The current decline observed in mortality rate among patients with ST-segment elevation acute myocardial infarction can be attributed not only to the increased use of reperfusion strategies, but also to a change in the demographic profile of this population, notably the reduction in mean age.
MethodsWe retrospectively reviewed all patients undergoing primary percutaneous coronary intervention in the period from April 2010 to December 2014. The primary objective was the characterization of the most prevalent risk factors, the angiographic nature of the lesions, the technical aspects of the procedure, and in-hospital clinical outcomes in patients aged ≤ 45 years, comparing them to those aged > 45 years.
ResultsAmong 489 patients with acute myocardial infarction, 54 were ≤ 45 years, and 435 were > 45 years. Young patients exhibited a higher prevalence of smoking and obesity, while patients > 45 years were more likely to have hypertension, diabetes mellitus, dyslipidemia, and previous myocardial infarction. Primary percutaneous coronary intervention in young patients was associated with the use of fewer guide catheters, shorter fluoroscopy time, and higher percentage of direct stent implantation. Young patients exhibited good in-hospital outcomes, with lower rate of adverse cardiac events (3.7% vs. 9.2%; p=0.30).
ConclusionsPatients aged ≤ 45 years accounted for approximately 10% of cases of ST-segment elevation acute myocardial infarction and exhibited high prevalence of modifiable risk factors.
O atual declínio observado na taxa de mortalidade entre pacientes com infarto do miocárdio com supradesnivelamento do segmento ST pode ser atribuído não apenas a maior utilização de estratégias de reperfusão, mas também a uma mudança no perfil demográfico dessa população, notadamente à redução em sua média de idade.
MétodosForam analisados retrospectivamente todos os pacientes submetidos à intervenção coronária percutânea primária no período de abril de 2010 a dezembro de 2014. O objetivo primário foi a caracterização dos fatores de risco mais prevalentes, a natureza angiográfica das lesões, os aspectos técnicos do procedimento e a evolução clínica hospitalar de pacientes jovens, com idade ≤ 45 anos, comparando-os àqueles com idade > 45 anos.
ResultadosDentre 489 pacientes com diagnóstico de infarto agudo do miocárdio, 54 tinham idade ≤ 45 anos e 435, idade > 45 anos. Pacientes jovens exibiram maior prevalência de tabagismo e obesidade, enquanto pacientes > 45 anos eram mais propensos a apresentar hipertensão arterial sistêmica, diabetes melito, dislipidemia e infarto do miocárdio antigo. Intervenção coronária percutânea primária em jovens associou-se ao uso de menor quantidade de cateteres-guia, menor tempo de fluoroscopia e maior porcentual de implante direto de stent. Pacientes jovens exibiram boa evolução hospitalar, com reduzida taxa de eventos cardíacos adversos (3,7% vs. 9,2%; p=0,30).
ConclusõesPacientes com idade ≤ 45 anos representaram aproximadamente 10% dos casos de infarto agudo do miocárdio com supradesnivelamento do segmento ST e exibiram elevada prevalência de fatores de risco modificáveis.
Data from the National Institutes of Health and from USA government agencies indicate that coronary artery disease was responsible for one in seven deaths in that country in 2011.1 It is estimated that, each year, 635,000 Americans are hospitalized for acute coronary syndrome. Although the mortality rate for ST-segment elevation acute myocardial infarction (STEMI) has decreased significantly - from 11.5%, in 1990, to 8.0%, in 2006-, this decrease can be attributed not only to advances in clinical pharmacotherapy and in reperfusion strategies, notably primary percutaneous coronary intervention (PCI), but also to changes in the demographic profile of patients.
Among these changes, the decline in the mean age of patients affected by STEMI stands out. A review of four French registries involving 6,707 people indicated a mean decrease from 66.2 to 63.3 years over the course of 15 years.2 In Brazil, the National Registry of Cardiovascular Interventions (Central Nacional de Intervenções Cardiovasculares - CENIC), encompassing 20,004 procedures in a 5-year period (2006-2010), recorded a mean age of 60.8 years among patients with STEMI.3
The in-hospital and late outcomes of young patients with stable coronary artery disease in our country were recently characterized, attesting to a good long-term prognosis.4,5 However, clinical and angiographic information about this population in the acute phase of STEMI are scarce. Thus, the aim of this study was to obtain more information on this subject.
