Multidrug-resistant Shigella sonnei ST152, global lineage III, is a high-risk clone, whose dissemination has limited therapeutic options for shigellosis. This study aimed to characterize two isolates of S. sonnei, which were recovered in Lima, Peru, during November 2019, exhibiting resistance to extended-spectrum cephalosporins and quinolones, and concurrently harboring blaCTX-M-15 and qnrS1 genes, in addition to mutations in gyrA-S83L. These isolates were resistant to ceftriaxone, ciprofloxacin and trimethoprim/sulfamethoxazole. The molecular analysis showed that both isolates belonged to lineage III, sublineages IIIa and IIIb. The blaCTX-M-15 gene was located in the same genetic platform as qnrS1, flanked upstream by ISKpn19, on a conjugative plasmid belonging to the IncI-γ group. To the best of our knowledge, this would be the first report on S. sonnei isolates carrying the blaCTX-M-15 gene in Peru. The global dissemination of S. sonnei ST152, co-resistant to β-lactams and quinolones, could lead to a worrisome scenario in the event of potential acquisition of genetic resistance mechanisms to azithromycin.
La bacteria multidrogorresistente Shigella sonnei ST152, del linaje global III, es un clon de alto riesgo, cuya diseminación ha limitado las opciones terapéuticas contra la shigellosis. En este estudio se caracterizaron dos aislamientos de S. sonnei resistentes a cefalosporinas de espectro extendido y a quinolonas, recuperados durante noviembre de 2019 en Lima, Perú. Ambos aislamientos albergaban simultáneamente blaCTX-M-15 y qnrS1, además de mutaciones en gyrA S83L. Estos aislamientos fueron resistentes a ceftriaxona, ciprofloxacina y trimetoprima/sulfametoxazol. El análisis molecular mostró que ambos aislamientos pertenecían al linaje III, sublinajes IIIa y IIIb; blaCTX-M-15 se encontró ubicado en la misma plataforma genética que qnrS1, rodeado aguas arriba por ISKpn19, en un plásmido conjugativo perteneciente al grupo IncI-γ. En nuestro conocimiento, esta es la primera comunicación de S. sonnei productora de blaCTX-M-15 en Perú. La propagación global de S. sonnei ST152 corresistente a β-lactámicos y quinolonas podría conducir a un escenario preocupante, llegado el caso de la adquisición de mecanismos genéticos de resistencia a azitromicina.
Shigellosis is a bacillary dysenteric disease that is responsible for approximately 1.1 million deaths annually, mainly involving children under 5 years old4. Shigella comprises four related species (S. flexneri, S. boydii, S. dysenteriae and S. sonnei), exhibiting a heterogenous geographic distribution. Shigella flexneri traditionally exhibits a predominant prevalence in low and middle income countries7. However, in the last decade, an abnormal increase in S. sonnei incidence has been observed globally4, including in Peru. Despite shigellosis being a self-limited disease, antimicrobial therapy is recommended in patients with severe or invasive infections and in cases associated with malnutrition and prolonged dysenteries7. Furthermore, the World Health Organization (WHO) has proposed antimicrobial use in asymptomatic carriers as an approach for limiting its dissemination15. However, the increase in Shigella antimicrobial resistance has modified the therapeutic alternatives for first- and second-line drugs. Since 2005, given the high levels of resistance against trimethoprim–sulfamethoxazole, tetracycline, chloramphenicol, ampicillin, and nalidixic acid, the WHO has suggested the use of ciprofloxacin and ceftriaxone, as first-line agents, and azithromycin as a second option15. Nevertheless, the global dissemination of S. sonnei sequence type (ST) 152, known for its antimicrobial resistance profile to extended-spectrum cephalosporins (ESC), macrolides and quinolones, drastically limits the therapeutic options and has raised a global alert4.
