Introduction
Parkinson's disease (PD) is a progressive movement disorder that is accompanied by bradykinesia and may be diagnosed precisely.It is characterized by the occurrence of a severe nigral cell loss in the pars-compacta, and an accumulation of alpha-synuclein in the cerebral trunk, spinal medulla and cortical regions1.
The etiopathogenesis of PD is not known with certainty, although we know that genetic predisposition exists2,3, and that age is a risk factor, since the prevalence of PD increases with age, for example incidence increases by 0.3% each year for every 1,000 persons aged between of 55 and 65, and 4.4% each year for every 1,000 persons aged 85 and above. Apparently men have a greater risk of suffering from PD than do women (the ratio between affected men and women being 1.54; 95% IC, 0.95 to 2.51)4,5.
The main motor symptoms of PD are tremors, rigidity, bradykinesia, akinesia, and problems with balance and gait6,7. These symptoms have an effect upon the health-related quality of life (HRQoL)8 affecting physical, psychological, social and functional well-being9; presenting a lower level of physical activity10, bone mass11, strength12, skills and balance13 than in healthy peers14, whereby this population has a threefold greater risk of falls followed by fractures than do persons not suffering from this disease15,16.
PD is marked by a deficit of dopamine supply, so that the most common treatment therapy is based on the replacement of this neurotransmitter17,18. Although neuroprotective treatments have advanced greatly, we are still very far off from being able to control motor handicap, so that the addition of other therapies, such as regular physical activity, which may contribute to improving gait, postural asymmetries, balance and increasing muscular strength is highly necessary19.
Even though some physical therapeutic treatment recommendations20 exist for each of the stages that PD passes through21, initiatives for studying the cost-effectiveness and cost-utility of these therapies are rare indeed22. However, this type of studies does exist for pharmacologic therapies23, along with other types24.
In the last decade of the previous century, the use of whole body vibration (WBV) for improving performance and therapy had surged tremendously25. However, the beneficial effects of vibration in patients with nervous-system disorders had already been observed by neurologists, such as Martin Charcot26, at the beginning of this century, thus paving the way for studies related to the harmful effects of exposure to vibration in the workplace27.
Although, in recent years, the use of WBV has seen an increase in popularity, the mechanism responsible for the resulting benefits remains unclear. It is generally believed that WBV stimulates subcutaneous proprioceptors, the spinal circuit being the first phase in the feedback motor loop for generating rapid efferent reactions in response to proprioceptive input, thereby producing a tonic vibration reflex28, although central projection of the supraspinal motor centres also controls these reactions, thereby increasing corticospinal excitability and producing an alteration of the intracortical processes that are exclusively related to exercise29.
The majority of studies with healthy individuals has demonstrated WBV as a method for increasing physical capacity30, hormonal production31, bone mass32, balance, proprioception, and HRQoL33. However, a growing number of studies have been published for specific populations, for example adults, post-menopausal women, or persons with neurological disorders34-46. Along with the increasing number of studies on the effects of WBV, systematic reviews related to the treatment and training of healthy individuals47-49, specific populations50, and neurological pathologies have begun to emerge. However, we have no knowledge of any systematic reviews on the effects of WBV in PD.
The aim of the present systematic review is to evaluate, at the risk of bias, the volume and methodological quality of clinically relevant studies existing up until June 1, 2009, and examine the effects obtained by WBV in patients affected by PD.
Methods
In producing our systematic reviews, we used the PRISMA methodology51.
Applied resources
Studies were identified by searching the following electronic databases of recognized quality, scanning the lists of articles reported there: AMED (2005 to the present), The Cochrane Library (2003 to the present), GoogleSchoolar (2003 to the present), MEDLINE (2000 to the present), PEDro (2003 to the present), PubMed (1973 to the present), SPORTdiscus (2002 to the present), TRIP database (2002 to the present), and Web of Science (1988 to the present). The ISRCTN database was scanned beginning from January 1, 2008, and until July 1, 2009, for the purpose of locating future studies of relevance to the current topic and entered there.
