADLs that negatively affect the self-confidence of the elderly, hampering their execution, due to fear of falling or other physical, psychological or social factors. Moreover, these restrictions may progressively compromise the functional autonomy over time, creating an irreversible cycle, resulting in total dependence or even bed confinement.11
Functional autonomy is defined as follows: autonomy of action, referring to the notion of physical independence; autonomy of will, that is, the possibility of self-determination; and autonomy of thoughts, related to the possibility of judging any situation.12,13 Autonomy of action is also referred to as functional autonomy, describing the ability of an elderly individual to independently perform ADLs.12
Physical activity has produced positive effects on maintaining functional autonomy and is a preventive factor against functional limitations, that is, the inability to sustain normal daily tasks, in addition to enhancing performance in ADLs.14–15
Several studies have investigated the benefits of physical activity on functional autonomy;1,14,15 however, there is a lack in regards to the training of sensorimotor functional activities that simulate displacement influencing ADLs and therefore part of the functional autonomy protocols.
The aim of the present study was to assess the effects of sensorimotor training of the lower limb in sedentary elderly as part of functional autonomy.
MethodsSubjectsThirty sedentary, autonomous and functionally independent women, aged between 60 and 75 years (χ=65.03±4.93) and enrolled in the Physical Activity and Rehabilitation Program for Autonomy in the Elderly (PARPAE) at the Centro Universitário UnirG in Gurupi, Brazil, were randomly selected.
The following exclusion criteria were adopted: the need for walking aids or assistance from another person; suffering from cardiovascular diseases that limit physical exercise; visual acuity less than 0.3 by the Snellen Table16; use of ortheses; presence of neurological dysfunctions; orthopedic diseases of the lower limbs that limit ambulation; otoneurological alterations; participation in other physical exercise programs and attending less than 80% of the sessions.
In accordance with Resolution 196/96 and the Helsinki Convention,17 subjects were informed about study procedures and possible related discomfort, in addition to giving written informed consent.
The project was approved by the Human Research Ethics Committee of Universidade Castelo Branco (UCB/RJ), under protocol no. 0002/2009.
Diagnostic assessmentStudy participants were assessed for functional autonomy, according to the Latin American Development for the Elderly Group (GDLAM) protocol,12 adapted for this study to characterize functional autonomy status in the elderly.
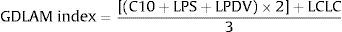
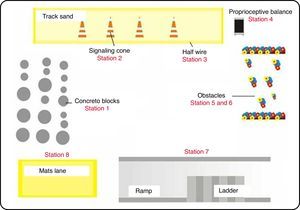
The assessment consisted of five tests, as follows: 10m Walk (C10m)18; getting up from a sitting position (LPS)19; getting up from the prone position (LPDV)20; getting up from a chair and moving around the house (LCLC).21 Scores are awarded based on time (seconds) required to execute tasks, such that the lowest time represents the highest level of functional autonomy. These tests are used to calculate the GDLAM index, classifying functional performance as very good<22.66; 22.66<good<24.97; 24.98<fair<27.42 and weak>27.42. The GDLAM index was calculated by normalization between the four autonomy tests. This calculation was elaborated from the following formula:
For the last test we used a wooden chair with a 50cm seat-to-floor height and no arm rest; a Cronobio SW 201 water resistant stopwatch (USA); an E.V.A. tatami mat (Brazil); and a Uyustools 50-cm professional measuring tape (USA).
For test the effect of the learning, the day before the intervention was teached until they properly execute the task. In the period preceding it and post intervention, all tests were performed in two trials with an interval of 5min, recording the shortest time achieved in the execution of each task. These times were compared with autonomy levels of the GDLAM protocol, in order to classify the elderly according to degree of functional autonomy.
InterventionAfter the pretest, subjects were randomly divided into the experimental group (EG n=15), submitted to a sensorimotor program and the control group (CG n=15). The EG underwent three 30min sessions per week for 8 weeks, followed by reassessment.
The CG met weekly for eight weeks and were informed that they would also be submitted to the same sensorial training after the conclusion of the study.
