This article reports an anatomic specimen specifically prepared to demonstrate a rare anomaly of the origin of the left coronary artery from the right sinus of Valsalva, with an incidence of 0.15% in patients undergoing coronary angiography. This is a subgroup of coronary artery anomalies with the greatest potential for clinical repercussions, especially sudden death in young patients. Based on current knowledge, pathophysiologic mechanisms, diagnosis and treatment options of anatomical variations of the anomalous origin of a coronary artery from the contralateral sinus are discussed.
Origem Anômala da ArtériaCoronária Esquerda do Seio de Valsalva Direito
Trazemos neste artigo a descrição de uma peça anatômica especificamente preparada para demonstrar uma rara anomalia da origem da artéria coronária esquerda do seio de Valsalva direito, com incidência de 0,15% em pacientes submetidos a cinecoronariografia. Trata-se de um subgrupo de anomalias das artérias coronárias que tem o maior potencial para repercussões clínicas, em especial a morte súbita em jovens. Discutimos, à luz dos conhecimentos atuais, os mecanismos fisiopatológicos, o diagnóstico e as opções de tratamento das variações anatômicas da origem anômala da artéria coronária do seio contralateral.
The heart is perfused by the coronary arteries and their branches, which originate from the sinuses of Valsalva. Generally, the right coronary artery originates from the right anterior sinus of Valsalva, passing through the coronary groove, and emerging between the pulmonary artery trunk and right atrium. In turn, the left coronary artery originates in the left anterior sinus of Valsalva, behind the pulmonary artery, passing through the coronary groove, and emerging between the pulmonary trunk and left atrium.1