Article selection
Selection of the databases, search strategy and list of terms, including their combinations, was done by medical library science experts and experts in the field of WBV applied to PD in order to locate the articles reported in the present systematic review. The search was completed July 1, 2009, with no submission deadline imposed on the experts.
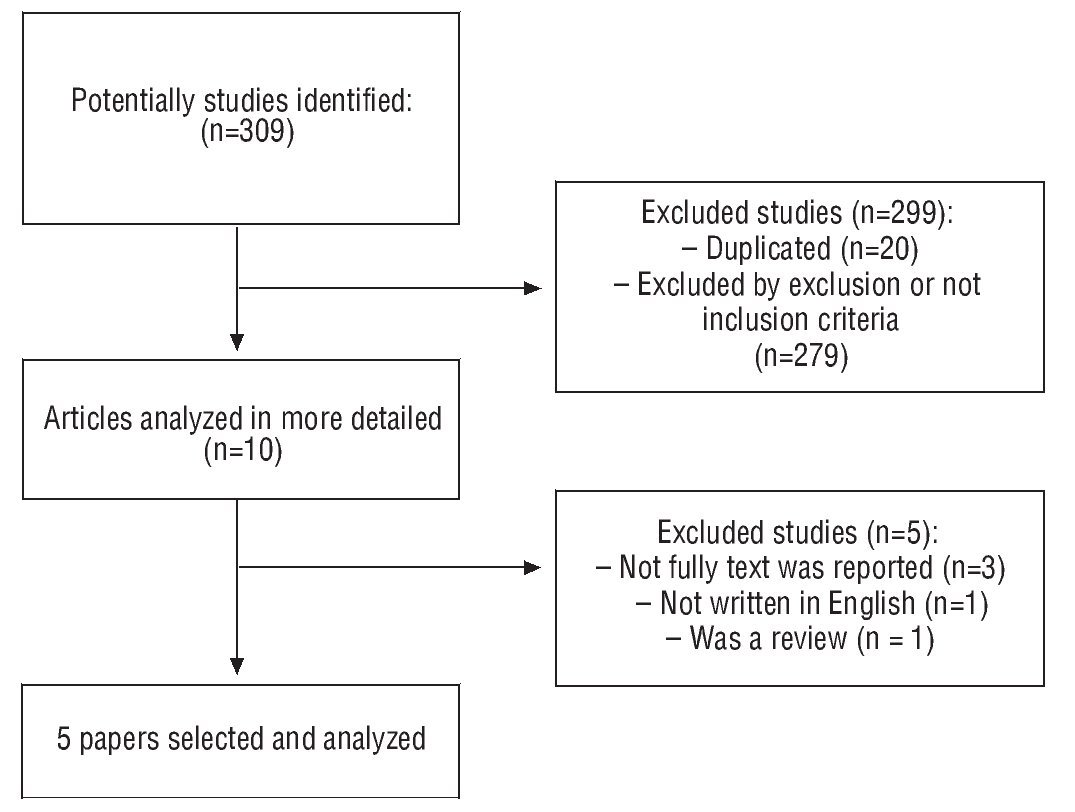
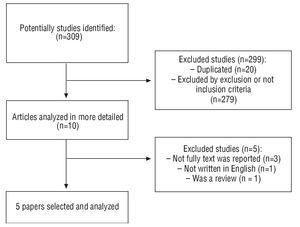
The articles were located by using a combination of terms, ranging from WBV training or therapy to PD, accurately using the Boolean operators (AND, OR, NOT) in order to scan all underlying articles of relevance to the topic. A detailed list of terms and combination formulas is available from the authors of the present study. Duplicate articles were manually removed by one of the authors taking part in the initial review process. In figure 1, the flow chart of the complete process for the system review appears. Articles of the present study were indexed, if they matched the following inclusion criteria: a) treatment or training with WBV, b) aimed at individuals with PD, c) randomized and non-randomized clinical studies, d) studies with and without a control group in order to compare the effects of the treatment or training, e) published exclusively in English, and f) original articles of clinical studies. Articles were excluded, if they matched the following criteria: a) effects of exposure to vibration if studied within industry, labour employment and transport, b) aimed at animals and persons not presenting PD, c) one-time presentation of a summary at a conference, congress, critical treatise or seminar, d) presented in a language other than English, and e) reviews. Article selection was done by two experts independent of the standard method (with no double-blind controls), and resolving potential disagreements through mutual consensus. However, if this was impossible, direct contact with the original author of a certain manuscript was obtained via e-mail or telephone, as appropriate.
