Renal artery fibromuscular dysplasia is a condition of unknown etiology, with non-inflammatory, non-atherosclerotic origin, associated to the development of stenosis and aneurysms. The authors report a case of bilateral renal artery fibromuscular dysplasia associated with a large renal artery aneurysm, treated with balloon angioplasty and a multilayer stent.
A fibrodisplasia muscular renal tem etiologia desconhecida, é de origem não inflamatória e não aterosclerótica, estando associada ao desenvolvimento de estenoses e de aneurismas. Relatamos um caso de fibrodisplasia muscular renal bilateral associada a aneurisma volumoso de artéria renal tratado com angioplastia com balão e stent multicamadas.
Fibromuscular dysplasia is a disease with unknown etiology that affects medium-caliber arteries, causing vessel stenosis. This condition typically affects women aged between 20 and 50 years, with renal artery aneurysm as one of its complications.1 Renal artery aneurysm is a rare condition, with a prevalence of 0.01% in autopsy studies.2 In the last decade, the availability of non-invasive diagnostic methods, such as Doppler ultrasound (DUS) and computed tomography angiography (CTA), has contributed to the increased detection of renal artery aneurysms.2
With the advent of interventional radiology, the treatment of these two pathologies became feasible and less invasive. In this report, the authors describe the approach for a case of bilateral renal fibromuscular dysplasia complicated with a massive aneurysm in a patient with a difficult-to-control secondary hypertension.
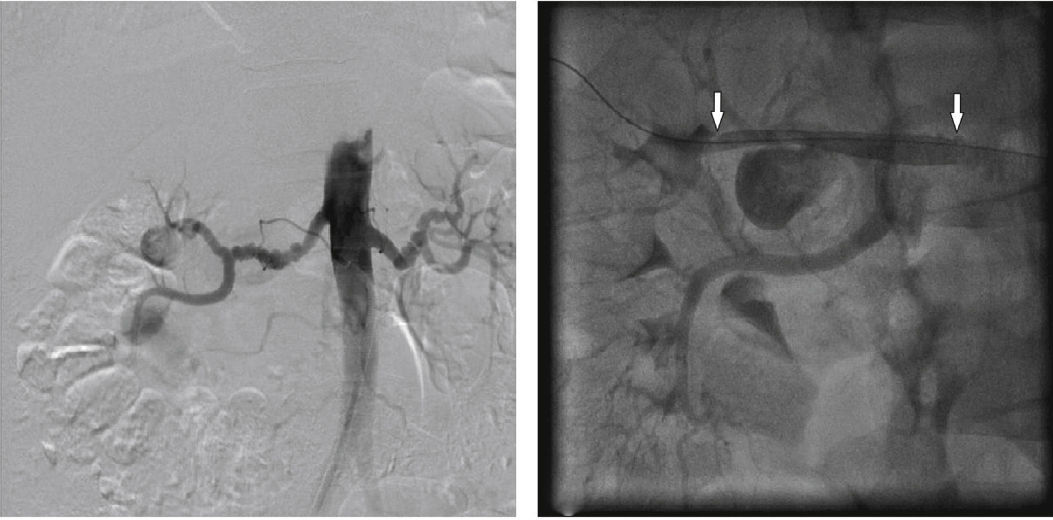
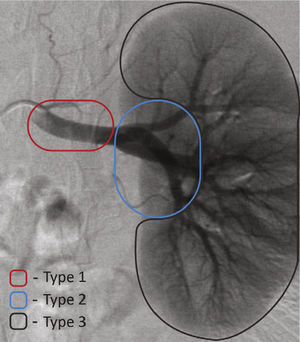
Case reportA 36-year-old woman with arterial hypertension had the diagnosis of renal artery aneurysm through DUS of renal arteries, which identified a saccular dilation in the right renal artery upper branch > 2.0cm, and a hemodynamically significant bilateral stenosis. Digital subtraction arteriography demonstrated a stenosis at the midportion of the right renal artery, in association with saccular dilation in its upper pole branch near the renal hilum, and a left renal artery with stenosis in its middle and distal thirds, both with the “string-of-beads” sign compatible with a diagnosis of renal artery fibromuscular dysplasia (Fig. 1).