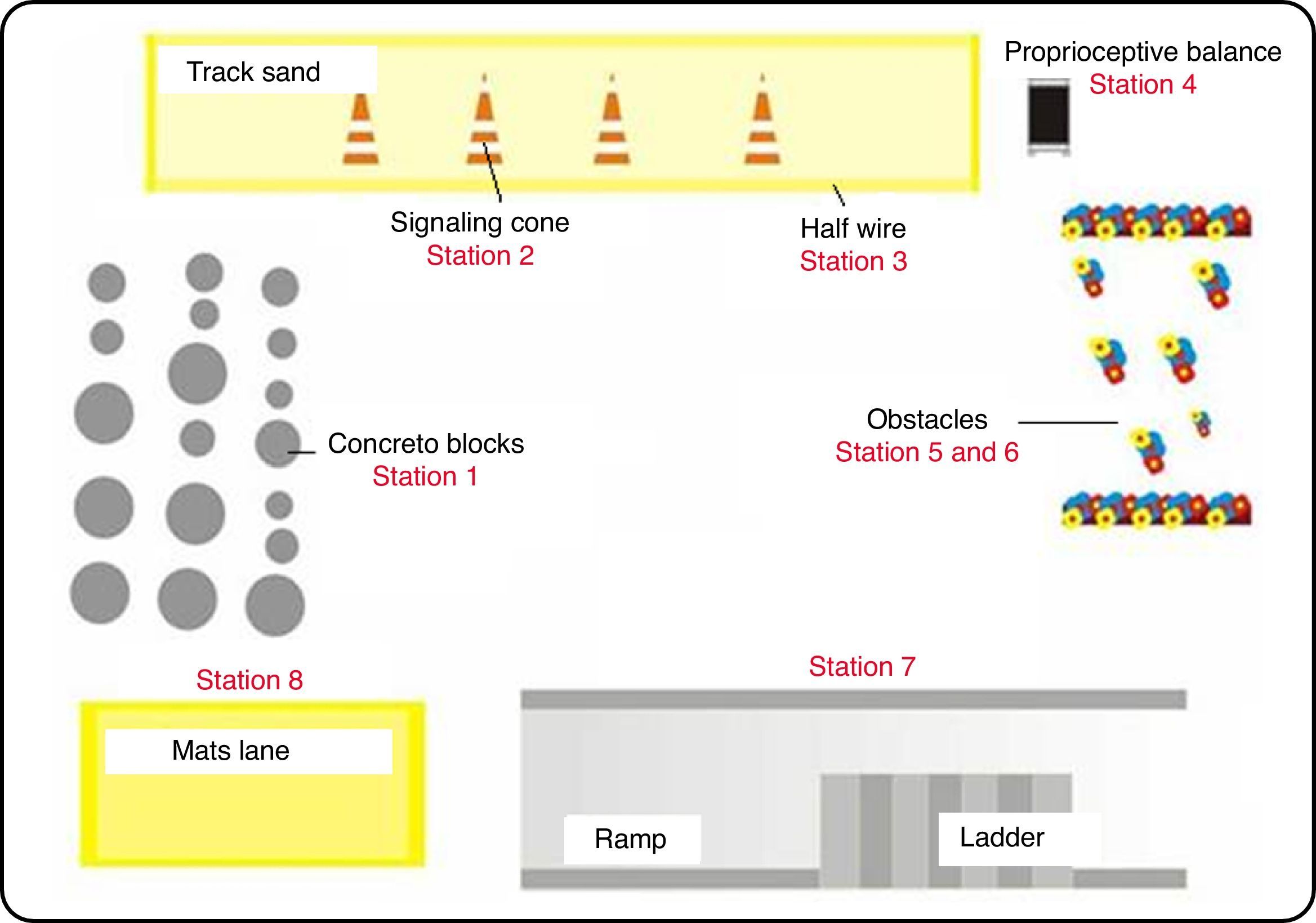
Training was conducted on a previously planned circuit established by PARPAE (Physical Activity and Rehabilitation for Autonomy in the Elderly Program), a community initiative supported by the federal agency FINEP (Research and Project Financing). The circuit was originally created in order to train the gait pattern, so it has tasks that simulate ADLs involving only the lower limbs. It has not been validated, but already there was a publication that demonstrated the effects of this circuit in the gait pattern of sedentary elderly.22 The circuit, denominated Circuit for Assessment and Development of Gait, Balance and Physical Conditioning in the Elderly, was built in a 15.84-meter-long room, containing eight stations designed for activities using proprioceptive and balance stimuli, as described below and illustrated in Fig. 1.
Station 1 – Walking over 35-cm-wide cylindrical blocks, ranging between 10 and 40cm in height, using alternate lower limbs and placing both feet on the block before proceeding to the next one. Blocks were arranged in two levels of difficulty: the first level had seven blocks with little variation in height while the second consisted of nine blocks with greater height variation, requiring more exercise intensity.