Fig. 1. Flow diagram of systematic review process.
Risk of bias
In order to assess the risk of bias in the studies that were included in the current systematic review, we used the Physiotherapy Evidence Database (PEDro) scale. We chose this scale due to its special design and ability to provide a global view of the external and internal validity of the studies included in the present systematic review, and after reviewing its repeatability and utility52. Each article was graded independently by two reviewers participating in the study, reporting a high degree of intra-class coefficient correlation (0.92). There were no significant disagreements among the advisors (p = 0.9).
Level of evidence
The level of evidence was reported in accordance with the guidelines of the German Institute for Healthcare Improvement (CBO)53.
Data extraction process and the outcome measurements used in this review. Analysis
The extraction of data from the selected articles was done by one author of the present review and subsequently checked by another, discussing potential disagreements among them, and finally allowing a third author to resolve any disagreements, when the original author of the manuscript submitted for discussion could not be contacted. The information was extracted separately from each selected manuscript, stating: a) participant characteristics (age and gender), b) degree of severity, duration and pharmacological patient dose, c) type of intervention (including type of machine, oscillation, frequency, amplitude, duration of intervention, series number and intervening rest periods, exposure time per series, body posture, knee angle and number of WBV sessions). An identical procedure followed in order to assess the key measurements contained in the individual reviewed articles and finally included in the present study. The key measurements presented were: a) balance, b) gait, c) postural control, d) proprioception, and e) HRQoL; using various measurements for the same physical quality in accordance with the article. These measurements were evaluated on the basis of the effect produced by WBV reported by the original author, and determined according to: a) ↑ improvement in the exercise group (p < .05), b) ↓ improvement in the control group (p < .05), c) = absence of significant differences, d) * unreported or non-existent data, and e) Δ significant intra-group, pre- and post-test differences.
Results
Article selection
Figure 1 shows the complete process that was followed in the systematic review. An electronic search of AMED (4), the Cochrane Library (11), GoogleSchoolar (281), MEDLINE (5), PEDro (1), PubMed (5), SPORTdiscus (3), TRIP database (0), Web of Science (10), and ISRCTN (0) yielded a total of 309 citations. A number of 289 citations were reviewed after removing duplicates. Of these, a total of 279 publications were rejected for inclusion in the systematic review, since having reviewed their summaries, they evidently did not match the proposed inclusion criteria. Five studies were subjected to a more in-depth analysis, since it was not clear from their summaries, whether or not they matched the inclusion criteria, and they were subsequently eliminated due to the following reasons: Full text not provided (n = 3), written in a language other than English (n = 1), and dealt with systematic reviews (n = 1). A total of 5 articles were identified for inclusion in the current systematic review.