At the beginning of 2022, the United Kingdom reported a three-fold increase in S. sonnei isolates displaying resistance to ESC, quinolones, tetracycline, azithromycin and sulfamethoxazole3. A similar scenario has been reported in several countries of the European Union and Southeast Asia4. In Latin America, the Pan American Health Organization (PAHO) recently issued an alert, highlighting the need to strengthen the epidemiological surveillance of S. sonnei9. The aim of this study was to report the genetic features of two S. sonnei clinical isolates coharboring blaCTX-M-15 and qnrS1 that belong to an internationally successful clone.
Two isolates of Shigella sonnei resistant to ESC (SS1 and SS2) were isolated from stool samples of a 2-year-old male and a 37-year-old female in November 2019, at the “Clínica Centenario Peruano – Japonesa” in Lima, Peru, respectively. Susceptibility tests to ampicillin/sulbactam (AMS), ceftazidime (CAZ), ceftriaxone (CRO), cefepime (FEP), ertapenem (ETP), meropenem (MER), amikacin (AMI), gentamicin (GEN), ciprofloxacin (CIP) and trimethoprim/sulfamethoxazole (TMS) were performed using automated systems (VITEK® 2 COMPACT, Biomeriux). Azytromicin (AZT) resistance and extended-spectrum β-lactamase (ESBL) production were determined by the disk diffusion method. Interpretation was performed by following the recommendations outlined in CLSI M100-ED33 2023 (https://clsi.org/all-free-resources/).
Bacterial DNA was extracted using the GeneJetGenomic DNA Purification kit (ThermoScientific), following the manufacturer's recommendations. The presence of the blaCTX-M gene was performed by polymerase chain reaction (PCR) amplification. In addition, the identification of blaCTX-M-1, blaCTX-M-2, blaCTX-M-9 groups was conducted by PCR using specific primers: Fw-blaCTX-M-1 (5′-ATGGTTAAAAAATCACTGC-3′), Rv-blaCTX-M-1 (5′-GGTGACGATTTTAGCCGC-3′); Fw-blaCTX-M-2 (5′-CGTTAACGGCACGATGAC-3′), Rv-blaCTX-M2 (5′-CGATATCGTTGGTGGTGCCAT-3′); Fw-blaCTX-M-9 (5′-GATTGACCGTATTGGGAGTTT-3′), Rv-blaCTX-M-9 (5′-CGGCTGGGTAAAATAGGTCA-3′). Plasmid conjugation assays were performed by a mating-out assay using Escherichia coli J53 sodium azide resistant (Azr) as the recipient strain (ECJ53) and SS1 and SS2 as donor strains. Isolates were grown overnight in 5.0ml of Luria Bertani (LB) broth and incubated until an optical density of 0.6 was reached. Subsequently, in each case, equal parts (0.5ml) of the cultures were mixed, centrifuged, and the pellet was resuspended in 100μl of LB broth. Transconjugants were initially selected on LB agar containing ampicillin (50μg/ml) and sodium azide (150μg/ml). Grown colonies were subcultured in LB agar supplemented with cefotaxime (2μg/ml) and sodium azide (150μg/ml). Transconjugants (TCSS1 and TCSS2) were evaluated by analyzing the blaCTX-M group and the antibiotic susceptibility profile as mentioned.
Next generation sequencing (NGS) analysis was performed on both strains. Genomic libraries were prepared using the MiSeq chemistry, Illumina, with paired-end 2×250bp. Poor quality readings (Phred scores below 30) were filtered out using the Trimmomatic v0.39 program. De novo genome assembly was conducted using Unicycler v0.4.8. Assembled final sequence genomes were annotated using Prokka v1.14.6 and manually curated. Sequence type (ST) was identified with MLSTfinder v2.0, resistance genes with ResFinder v.1 and plasmid incompatibility groups with PlamidFinders v2.1 software. Genetic relationship based on single-nucleotide polymorphisms (SNPs) was assessed using genomic sequences of S. sonnei ST152 available on the GenBank public database. SNPs were identified and extracted using SNP-sites v.2.5.1 and maximum-likelihood clustering was inferred by IQ-TREE Phylogenomic v.1.5.5.3 using the best-fit model found and 1000 bootstraps. The complete, raw sequences were deposited in NCBI under BioProject ID: PRJNA968049.