Station 2 – Stepping over five 0.75-cm-high signal cones, lying flat and placed 1m apart in a sandbox measuring 11m×1.10.
Station 3 – Walking along a curb 10-cm-high, 12-cm-wide and 11-m-long.
Station 4 – Standing on both feet for 20s with no hand support, in proprioceptive balance.
Station 5 – Moving forwards and sideways to negotiate eight obstacles tied to the ceiling with nylon thread, arranged in two columns measuring 125cm×60cm.
Station 6 – Walking under two 80-cm-long obstacles located 130cm above the floor, using squatting movements.
Station 7 – Climbing stairs with seven 10-cm-high steps, angled at 45° and equipped with an 85-cm-high handrail, then going down a 3.10-m-long ramp. This procedure was then repeated.
Station 8 – Walking in a straight line over 3m of mats placed end-to-end on the floor.
Participants were instructed to complete the circuit at a fairly light intensity, corresponding to level 12 on the Borg Scale,23 which requires approximately 55% of maximum heart rate, ensuring continuity of the activity for the time period established.
They were also advised to use light clothing and no footwear, in order to avoid possible influences by different types of shoes.
On the first day, prior to the experiment, participants were familiarized with the circuit. They were also informed that they could interrupt the maneuver at any time if they felt discomfort. Furthermore, they were instructed not to alter their activities of daily living, in order to reduce possible external influences on the final results.
Statistical analysesWe used descriptive analysis with mean, standard deviation and delta percentage. Sample normality was assessed by the Shapiro–Wilk test. To analyze response variables, the paired Student's t or Wilcoxon test was used for intergroup analysis, when appropriate. The value of p<0.05 was adopted for statistical significance, and the SPSS version 19 program was used to assess results.
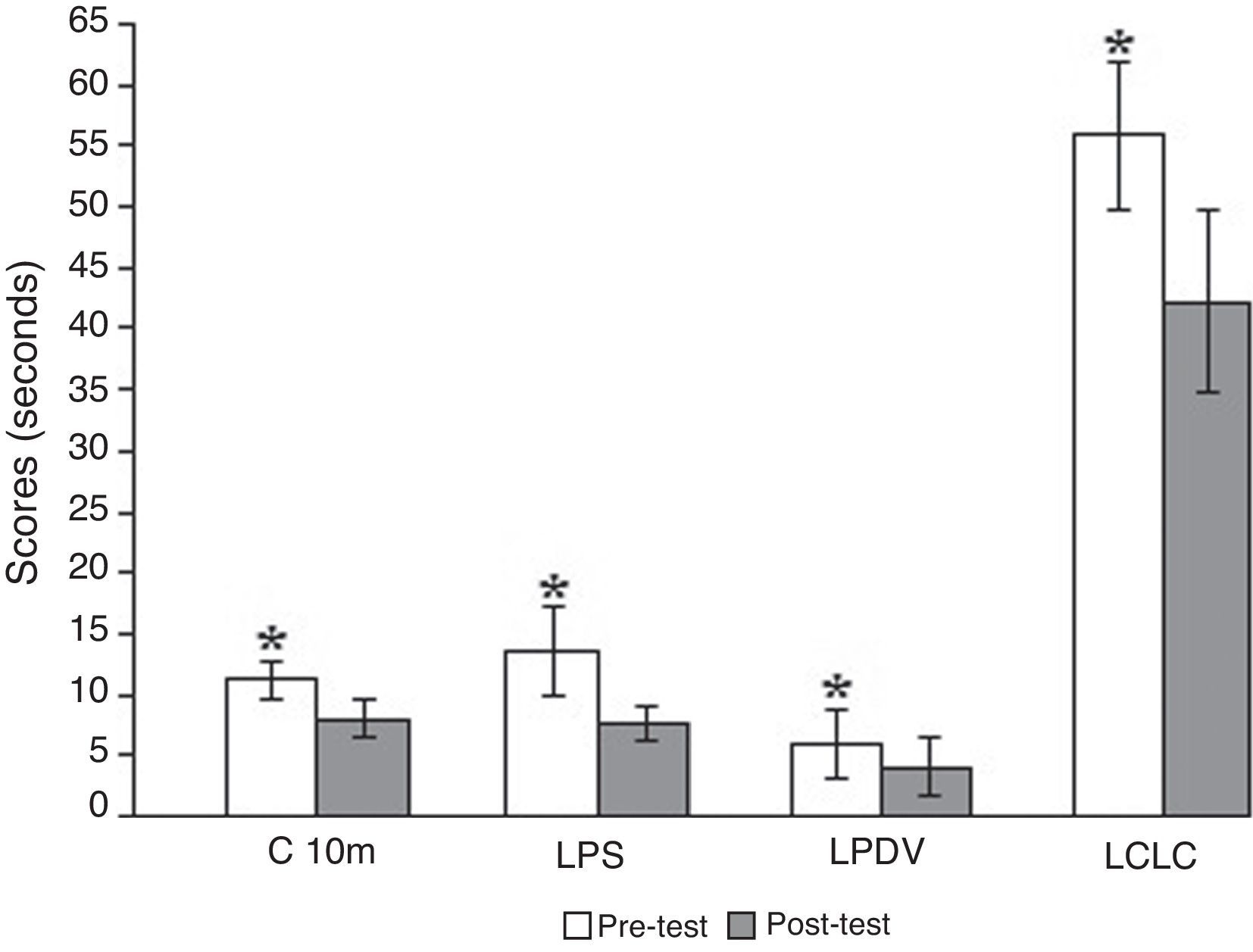
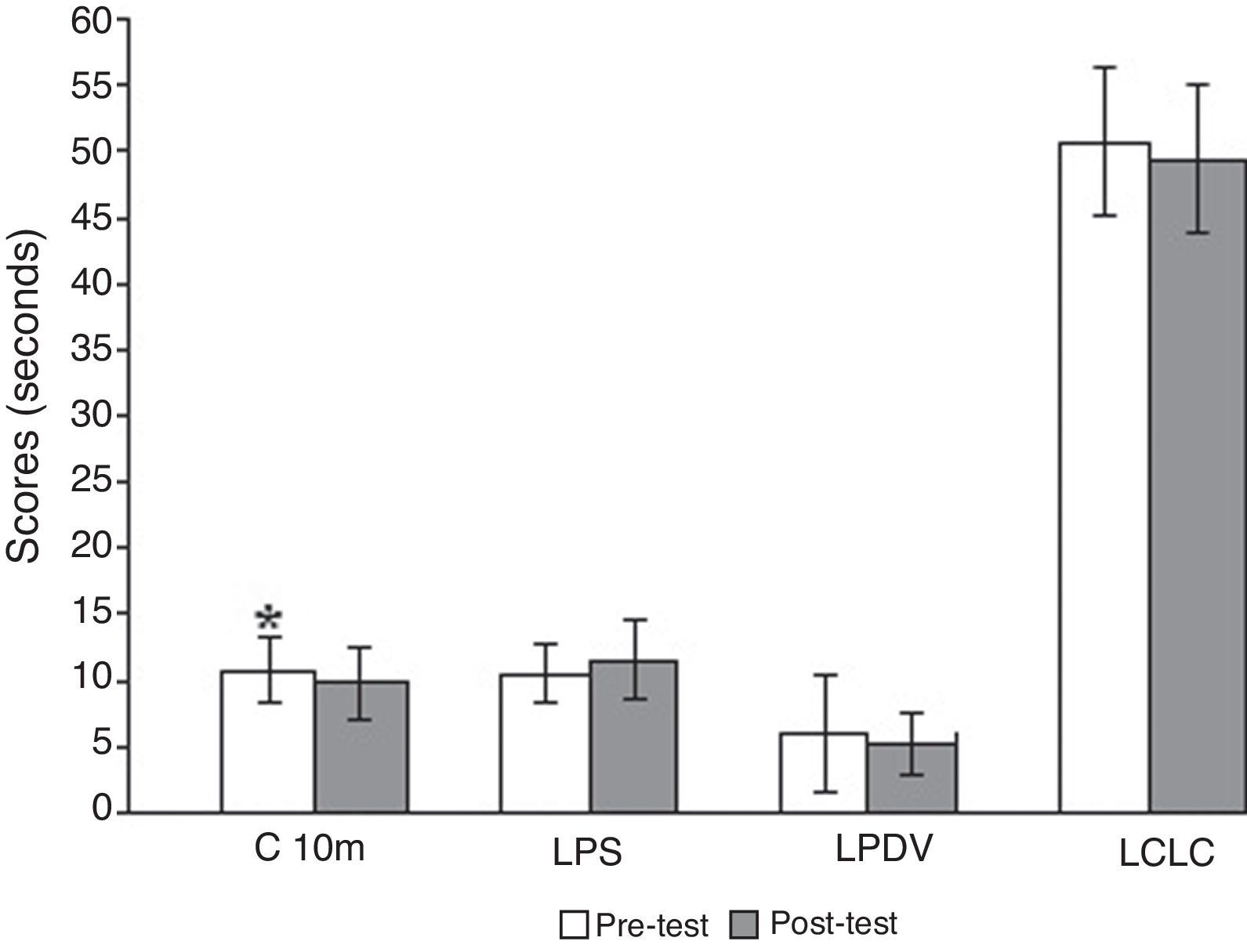
ResultsThe scores obtained by the control and experimental groups on the four tests and the GDLAM index, before and after the intervention, are illustrated in Graphs 1, 2 and 3.