Risk of bias
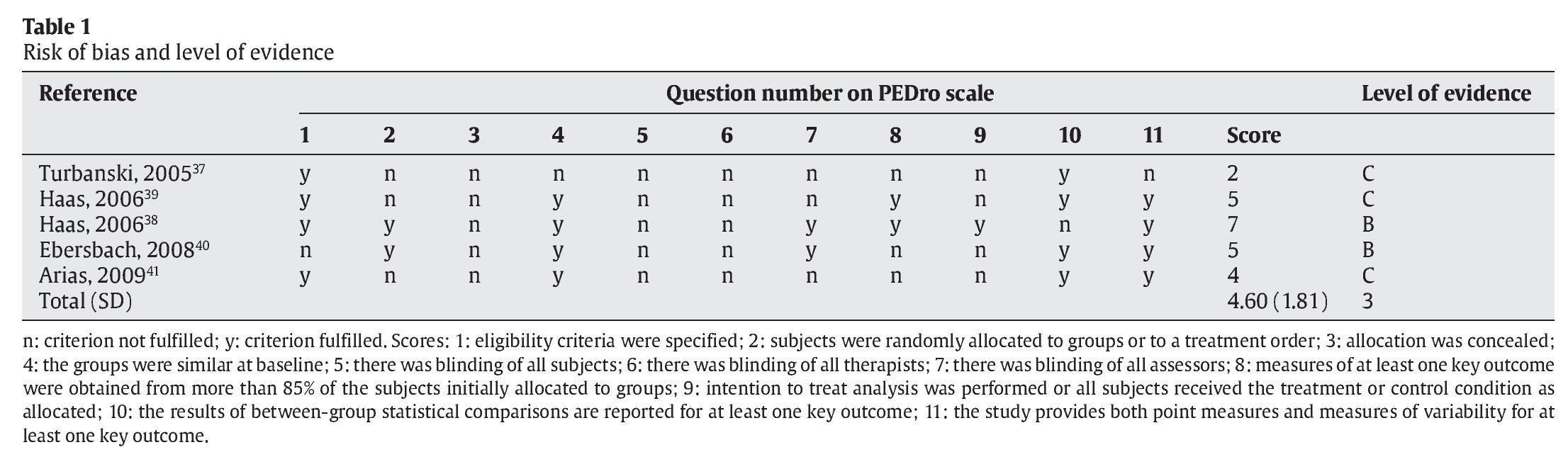
Table 1 provides the scores of each reviewed study, in which 3 studies were randomized and 2 were not. The scores on the PEDro scale varied between 2 and 7, the average being 4.60, and the standard deviation ±1.81. The lowest scores were given to items referring to the ignorance as to which group each patient corresponded to (assessors and therapists), where this was referenced by only two studies, and ignorance (by a patient) as to which group he/she belonged to, where no study made reference to assignment ignorance. On the other hand, an «intent-to-treat» analysis was not provided by any study. In the statistical field, 2 studies provided detailed measurements along with their variability, while 2 thereof made no reference to these measurements. Four of the reviewed studies provide inter-group comparisons, whereas only one study does not. All the studies provide participant characteristics, along with the inclusion and exclusion criteria defined by each study.