MethodsStudy populationAll patients diagnosed with STEMI undergoing primary PCI in a single center performing a large volume of procedures (> 70 primary PCIs/year) were analyzed retrospectively. Patients aged ≤ 45 years were classified as young patients, based on previous publications on the subject.6–8
The primary aim of this study was the characterization of the most prevalent risk factors in young patients with STEMI, angiographic nature of lesions, technical details of primary PCI, and in-hospital clinical evolution, with emphasis on mortality rate, reinfarction, stroke, stent thrombosis, and the occurrence of major bleeding, comparing them to patients aged > 45 years.
ProceduresA 12-lead electrocardiogram, plus V3R, V4R, V7, and V8 leads in inferior infarction, were performed at hospital admission and 30-60minutes after the procedure. Therapeutic interventions followed recommendations and practices established by the existing guidelines.9,10 Anticoagulation was obtained with unfractionated heparin (UFH) 100 U/kg IV and dual antiplatelet therapy with a loading dose of 300mg of acetylsalicylic acid, plus clopidogrel 600mg or ticagrelor 180mg. The radial approach was the first choice of vascular access. Manual thrombus aspiration and use of glycoprotein IIb/IIIa inhibitors were at the discretion of the operator. Dosages of creatine kinase MB isoenzyme (CK-MB) were performed every 6hours, until a decrease in the level of this marker was observed.
DefinitionsThe following risk factors were assessed: smoking - active smoker, or abstinence from smoking occurring in less than 6 months; hypercholesterolemia (low density lipoprotein-cholesterol - LDL-C > 160mg/dL); systemic arterial hypertension (systolic blood pressure > 140mmHg and/or diastolic blood pressure > 90mmHg); diabetes mellitus (two fasting plasma glucose levels > 125mg/dL on different days); family history of heart disease (atherosclerosis diagnosed in parents or siblings < 55 years for men and < 65 for women); prior manifestation of atherosclerotic disease (previous myocardial infarction, percutaneous or surgical revascularization procedure, stroke); and chronic renal failure (glomerular filtration rate < 60mL/min or serum creatinine > 1.5mg/dL).
Regarding electrocardiographic location, acute myocardial infarction was classified as an anterior (anteroseptal, anterior, anterolateral, and extensive anterior) or inferior (inferior, lateral, and dorsal) event. Door-to-balloon time was defined as the interval between hospital admission and crossing of the lesion with a predilation balloon, manual thrombus aspiration catheter, or stent. Angiographic success was defined as a PCI with reduction of target stenosis to < 20% diameter, maintaining or restoring normal antegrade flow (Thrombolysis in Myocardial Infarction - TIMI grade 3). Major bleeding was defined as a Type 3 or 5 bleeding according to the definition of the Bleeding Academic Research Consortium: type 3 – (3a) bleeding with hemoglobin decrease ≥ 3 and < 5g/dL or with red blood cell transfusion; (3b) bleeding with hemoglobin decrease ≥ 5g/dL, or cardiac tamponade, or bleeding requiring surgical intervention, or bleeding requiring the use of intravenous vasoactive drugs; (3c) intracranial hemorrhage, or subcategories confirmed by autopsy, imaging studies, or lumbar puncture, or intraocular bleeding with vision impairment; Type 5 – (5a) likely fatal bleeding; (5b) final fatal bleeding.11
Statistical analysisQualitative variables were summarized in absolute frequencies and percentages, and quantitative data were expressed as mean±standard deviation. To compare groups, the Chi-squared test or Fisher's exact test for qualitative variables and Student's t-test or the Mann-Whitney test for quantitative variables were used. Results with p < 0.05 were considered statistically significant.
ResultsFrom April 2010 to December 2014, 2,674 PCIs were carried out; of these, 489 (18.3%) occurred in patients with STEMI in the first 12hours of sympton onset. Of these patients, 54 (11%) were aged ≤ 45 years (mean 40.7 years, range 36-45 years), and 435 were aged > 45 years (mean 64.2 years, range 46-96 years).