The experimental group showed a significant reduction in execution time in all the tasks (Fig. 2), while the control group scored significantly higher only in the 10-M walk (Fig. 3).
With respect to the GDLAM index (Fig. 4), the experimental group decreased from 81.09 to 54.33 (p=0.0001), that it is still considered weak, that is >27.42. The control group increased from 34.75 to 35.49 (p=0.3016).
DiscussionThe low functional performance classification observed in the elderly of the present study is in accordance with the premise that aging, in conjunction with a sedentary lifestyle, provokes a reduction in functional capacity.24 According to a number of studies,25,26 the more active elderly preserve functional autonomy for a longer period of time, thereby reducing the risks of functional decline.
Similar data were observed in another study.24 The authors compared the autonomy level between 15 sedentary elderly individuals, that is, who did not engage in any type of regular physical activity and 15 others who walked at a light intensity pace three times a week for 30min, over a three-month period. The active elderly obtained better results (p<0.01), but when EG values were compared, both groups were classified as weak. In the C10m, LPS, LPDV and LCLC tests, the active elderly exhibited significantly better results (p<0.05) than the other group.12,27
As a strategy to preserve autonomy, physical exercises can be implemented to increase not only endurance and muscle strength, but also balance and mobility, which could reduce risks of falling and injuries28 and positively impact the performance of activities of daily living.29,30
Physical activity also improves functional capacity, that is, the ability to perform normal activities of daily living with efficiency and independence, and training focusing on functionality is the best means of developing this capacity. According to the principle of specificity, this form of exercise seeks to adapt the human body to normal activities of daily living, using exercises that stimulate proprioception and physical capacities such as strength, flexibility, motor coordination, balance and cardiovascular endurance.31,32
In order to promote successful learning, specific task-directed activities must be intensely performed, evolving to varied exercises and environments. In this training, several distinct strategies must be applied, since most balance demands derive from activities of daily living. For this reason, two aspects must be considered when selecting functional training activities: the patient's safety and level of control, as well as variety in terms of real-life functional tasks and environment.31
In the present study, pre- and post-training sensorimotor results in the EG demonstrate task learning, evidenced by the reduced execution time on the tests. Similar studies have shown that a physical activity program involving walking three times a week for 45min at an intensity between 55% and 75% of maximum heart rate,33 and another applying the same frequency with a duration of 60min, over a three-month period, produced shorter execution times on all GDLAM tests, reflecting in improved functional autonomy.34
An experimental study conducted in elderly women (65±6.40 years), separated randomly into an experimental – EG (n=31) and control group – CG (n=28), assessed aerobic endurance, autonomy and quality of life after recreational activities and 1h walks three times a week for four months. With respect to autonomy, the GDLAM index of the EG exhibited significant improvements when compared to the pre-test and post-test (p=0.0001), in contrast to the CG, where this did not occur (p=0.999).35
Other types of programs also aim at improving functional autonomy. This can be observed in a study of 52 sedentary elderly people, divided into a control (CG) and experimental (EG) group, submitted to a series of 10 Pilates exercises, twice a week for eight weeks. After the training program, it was found that the EG achieved significantly better results on all the tests and in the GDLAM index (p=0.035), and that the CG obtained a significantly higher score (p=0.042) only on the 10m walk test.36
Yoga has also been shown to improve autonomy when a group that engaged in this activity twice a week for 60min over a 14-week period, n=52 (66.79±3.30 years) was compared with a control group, n=31 (69.33±4.84 years), resulting in better GDLAM index (p=0.0001).37
Although sensorimotor training provoked significant improvements in task execution time, the GDLAM remained weak. This may be due to the fact that the subjects investigated were elderly and sedentary, in addition to insufficient training duration. Thus, new studies should be conducted with longer intervention periods and a younger age group than the one used in the present study.
In conclusion, the results show that engaging in sensorimotor training reduces the task execution, which is directly related to improved functional performance in activities of daily living.
Conflicts of interestThe authors declare that they have no conflicts of interest.