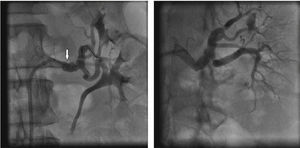
Digital subtraction aortography and final renal angiography after multilayer stenting. On the left, abdominal aortogram showing bilateral renal fibrodysplasia with a massive right renal artery aneurysm. On the right, final arteriography after multilayer stenting. The arrows point to the beginning and the end of the stent.
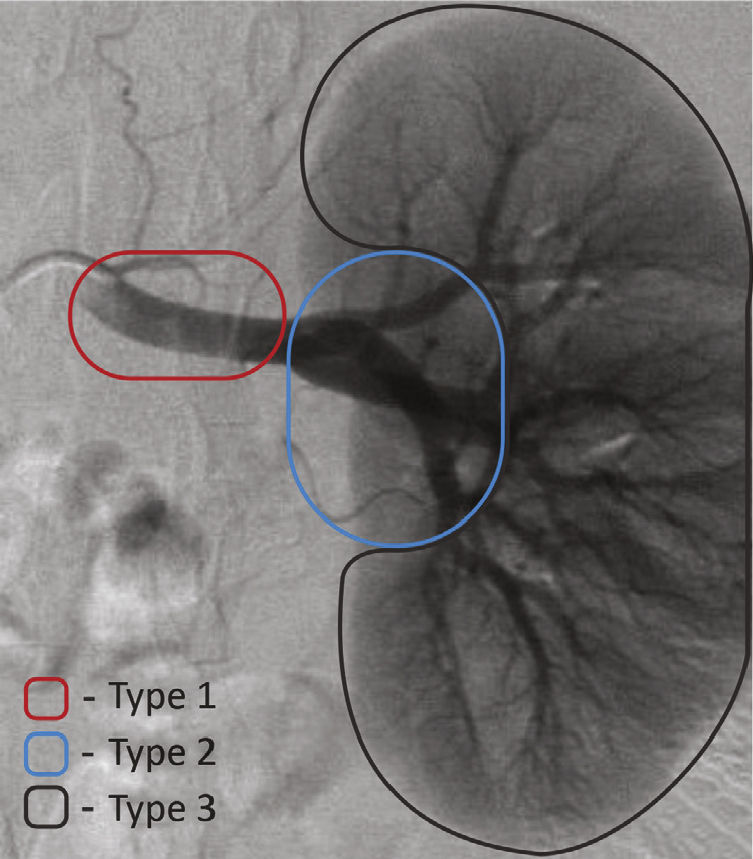
The endovascular treatment of this renal artery aneurysm was planned after having established its location (Fig. 2).3 Because this was a type-2 aneurysm in the presence of a significant renal segmental branch, the decision was made in favor of an angioplasty with the use of a multilayer stent (MultilayerTM, Cardiatis, Isnes, Belgium), in order to preserve the segmental vascularization and to exclude the right renal artery aneurysm. The left renal artery was treated with balloon angioplasty.
The procedure was performed in the catheterization laboratory with the patient under local anesthesia. Antibiotic prophylaxis were performed with 1.5g cefuroxime, and the approach was done through the right common femoral artery. The radiographic control was performed by a Siemens Artis Flat Panel system (Siemens AG, Berlin, Germany).
An arteriography was performed, followed by selective catheterization of the right renal artery with a Judkins right 5 F catheter and with the positioning of a 6 F, 45cm DestinationTM sheath (Terumo Interventional Systems, Somerset, USA). A 0.018-inch, 195-cm V-18TM Control WireTM guide wire (Boston Scientific, Natick, USA) was placed in the interlobar branch of the right renal artery, and a 6-mm × 30-mm multilayer stent (MultilayerTM; Cardiatis, Isnes, Belgium) was released in proper position, which promoted the exclusion of the aneurysm and secured the patency of the bifurcation close to the neck (Fig. 1).