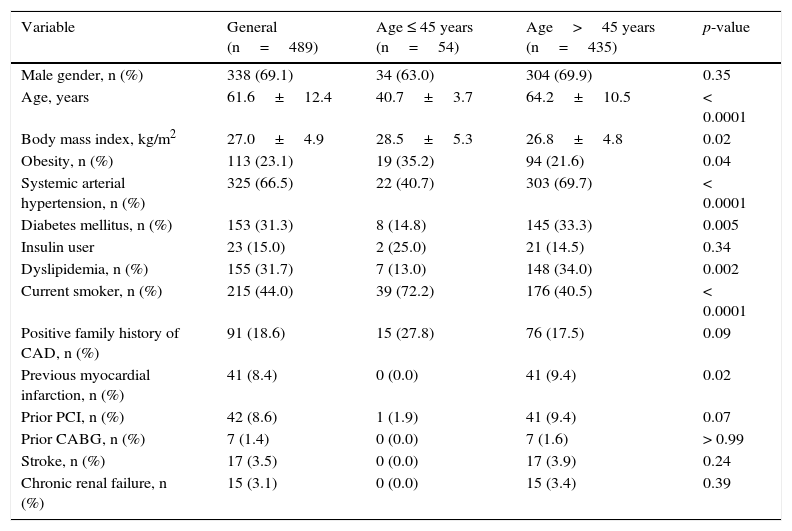
Young patients exhibited a higher prevalence of smoking (72.2% vs. 40.5%; p<0.0001) and obesity (35.2% vs. 21.6%; p=0.04), while patients > 45 years showed a greater propensity to present systemic arterial hypertension (69.7% vs. 40.7%; p<0.0001), diabetes mellitus (33.3% vs. 14.8%; p=0.005), dyslipidemia (34.0% vs. 13.0%; p=0.002), and previous myocardial infarction (9.4% vs. 0.0%; p=0.02; Table 1).
Basal clinical and demographic characteristics.
| Variable | General (n=489) | Age ≤ 45 years (n=54) | Age>45 years (n=435) | p-value |
|---|---|---|---|---|
| Male gender, n (%) | 338 (69.1) | 34 (63.0) | 304 (69.9) | 0.35 |
| Age, years | 61.6±12.4 | 40.7±3.7 | 64.2±10.5 | < 0.0001 |
| Body mass index, kg/m2 | 27.0±4.9 | 28.5±5.3 | 26.8±4.8 | 0.02 |
| Obesity, n (%) | 113 (23.1) | 19 (35.2) | 94 (21.6) | 0.04 |
| Systemic arterial hypertension, n (%) | 325 (66.5) | 22 (40.7) | 303 (69.7) | < 0.0001 |
| Diabetes mellitus, n (%) | 153 (31.3) | 8 (14.8) | 145 (33.3) | 0.005 |
| Insulin user | 23 (15.0) | 2 (25.0) | 21 (14.5) | 0.34 |
| Dyslipidemia, n (%) | 155 (31.7) | 7 (13.0) | 148 (34.0) | 0.002 |
| Current smoker, n (%) | 215 (44.0) | 39 (72.2) | 176 (40.5) | < 0.0001 |
| Positive family history of CAD, n (%) | 91 (18.6) | 15 (27.8) | 76 (17.5) | 0.09 |
| Previous myocardial infarction, n (%) | 41 (8.4) | 0 (0.0) | 41 (9.4) | 0.02 |
| Prior PCI, n (%) | 42 (8.6) | 1 (1.9) | 41 (9.4) | 0.07 |
| Prior CABG, n (%) | 7 (1.4) | 0 (0.0) | 7 (1.6) | > 0.99 |
| Stroke, n (%) | 17 (3.5) | 0 (0.0) | 17 (3.9) | 0.24 |
| Chronic renal failure, n (%) | 15 (3.1) | 0 (0.0) | 15 (3.4) | 0.39 |
CAD: coronary artery disease; PCI: percutaneous coronary intervention; CABG: coronary artery bypass graft.