Coronary artery anomalies result from disturbances that occur in the third week of fetal development.2 These changes cause anatomical variations related to the origin, trajectory, and termination of these arteries, or alterations in their intrinsic anatomy. Some coronary artery anomalies cause occasional or obligatory ischemia (anomalous origin of the left coronary artery from the pulmonary artery), whereas others predispose to complications (spasm or development of atheromatous plaques).3
This study aimed to discuss a rare case of anomalous origin of the coronary artery, detected in an anatomic specimen from the anatomy laboratory of a medical school.
CASE REPORTA mold of the coronary circulation was prepared from the anatomical specimen by filling the vessels by injecting silicone rubber dissolved in chloroform, which was subsequently hardened with a catalyst (peroxol). Red dye was used in the arteries, and blue in the veins. Once prepared, the piece was immersed in 10% formalin and removed after 24 hours. The cavities were filled with resin (RESAPOL T208), and then corrosion was performed with sulfuric acid. Approximately one week was required to complete the preparation of the piece.
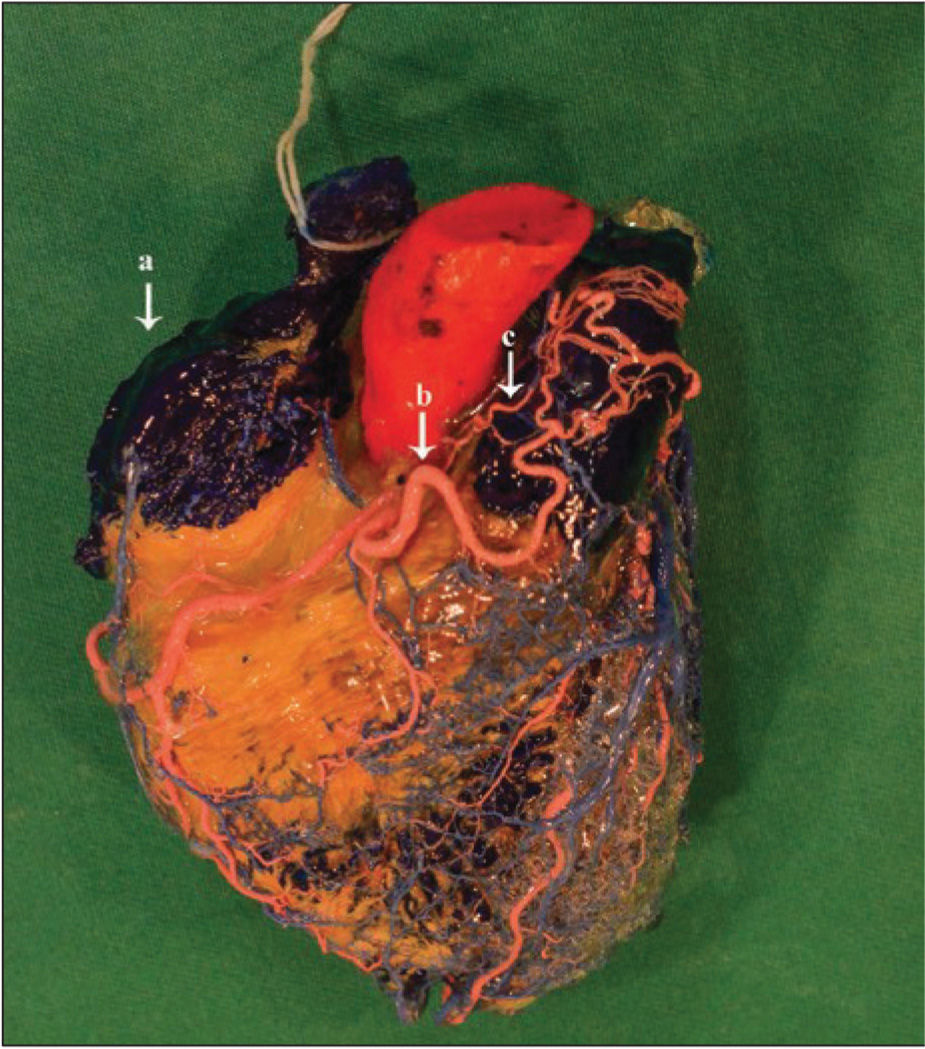
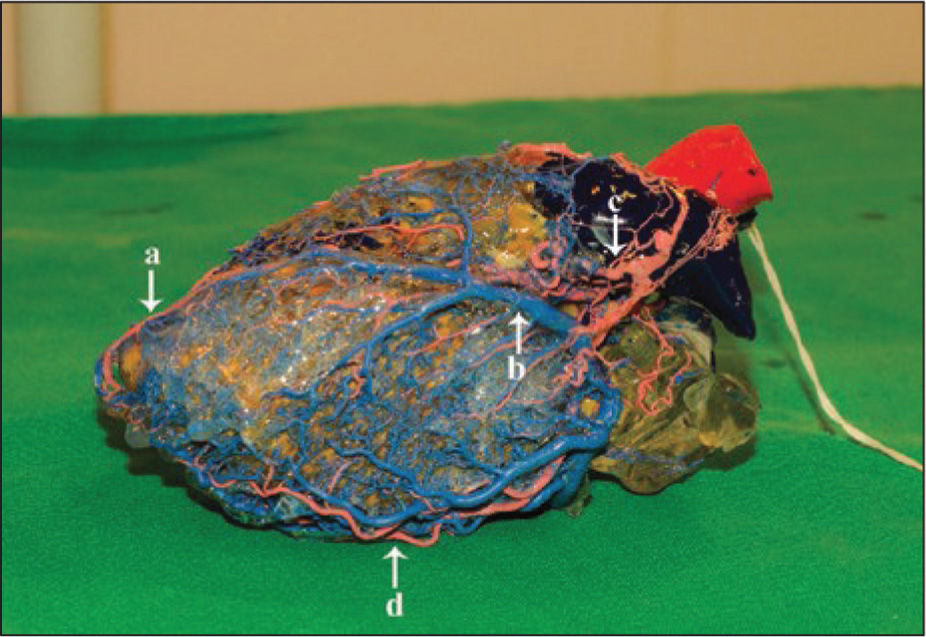
In the investigated anatomic specimen (Figures 1 and 2), the left coronary artery originated from the right sinus of Valsalva, near the right coronary artery, with a pre-pulmonary (or pre-cardiac) trajectory, i.e., a trajectory anterior to the pulmonary artery trunk, originating branches that anastomosed to each other. Among these branches, the left circumflex artery, two marginal arteries, and the left anterior descending artery were identified, all showing smaller calibres than usual.