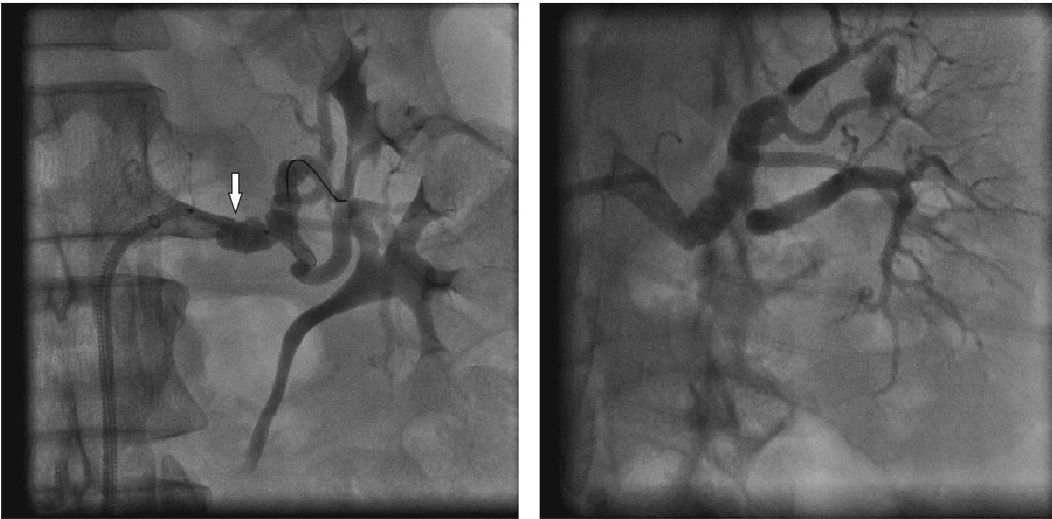
The left renal artery was managed by selective catheterization with the same technique and with the introduction of a 6-mm × 20-mm AviatorTM Plus semi-compliant balloon (Cordis Corporation, Warren, USA) in association with a 0.014-inch, 180cm V-14TM Control WireTM guide wire (Fig. 3).
Treatment of left renal fibrodysplasia with balloon angioplasty. On the left, angioplasty balloon placement at the level of renal fibrodysplastic lesion. The white arrow indicates the angioplasty balloon. On the right, final arteriography after endovascular treatment of renal fibrodysplasia.
The angioplasty procedures, with stenting on the right and with balloon on the left, resulted in an immediate technical and therapeutic success, documented with the final control angiography (Figs. 1 and 3).
Postoperative follow-upOn the first day after the procedure, the patient complained of low back pain in the right side, associated with hematuria and a slight increase in creatinine (0.7mg/dL before the procedure vs. 0.9mg/dL after the procedure). Due to the persistent low back pain, even with the improvement of hematuria and the normalization of kidney function, CTA was indicated on the fifth day after the procedure. The examination showed occlusion of the multilayer stent and signs of right kidney upper pole ischemia, with thrombosis of the aneurysm. The left renal artery was pervious, and the left kidney showed no signs of ischemia (Fig. 4).
Postoperative computed tomography angiography of the treatment of the right renal artery aneurysm. On the left, the arrow indicates a hypodense region in the right renal parenchyma devoid of vascularization, compatible with renal ischemic infarction. In the middle panel, the arrow indicates preservation of a renal segmental branch from the multilayer stent. On the right, three-dimensional volumetric reconstruction of abdominal aorta and renal arteries. The arrow indicates the position of the multilayer stent in the renal artery.
During the in-hospital follow-up, the patient developed an uncontrollable and persistent pain, even with the use of analgesics and opioids, and the Urological Department Surgery opted for a partial nephrectomy.
Currently, the patient is receiving outpatient treatment, with improvement in blood pressure, use of only one antihypertensive drug class, and creatinine levels similar to those of the pre-procedure period.