Both S. sonnei bacterial isolates, designated as SS1 and SS2, respectively, exhibited a multidrug-resistant (MDR) profile against AMS, CRO, TMS, and CIP, remaining susceptible to CAZ, FEP, ETP, MER, IMP, GEN, AMI and AZT (Table 1).
Antibiotic susceptibility profiles of Shigella sonnei strains and their transconjugants.
| Isolates | Minimum inhibitory concentration (μg/ml)c | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| AMS | CAZ | CRO | FEP | ETP | MER | AMI | GEN | CIP | TMS | |
| SS1 | 8S | 2S | ≥64R | 0.5S | ≤0.12S | ≤0.25S | ≤1S | ≤1S | ≥4R | ≥320R |
| TCSS1a | 8S | 2S | 32R | 0.5S | ≤0.12S | ≤0.25S | ≤1S | ≤1S | 0.5I | ≥320R |
| SS2 | 8S | 2S | ≥64R | 0.5S | ≤0.12S | ≤0.25S | ≤1S | ≤1S | ≥4R | ≥320R |
| TCSS2b | 8S | 2S | 32R | 0.5S | ≤0.12S | ≤0.25S | ≤1S | ≤1S | 0.5I | ≥320R |
| EJ53 | ≤2 | ≤0.12 | ≤0.25 | ≤0.12 | ≤0.12 | ≤0.25 | ≤1 | ≤1 | ≤0.06 | ≤20 |
AMS: ampicillin/sulbactam; CAZ: ceftazidime; CRO: ceftriaxone; FEP: cefepime; ETP: ertapenem; MER: meropenem; AMI: amikacin; GEN: gentamicin; CIP: ciprofloxacin; TMS: trimethoprim/sulfamethoxazole; R: resistant; S: susceptible; I: intermediate.
PCRs for blaCTX-M and blaCTX-M-group-1 rendered positive results. The conjugation assay indicated that the blaCTX-M-group-1 gene was located on a conjugative plasmid that could be successfully transferred into E. coli J53. Two transconjugant strains were obtained (TCSS1 and TCSS2). Transconjugants showed resistance to β-lactams and TMS and exhibited reduced susceptibility to CIP (Table 1).
The whole genome of SS1 strain was composed of a 4554387 bp chromosome defined in 367 contigs, while the SS2 genome consisted of 4557581 bp, included in 369 contigs. NGS analysis confirmed that both isolates belonged to ST152. Replicons belonging to different incompatibility groups, such as IncFIB, Col156, ColRNAI, Col (BS512) and IncI-γ, were identified. In addition to the determinants of resistance to ESC (blaCTX-M-15), a plethora of genes, associated with resistance to phenicols [mdf(A)], tetracycline [tet(A)], aminoglycosides [aph (6)-Id, aph (3″)-Ib and ant(3″)-Ia], sulfonamide (sul2), quinolones (qnrS1) and trimethoprim (dfrA1) were also identified. Mutations in GyrA S83I related to fluoroquinolone resistance were detected as well.
The blaCTX-M-15 and qnrS1 genes were located in the same contig in both genomes. In SS1, they were identified in the same contig belonging to IncI-γ replicon. Additionally, the tet(A), aph(6)-Id, aph(3”)-Ib and sul2 genes were located in the same contig associated with the ColRNAI incompatibility group in both genomes. When analyzing the blaCTX-M-15 genetic context in SS1 and SS2, both genomes exhibited the same genetic platform, accompanied by the sequences: blaCTX-M-15 –cupin Wbuc-Tn3Δ-IS3Δ-qnrS1-hin-ISKpn19.