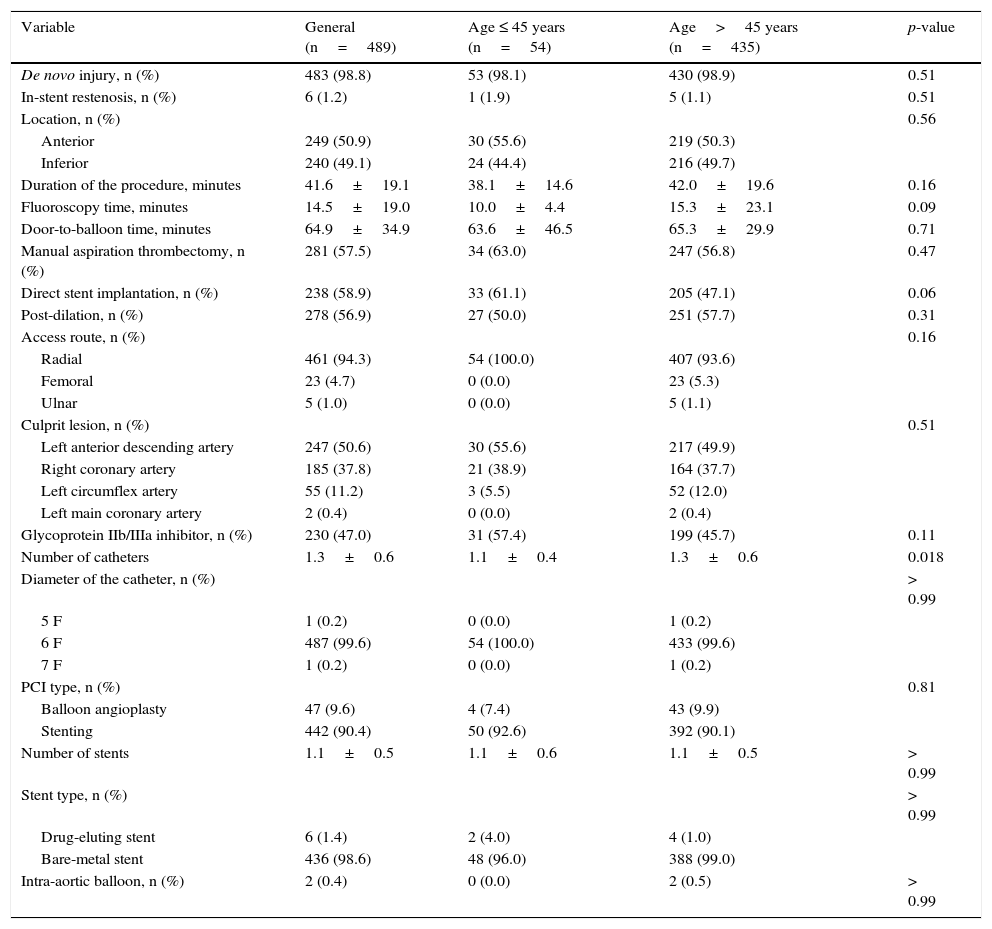
Anterior wall infarction was more frequent (50.9%), with stenting in 90.4% of procedures, predominantly with bare-metal stents (98.6%); manual aspiration thrombectomy, radial access, and glycoprotein IIb/IIIa inhibitors were used in 57.5%, 94.3%, and 47.0% of the cases, respectively, with no difference between groups (Table 2). Primary PCI in young patients was associated with the use of fewer guide catheters (1.1 vs. 1.3, p=0.02), shorter fluoroscopy time (10.0±4.4 vs. 15.3±23.1min; p=0.09), and a higher percentage of direct stenting (61.1% vs. 47.1%; p=0.06).
Angiographic and procedural characteristics.