DiscussionFibromuscular dysplasia was first described in 1938 by Leadbetter and Burkland.4 Although a long-established disease, it has been little studied in the past 30 years. New information about its clinical course, pathophysiology, and treatment modalities appeared 3 years ago, leading to the establishment of the United States Registry for Fibromuscular Dysplasia.5 In the light of modern knowledge, what is known about this disease is that it has a non-inflammatory, non-atherosclerotic etiology, most commonly affects young white women, and more often affects renal and extracranial carotid arteries.5 Its manifestation depends on the affected vascular territory, presenting with high blood pressure (the most frequent finding), transient ischemic attack, or stroke; or it may remain asymptomatic for years, being diagnosed on imaging studies. Of all 447 patients evaluated by the United States Registry for Fibromuscular Dysplasia, 294 had renal artery muscle fibrodysplasia; of these, 25 had an associated renal aneurysm.5
The lesion caused by renal artery fibromuscular dysplasia is responsible for 10% of cases of renovascular hypertension. It is located in the mid and distal portions of the renal artery, thereby differing from atherosclerotic pathologies, which usually are located in the proximal portion of the vessel, due to their close relationship with the progression of aortic atherosclerotic disease to its branches. Bilateral involvement of renal arteries occurs in 39% of cases.5
Balloon angioplasty is the treatment of choice in symptomatic patients with renal artery muscle fibrodysplasia. This type of therapy has high rates of technical and clinical success, with lower complication rates when compared to conventional surgical treatment. Balloon angioplasty is also less invasive, requires less recovery time, and is less expensive.6 Stents are used as a bailout strategy when the balloon angioplasty had unsatisfactory results in the presence of dissection with flow restriction and/or acute occlusion. Its has the disadvantage of preventing surgical revascularization.6
Renal artery aneurysms are rare. Their prevalence in autopsy studies is 0.01%; however, in patients selected for renal arteriography, its prevalence can reach 0.3-1%. These conditions are prevalent among women because of their strong association with renal artery fibromuscular dysplasia.1,2
There is general agreement in the literature that renal artery aneurysms should be treated when: (1) these lesions measure > 2cm or after documented growth; (2) are associated with symptoms; (3) in face of a documented distal embolization; (4) are diagnosed in women of child-bearing age or during pregnancy; or (5) are associated with significant stenosis and poor renal perfusion.2,3
Rundback et al. classified renal aneurysms according to their angiographic location, making it easier to establish treatment strategies.3 Type-2 renal artery aneurysms were formerly treated only by conventional surgery or nephrectomy. These lesions are a therapeutic challenge for endovascular technique due to anatomical difficulty, and were the type covered in this study.
In these cases, the use of remodeling techniques with stenting associated with coils, or with coils and glue, is critical to the preservation of native vessels and the proper sealing of the aneurysm. Brazilian authors have reported their initial experience with this type of aneurysm, using the remodeling technique with satisfactory results.7
Currently, the use of the multilayer stent (MultilayerTM) has been reported as an option for the correction of peripheral aneurysms with good results. This type of device is composed of non-coated, interconnected layers which modify the flow (from turbulent to laminar), decreasing the blood flow rate which leads to a thrombosed aneurysm, and maintaining the patency of existing branches. Ruffino et al. prospectively evaluated 54 patients with peripheral aneurysms (9 of them with visceral origin) treated with the MultilayerTM device, resulting in primary patency of the branch in 87.0%, secondary patency in 91.0%, and complete exclusion of the aneurysm in 93.3%. Stent occlusion occurred in 11% (n = 6), and mortality in 3.7% (n = 2) of cases within 1 year.8 In the present report, there was failure of the multilayer stent with consequent thrombosis around the whole renal upper pole, culminating in uncontrolled pain and subsequent partial nephrectomy.
Funding sourceNone.
Conflicts of interestThe authors declare no conflicts of interest.
Peer Review under the responsability of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.