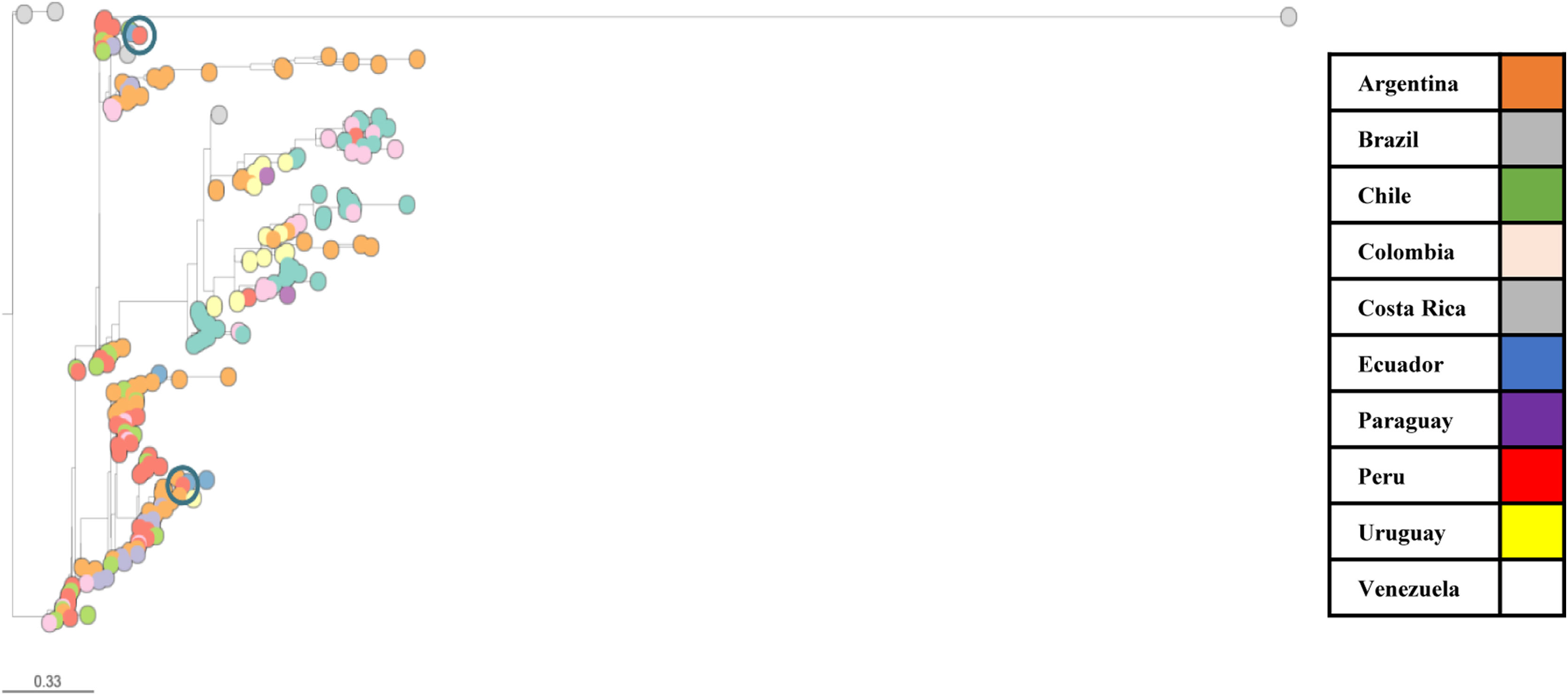
Phylogenetic analysis using a representative group composed of 230 genomes of S. sonnei from PulseNet Latin America and Caribbean surveillance network1, indicated that SS1 was closely related to ERR200468, isolated in Argentina in 2005, with 374 SNPs differences, while SS2 was related with SRR7693709, isolated in Ecuador in 2014, with 261 SNPs differences (Fig. 1). Additionally, a further analysis indicates that SS1 and SS2 correspond to IIIb and IIIa sublineages, respectively.