| Variable | General (n=489) | Age ≤ 45 years (n=54) | Age>45 years (n=435) | p-value |
|---|---|---|---|---|
| De novo injury, n (%) | 483 (98.8) | 53 (98.1) | 430 (98.9) | 0.51 |
| In-stent restenosis, n (%) | 6 (1.2) | 1 (1.9) | 5 (1.1) | 0.51 |
| Location, n (%) | 0.56 | |||
| Anterior | 249 (50.9) | 30 (55.6) | 219 (50.3) | |
| Inferior | 240 (49.1) | 24 (44.4) | 216 (49.7) | |
| Duration of the procedure, minutes | 41.6±19.1 | 38.1±14.6 | 42.0±19.6 | 0.16 |
| Fluoroscopy time, minutes | 14.5±19.0 | 10.0±4.4 | 15.3±23.1 | 0.09 |
| Door-to-balloon time, minutes | 64.9±34.9 | 63.6±46.5 | 65.3±29.9 | 0.71 |
| Manual aspiration thrombectomy, n (%) | 281 (57.5) | 34 (63.0) | 247 (56.8) | 0.47 |
| Direct stent implantation, n (%) | 238 (58.9) | 33 (61.1) | 205 (47.1) | 0.06 |
| Post-dilation, n (%) | 278 (56.9) | 27 (50.0) | 251 (57.7) | 0.31 |
| Access route, n (%) | 0.16 | |||
| Radial | 461 (94.3) | 54 (100.0) | 407 (93.6) | |
| Femoral | 23 (4.7) | 0 (0.0) | 23 (5.3) | |
| Ulnar | 5 (1.0) | 0 (0.0) | 5 (1.1) | |
| Culprit lesion, n (%) | 0.51 | |||
| Left anterior descending artery | 247 (50.6) | 30 (55.6) | 217 (49.9) | |
| Right coronary artery | 185 (37.8) | 21 (38.9) | 164 (37.7) | |
| Left circumflex artery | 55 (11.2) | 3 (5.5) | 52 (12.0) | |
| Left main coronary artery | 2 (0.4) | 0 (0.0) | 2 (0.4) | |
| Glycoprotein IIb/IIIa inhibitor, n (%) | 230 (47.0) | 31 (57.4) | 199 (45.7) | 0.11 |
| Number of catheters | 1.3±0.6 | 1.1±0.4 | 1.3±0.6 | 0.018 |
| Diameter of the catheter, n (%) | > 0.99 | |||
| 5 F | 1 (0.2) | 0 (0.0) | 1 (0.2) | |
| 6 F | 487 (99.6) | 54 (100.0) | 433 (99.6) | |
| 7 F | 1 (0.2) | 0 (0.0) | 1 (0.2) | |
| PCI type, n (%) | 0.81 | |||
| Balloon angioplasty | 47 (9.6) | 4 (7.4) | 43 (9.9) | |
| Stenting | 442 (90.4) | 50 (92.6) | 392 (90.1) | |
| Number of stents | 1.1±0.5 | 1.1±0.6 | 1.1±0.5 | > 0.99 |
| Stent type, n (%) | > 0.99 | |||
| Drug-eluting stent | 6 (1.4) | 2 (4.0) | 4 (1.0) | |
| Bare-metal stent | 436 (98.6) | 48 (96.0) | 388 (99.0) | |
| Intra-aortic balloon, n (%) | 2 (0.4) | 0 (0.0) | 2 (0.5) | > 0.99 |
PCI: percutaneous coronary intervention.
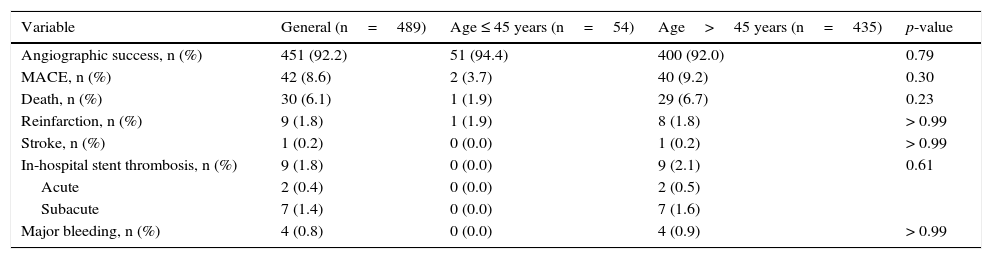
The overall angiographic success rate was high (92.2%); and young patients exhibited good in-hospital evolution, with reduced mortality (1.9% vs. 6.7%; p=0.23) and reinfarction (1.9% vs. 1.8%; p>0.99) rates and no occurrence of stroke, stent thrombosis, and major bleeding (Table 3).