Level of evidence
Table 1 shows the level of evidence for each study. Two studies present a level of evidence B, and three studies present a level of evidence C. The level of evidence of the topic discussed in the review was 3, in conformance with CBO53.
Study characteristics
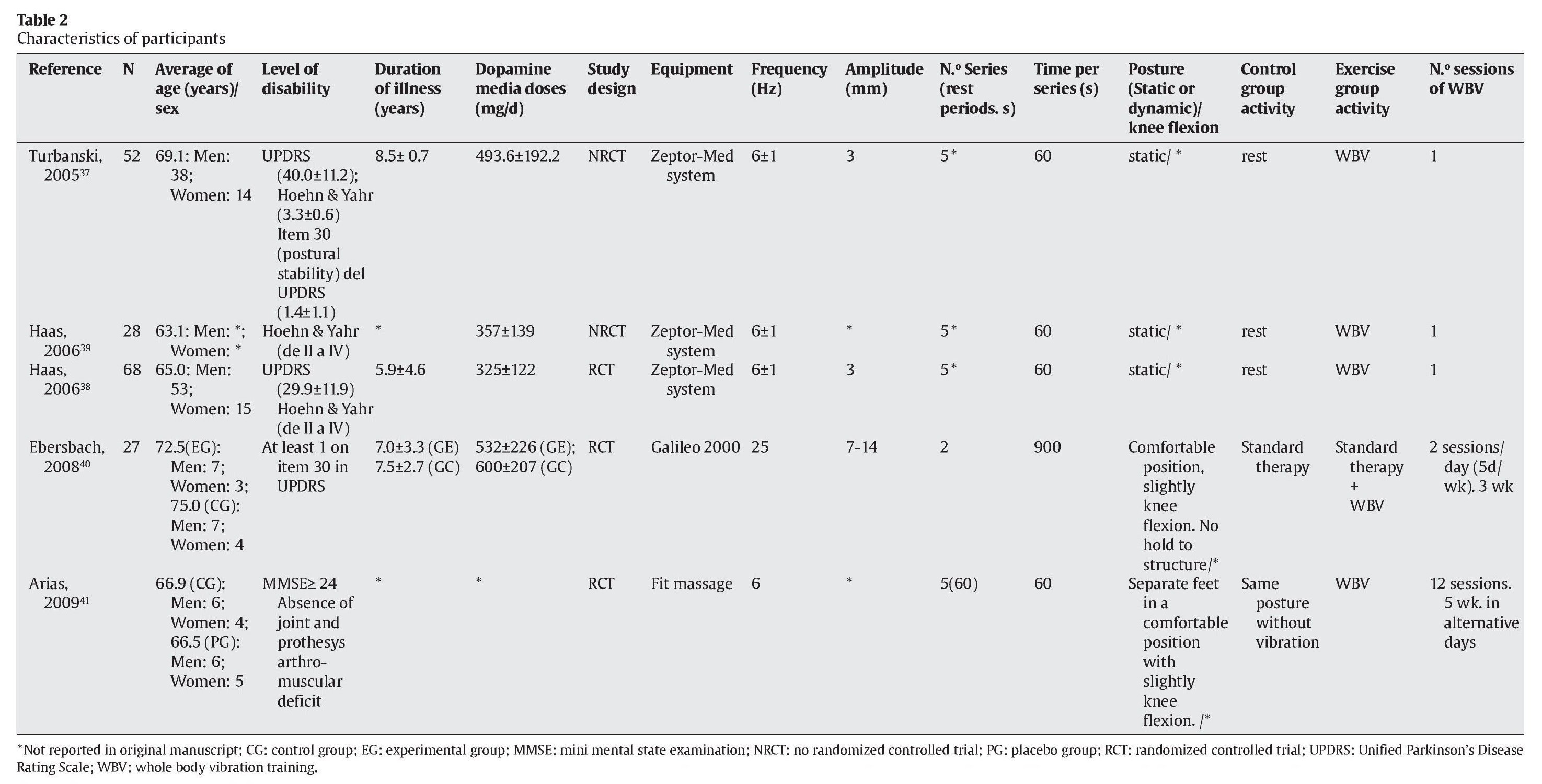
Table 2 captures the characteristics of the articles reviewed according to the theoretical approach reported internationally in health care, PICOS (Participants, Intervention, Control, Outcome Measurements and Study design)54.
Patients
The age of reviewed study participants varied between 63.1 ± 7.3 and 75.0 ± 6.8. Most of the patients presented in the studies were of male gender (above 50% in each reviewed study). The minimum sample contained 27 patients, and the maximum 68. The degree of severity varied from II to IV according to the Hoehn & Yahr (H&Y) scale21. The dopamine dose varied from 325 (± 122) to 600 (± 207.0) mg/d. The duration of the disease varied from 5.9 ± 4.6 to 8.5 ± 0.7 years.