S. sonnei phylogenetic analysis using 232 genomes belonging to PulseNet Latin America and Caribbean Network. Analysis of the core-genome phylogeny of 232 S. sonnei isolates, including SS1 and SS2. Colors indicate the country of origin for each strain. The assembled WGS of the strains are presented in a core-genome SNV tree. The scale bar (0.33) represents the average number of nucleotide substitutions per site. The core genome represents the maximum total coverage (81.8%) of the alignment among all 232 S. sonnei conserved sequences, corresponding to 3985 SNVs. Framed in a blue circle: SS1 and SS2.
The high level of antimicrobial resistance in S. sonnei, attributed to the dissemination of ST152, global III lineage, has narrowed the antimicrobial options against shigellosis13 and has alerted about the need to strengthen epidemiological surveillance systems. Nowadays, there are several reports of S. sonnei ESBL producers, primarily related to CTX-M-15 and CTX-M-3, mainly10. To the best of our knowledge, although ESBL-producing S. flexneri isolates have been previously described in Peru by Gonzales et al.5, this study would be the first documentation of S. sonnei isolates harboring the blaCTX-M-15 gene in Peru. The ESBL gene was detected on a conjugative plasmid, conveying antimicrobial resistance capacity to β-lactams, TMS and reduced susceptibility to CIP.
As mentioned above in SS1, blaCTX-M-15 was identified in the IncI-γ group-contig (contig 3: 84778 bp). In S. sonnei, blaCTX-M-15 has been associated with several incompatibility groups (IncFII, IncZ), with IncI being relevant for its successful dissemination since 20066. Contig 3 in SS1 exhibited an identity of 99.2% with the plasmid p202102843-3 (GenBank: OP038292.1), recently reported in France in 20228. The genetic environment of blaCTX-M-15 is similar to that described in a IncFII plasmid from S. sonnei in 2020 (GenBank: CP045525)2 and in an IncFII plasmid from K. pneumoniae isolated in China in 2014 (GenBank: CP026158)11. The genetic context of blaCTX-M-15 described in the present study suggests the risk of dissemination of this genetic platform in different types of plasmids.
The global dissemination of ciprofloxacin-resistant S. sonnei, evolved from the sequential accumulation of mutations in gyrA-S83L, parC-S80I and gyrA-D87G, from Central Asia14. The former isolates reported only the gyrA-S83L mutation, accompanied by the qnrS1 gene, harbored in the same genetic environment as blaCTX-M-15. A Latin American surveillance study with 22273 S. sonnei collected over 15 years revealed that Peru was one of the countries in the region with the highest annual increase in resistance to ciprofloxacin (1–5%)12. Fortunately, the regional levels of resistance are still as low as 2.7% (9/329)1. Nevertheless, in several European and Asian countries, such as France or India, ciprofloxacin resistance has reached levels of up to 38.7% and 61.5%, respectively8.
The isolates SS1 and SS2, belonging to the global III lineage, were recognized for their role in the global dissemination of multidrug-resistant S. sonnei clones. We highlight their belonging to sublineage IIIb, described for the very first time in Peru1. These results support the evidence of clonal expansion of sublineages IIIa and IIIb in Latin America, as postulated by Baker et al.1
However, the low number of isolates and the lack of clinical information limit the scope of this study. Nevertheless, this research contributes to the characterization of the circulating strains of S. sonnei in our environment. Both isolates presented blaCTX-M-15 associated with qnrS1, presumably on a conjugative plasmid of the IncI-γ group; in both cases azithromycin susceptibility was observed. The global spread of strains with a profile of extreme resistance to antimicrobials makes it necessary to strengthen epidemiological surveillance systems.
FundingThis work was supported by the Faculty of Medicine of the University of Piura (PI2204).
Conflict of interestThe authors declare that they have no conflicts of interest.
To the company “SIMED Perú” for the donation of the bacterial susceptibility profile and identification kit, to Franco Romani of the Research Unit of the Faculty of Human Medicine, for the critical review of the manuscript, Agustina Costa of the University of Buenos Aires, Faculty of Pharmacy and Biochemistry (IBaViM), and Brenda Moy for the technical support in the laboratory.