– The model shows the origin of the left coronary artery from the right coronary sinus and its anterior distribution to the pulmonary artery trunk, as well as the origin of the aortic cone above the coronary sinus, anastomosing with the branches of the left coronary artery. (a, right atrium; b, left coronary artery; c, cone branch)
During inspection with magnifying glass and reflectors, an anomaly in the cone artery was also observed, which arose directly from the aorta. The cone branch had tortuous and ascending trajectory in the pulmonary trunk, where it joined the abovementioned network of anastomoses, also characterizing an anomaly of its origin and trajectory.
DISCUSSIONCoronary anomalies are classified broadly into four groups: 1) anomalies of coronary origin and trajectory (absence of left main coronary artery, anomalous location of coronary ostium inside or outside the appropriate sinus of Valsalva, anomalous location of the coronary ostium in inappropriate sinus of Valsalva, and single coronary artery); 2) intrinsic abnormalities of coronary anatomy (atresia or stenosis of the coronary ostia, coronary aneurysm, coronary hypoplasia, and myocardial bridge); 3) anomalies of terminal coronary circulation (fistulas to cardiac chambers, inferior vena cava, or pulmonary arteries and veins); and 4) anomalous anastomotic vessels.3
The origin of the left coronary artery from the right sinus of Valsalva occurred in 0.15%, while the origin of the right coronary artery from the left sinus of Valsalva occurred in 0.92% of cases, totalling an incidence of 1.07% of coronary arteries arising from the contralateral sinus in a consecutive series of 1,950 angiograms reviewed for detection of coronary abnormalities.4 Five coronary trajectories originating in contralateral aortic sinuses are possible: retrocardiac, retroaortic, pre-aortic (between the aorta and the pulmonary artery), intraseptal (supracristal), and pre-pulmonary (pre-cardiac).3
The origin of the coronary artery from the contralateral sinus may be associated with poor prognosis in young individuals, especially the anomalous coronary with pre-aortic trajectory, between the aorta and pulmonary artery. The classic "scissors-like" mechanism that causes ischemia, to which the anomalous artery would be subject due to the proximity of the aorta and the pulmonary artery, was recently questioned by Angelini et al.5 The authors state that the point of greatest aortopulmonary proximity is located within the aortic wall, and intravascular ultrasound studies have demonstrated that this coronary anomaly is associated with intramural proximal intussusception of the ectopic artery on the wall of the aortic root. The mechanisms potentially associated with stenosis of this segment would be coronary hypoplasia (intramural circumference of the vessel lower than that of the distal vessel), lateral compression (ovoid rather than circular cross-section of the intramural artery), and the length of the stenotic segment, which varies from 5mm to 15mm. The distensibility of the aortic wall is another potential mechanism, which would depend on the characteristics of the vessel wall and changes in aortic pressure. This mechanism possibly explains why sudden death occurs only in young patients, due to the progressive stiffening of the aortic wall in adults.5
The clinical presentation of cases of coronary artery arising from the contralateral sinus occurs by sudden death (usually in young patients after strenuous physical exertion) or uncharacteristic symptoms. When investigating atypical chest pain, coronary angiography performed due to false positive functional tests or concomitant atherosclerosis can detect this anomaly. Angelini et al.5 opine that symptomatic patients should be treated with beta-blockers and should be advised to avoid strenuous physical exertion. Percutaneous or surgical treatment is reserved for anomalies with preaortic trajectories. Most patients with right coronary artery originating from the left sinus of Valsalva do not need treatment, and coronary intervention with drugeluting stent implantation is reserved for symptomatic cases and intramural abnormal vessel area<50% of the distal vessel area or reversible ischemia detected by myocardial scintigraphy. For cases of left coronary artery originating from the right sinus of Valsalva, the current indication is for surgical correction (externalization of the intramural segment of the anomalous vessel or creation of new coronary ostium in the distal emergence of the intramural segment).3
In the present case, clinical data and the cause of death of the patient were not available. Considering the knowledge accumulated to date, it is likely that the pre-pulmonary trajectory of the left coronary artery found in this case did not contribute to the patient‘s death.
CONFLICT OF INTERESTThe authors declare no conflicts of interest.