Whole body vibration equipment
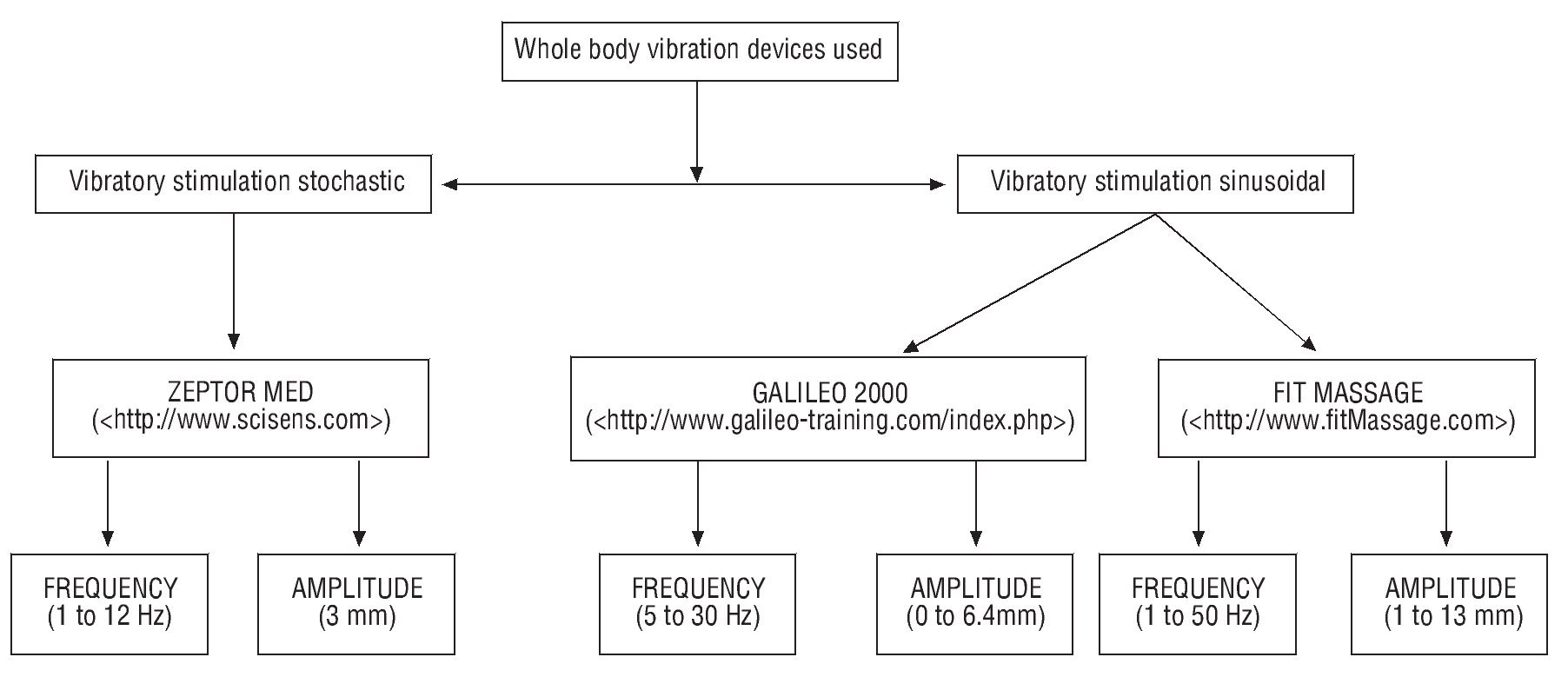
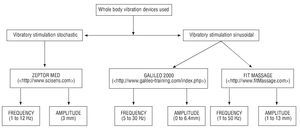
The following vibration platforms were used in the review studies; 3 studies37-39 used ZEPTOR-med (Scisen GmbH, Germany), study 40 used Galileo 2000 (Novotec, Germany) and 1 study used Fit Massage 21641 (Top elite fit massage. Co, Zhejiang, China), differing from one another in terms of the type of vibration stimulation; the studies of one single WBV session used vibration platforms of the stochastic type, whereas the studies of at least 12 intervention sessions used tilting vibration platforms (fig. 2).
Fig. 2. Whole body vibration devices.
Parameters affecting whole body vibration
Frequency (Hz) and amplitude (mm)
The frequency applied in the stochastic vibration machines was 6 Hz and the amplitude 3 mm37-39, whereas the tilting vibration machines used 6 and 25 Hz with an amplitude varying between 7 and 4 mm40,41.
Knee position and degree of knee flexion
All the reviewed studies reported static position during WBV, while no study detailed the exact degree of knee flexion.
Description of training
WBV training varied between studies, where a single session was used in order to determine the acute effects and studies, where 12 or more WBV sessions were used in order to observe chronic effects. Three studies analyzed the acute effects of WBV37-39, after a single session of 60 s, while 2 studies analyzed the chronic effects after 12 and 30 sessions, respectively, lasting from 60 to 900 s (with a 60-s resting period between series)40,41.