In-hospital efficacy and safety outcomes.
| Variable | General (n=489) | Age ≤ 45 years (n=54) | Age>45 years (n=435) | p-value |
|---|---|---|---|---|
| Angiographic success, n (%) | 451 (92.2) | 51 (94.4) | 400 (92.0) | 0.79 |
| MACE, n (%) | 42 (8.6) | 2 (3.7) | 40 (9.2) | 0.30 |
| Death, n (%) | 30 (6.1) | 1 (1.9) | 29 (6.7) | 0.23 |
| Reinfarction, n (%) | 9 (1.8) | 1 (1.9) | 8 (1.8) | > 0.99 |
| Stroke, n (%) | 1 (0.2) | 0 (0.0) | 1 (0.2) | > 0.99 |
| In-hospital stent thrombosis, n (%) | 9 (1.8) | 0 (0.0) | 9 (2.1) | 0.61 |
| Acute | 2 (0.4) | 0 (0.0) | 2 (0.5) | |
| Subacute | 7 (1.4) | 0 (0.0) | 7 (1.6) | |
| Major bleeding, n (%) | 4 (0.8) | 0 (0.0) | 4 (0.9) | > 0.99 |
MACE: major adverse cardiac events (death, reinfarction, stroke, stent thrombosis, or major bleeding).
Although hospitalizations for acute myocardial infarction currently present a downward trend, this is not observed in young patients.12 Consequently, the statistics show a decline in the mean age of STEMI cases, as well as in mortality rate, and these findings are justified by the prognostic impact of advanced age in this high-risk scenario, representing one of its main determinants of morbidity and mortality.13
Data from registries such as FAST-MI (French Registry of Acute ST-Elevation or non-ST-elevation Myocardial Infarction) still show increased prevalence of smoking (from 32.0% to 40.9%) and obesity (from 14.3% to 20.1%) in the population of myocardial infarction patients over the past 15 years.2 In the USA, among young individuals aged 18-44 years, 22.9% of men and 16.6% of women are smokers, and 69% of the general population is classified as obese or overweight.1
In assessing the population of young patients with an acute myocardial infarction diagnosis, the percentage of smokers can reach up to 74%, as in the CRAGS (Coronary Artery Disease in Young Adults) study.14 It is known that smoking contributes negatively in the regulation cascades engaged in preventing coronary occlusion, besides promoting changes in tissue plasminogen activator response to bradykinin. Furthermore, the hypercoagulability state and endothelial dysfunction present in smokers predispose to the formation of intracoronary thrombi.15
In the present study, patients aged ≤ 45 years represented 11% of all STEMI cases (37% female), with high prevalence of modifiable risk factors such as obesity (35.2%) and smoking (72.2%), and lower percentages of hypertension, dyslipidemia, diabetes mellitus, and previous myocardial infarction. The characteristics of procedures – for instance, a lower mean number of catheters used, shorter fluoroscopy time, and higher percentage of direct stent implantation – suggest less angiographic complexity in this subgroup, as well as a low rate of major adverse cardiac events during hospitalization, exemplified by mortality rates of 1.9% vs. 6.7% in patients > 45 years. Similar findings were reported by the London Chest Hospital, a reference center for chest pain, which, from 2004 to 2012, registered 3,618 primary PCIs. Patients aged ≤ 45 years constituted 10.1% of the sample, and smoking had a prevalence of 62.7%, with a 30-day mortality of 1.6%.16
Together, these data reflect the importance of instituting health policies that address young people and target primary or secondary prevention, with emphasis on changes in lifestyle, particularly smoking cessation, regular physical activity, and a balanced diet to maintain proper weight. These are low-cost actions with great potential for reducing the incidence of new cases of myocardial infarction in this population.
Study limitationsThis analysis had the following limitations: its observational and unicentric nature, the limited sample size, lack of long-term clinical follow-up, as well as non-performance of routine diagnostic tests for illicit drugs such as cocaine, a known promoter of coronary spasm and hypercoagulability in an environment of sympathetic activity exacerbation, which represents a common cause of acute coronary syndrome in young people.
ConclusionsPatients aged ≤ 45 years represented approximately 10% of cases of ST-segment elevation acute myocardial infarction, showed high prevalence of modifiable risk factors, especially smoking, favorable in-hospital clinical outcome after primary percutaneous coronary intervention, and less technical complexity when compared to patients > 45 years. Health policies addressing changes in lifestyle are low-cost actions, with potential impact on reducing future events in this population.
Funding sourceNone declared.
Conflicts of interestThe authors declare no conflicts of interest.
Peer Review under the responsability of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.