Key measurements and effects
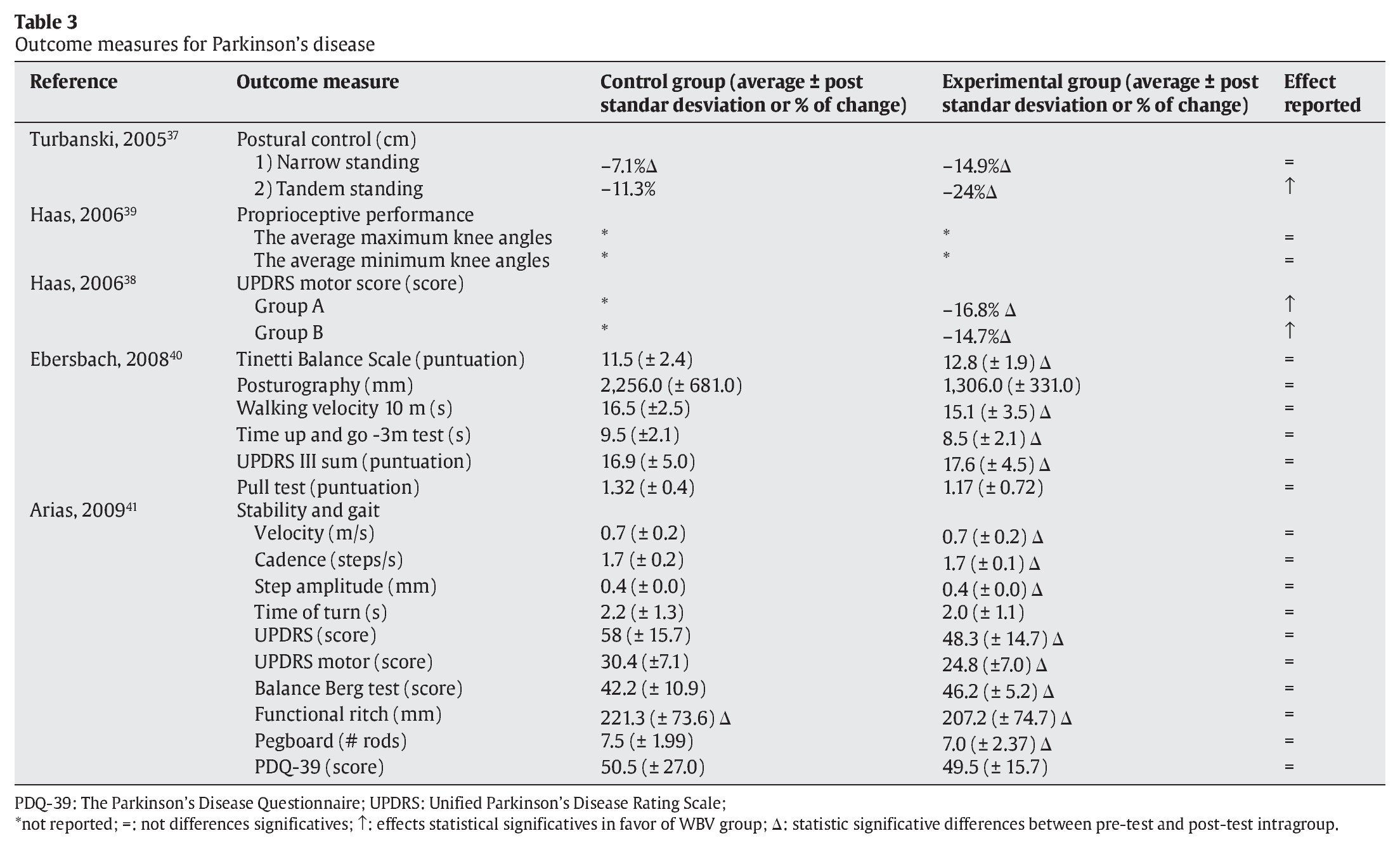
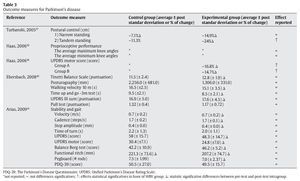
The key measurements refer mainly to HRQoL and postural control values (table 3).
HRQoL
Five articles evaluated the impact of WBV on HRQoL using special questionnaires for each population. The Unified Parkinson's Disease
Ratings Scale (UPDRS)40,41 and the Parkinson's Disease Questionnaire (PDQ-39) were used41.
Postural control
Four studies captured measures related to postural control, balance or gait37,38,40,41. In order to evaluate balance, proprioception and gait, we used measurements such as the functional reach test41, a test of walking 10 m at maximum speed40, the Berg41 and Tinetti40 balance scale, a test of rising, walking and sitting down40 and specific gait parameters, such as speed, cadence, stride length and turning41.
Effects of exposure to whole body vibration
Three37-39 out of the 5 studies reviewed focus on the acute effects of undergoing a single vibration session, and particularly evaluating the effects of postural control37, proprioception39 and PD motor symptoms38 noting improvements in the measurements of postural control with an advanced foot, in tremor, rigidity, bradykinesia, gait and posture. As for chronic effects, two articles studied the effects of medium-term exposure (after 12 and 30 sessions) to WBV40,41, one of them in comparison with a standard therapy40 and the other, comparing with a placebo group41, finding no improvements in any of the measured parameters, except for posturography.
Discussion
The completed systematic review produced a limited number of studies related to the effects on PD obtained by WBV, this being still a very recent topic (the first completed study dates back to 2005), and a great variety in the PICOS approach in the reviewed studies, something which makes it difficult to conduct a meta-analysis. For all the above reasons, the scientific evidence on the subject is limited, yielding a level 3 conformance with CBO53.
The results of the reviewed studies show that after a single WBV session, or after several weeks of training, the final HRQoL score improves in the UPDRS questionnaire, as does the score in the section of the questionnaire dealing with physical parameters. However, this improvement is reminiscent of the one obtained in a placebo group or a group in which a standard physical therapy was continued40,41. The paucity of studies and the modest sample size, allow us to say that there is currently scant evidence concerning the effects of WBV on HRQoL in PD.
In contrast, nearly all the reviewed studies present measurements related to balance, gait and postural control, which are crucial conditions in the course of PD7. The effects of applying a single WBV session on the above parameters remain limited, since only one study reported improvements in terms of postural control37. As for the effects of WBV training below 12 weeks, it was observed that this type of training fails to produce a major improvement in patients, when comparing with a placebo therapy or a standard physical therapy, however, the statistically significant improvements found in the WBV group vis-a-vis the baseline is a sign that this treatment may be useful in PD.
This review presents some limitations. It lacks a standardized criterion for evaluating the level of evidence. Different authors of systematic reviews use different criteria55, and besides, the one and the same author sometimes uses different criteria depending on the study56. The use of different criteria is related to the decision as to whether randomized clinical studies or studies presenting a low methodological quality should be considered, whereby scales of measurement may also vary, and the best method for assessing the risk of bias is also uncertain55.
Data deemed important, but found missing in the original manuscript, had to be requested from the author in charge of correspondence and omitted if not reported.
The search strategy that was used involved the risk of bias, since only articles written in English were searched. Publishing significant rather than non-significant results is easier, and the latter are more likely to appear in national journals, if written in the native language57.
The need to investigate whether all the beneficial effects related to the application of WBV in healthy populations can be extrapolated to PD becomes apparent.
An optimal dose-response study according to disorder and WBV type is urgently needed. Similarly, the cost-effectiveness and cost-utility of various WBV treatments should be determined.
Conclusions
From data disclosed in the present review it appears that WBV may help improve balance, gait, postural control, as well as HRQoL of individuals with PD, however, the paucity of studies, the variety of applied vibration types, measurements provided in the various studies, and interventions performed have all made it difficult to make a comparison between existing PD and WBV studies. In order to clarify these issues, future studies need to be made.
Acknowledgements
This proyect was supported by Enterprising Solutions for Health, S.L.
Correspondence:
B. del Pozo Cruz.
Faculty of Sports Sciences. University of Extremadura. 10071 Caceres, Spain
E-mail:borjadelpozo@unex.es
History of the article:
Received August 14, 2010.
Accepted December 5, 2010.