Although predilation during primary percutaneous coronary intervention offers greater predictability for stent implantation, it is associated with complications that may negatively influence immediate and late outcomes. The objective of this study was to characterize procedures requiring predilation, comparing them to those performed by direct stent implantation.
MethodsPrimary percutaneous coronary interventions registered at the Central Nacional de Intervenc¿o¿es Cardiovasculares (CENIC) from 2006 to 2016 were analyzed. The clinical and angiographic profiles of the procedures performed with or without predilation, hospital outcome measures, and predictors of mortality were characterized.
ResultsThe sample consisted of 17,515 patients. Those who underwent predilation differed from the direct stent implantation group regarding clinical characteristics, with a higher prevalence of elderly, women, and associated comorbidities. In the first group, the rates of calcified lesions, bifurcations, occlusions, and multivessel coronary disease were higher. Intervention failure rates were also higher in patients undergoing predilation, as well as the rates of major adverse cardiac events. In the multiple logistic regression model, the need for predilation was correlated with the occurrence of hospital death.
ConclusionsPrimary percutaneous coronary intervention requiring predilation was characterized by a higher prevalence of clinical comorbidities and by angiographic and technical complexity of the procedures. Predilation is an independent predictor of hospital mortality in this clinical setting.
Embora a pré-dilatação durante a intervenção coronária percutânea primária confira maior previsibilidade ao implante do stent, ela associa-se a complicações que podem influenciar negativamente em seus resultados imediatos e tardios. O objetivo deste estudo foi caracterizar os procedimentos com necessidade de pré-dilatação, comparando-os àqueles realizados pelo implante direto de stent.
MétodosForam analisadas as intervenções coronárias percutâneas primárias cadastradas na Central Nacional de Intervenções Cardiovasculares (CENIC) durante o período de 2006 a 2016, tendo sido caracterizados os perfis clínico e angiográfico dos procedimentos efetivados com ou sem pré-dilatação, aferição de desfechos hospitalares e preditores de mortalidade.
ResultadosA amostra foi composta por 17.515 pacientes. Aqueles submetidos à pré-dilatação diferiram do grupo stent direto, quanto às características clínicas, com maior prevalência de idosos, mulheres e comorbidades associadas. No primeiro, as taxas de lesões calcificadas, bifurcações, oclusões e coronariopatia multiarterial foram maiores. Também foram maiores as taxas de insucesso da intervenção entre pacientes submetidos à pré-dilatação e de eventos cardíacos adversos maiores. No modelo de regressão logística múltipla, a necessidade de pré-dilatação correlacionou-se com a ocorrência de óbito hospitalar.
ConclusõesA intervenção coronária percutânea primária com necessidade de pré-dilatação caracterizou-se pela maior prevalência de comorbidades clínicas entre os pacientes e pela complexidade angiográfica e técnica dos procedimentos. A pré-dilatação constituiu-se em variável preditora independente de mortalidade hospitalar neste cenário clínico.
Primary percutaneous coronary intervention (PCI), when performed in a timely manner and by a trained team, is considered the treatment of choice for ST-elevation myocardial infarction (STEMI).1 Stent implantation during the procedure is known to reduce acute complications and restenosis rates, increasing angiographic success.2 During primary PCI, two technical approaches are possible: the classic, with balloon predilation before endoprosthesis deployment, and direct stent implantation, without predilation.
The classic technique allows the best crossing and delivery of the stent in the lesion. However, balloon insufflation may cause barotrauma in the fragile vessel, leading to immediate complications, such as dissection, thrombosis, and microvascular obstruction; it can also influence late results, such as increased risk of target vessel failure.3,4 Thus, direct stent implantation is recommended in selected cases, with potential improvement in the final epicardial flow, reduction in procedure duration and costs, reduced radiation exposure, and benefits regarding adverse clinical outcomes.5–8
The patient's emergency condition in the presence of an acute myocardial infarction (AMI) makes this an essential subject; however, there are few conclusive data available in the literature. This article aimed to characterize procedures requiring predilation, comparing them to those performed by direct stent implantation.
MethodsThe Central Nacional de Intervenção Cardiovascular (CENIC) is an official organ of the Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista (SBHCI) created in 1991 to document the performance and evolution of the specialty in Brazil. It comprises a database of voluntary contributions from the full and aspiring members of this society who are authorized to practice PCI, comprising the five geographic regions of Brazil. Its coordinating center is located at the headquarters of SBHCI, in São Paulo (SP), and its operating system works through the collection of data in pre-specified telecards filled out electronically; they are identical for all the participating centers, as previously described.9 PCI data collection began in 1992, and the new percutaneous instruments, different from coronary balloon angioplasty, were incorporated as of the second half of 1995.
This analysis used the data related to primary PCI performed between 2006 and 2016. The following criteria and definitions established by CENIC were used, after the interventionists’ consideration: predilation with balloon prior to stent implantation; procedural success in obtaining a residual lesion < 30%; occurrence of in-hospital severe adverse outcomes: death and acute vessel occlusion; reinfarction or emergency surgery, if performed as a result of acute or subacute target vessel occlusion or triggered due to other modalities of percutaneous coronary intervention failure, accompanied by acute myocardial ischemia.
Statistical analysisCategorical variables were expressed as absolute numbers and percentages and compared using the chi-squared test. Fisher's exact test or the likelihood ratio test were used when necessary. Continuous variables were expressed as means and standard deviations and compared by analysis of variance (ANOVA). Simple and multiple logistic regression models were used to verify the influence of variables of interest in relation to mortality. A significance level of 5% (p < 0.05) was considered in all analyses.
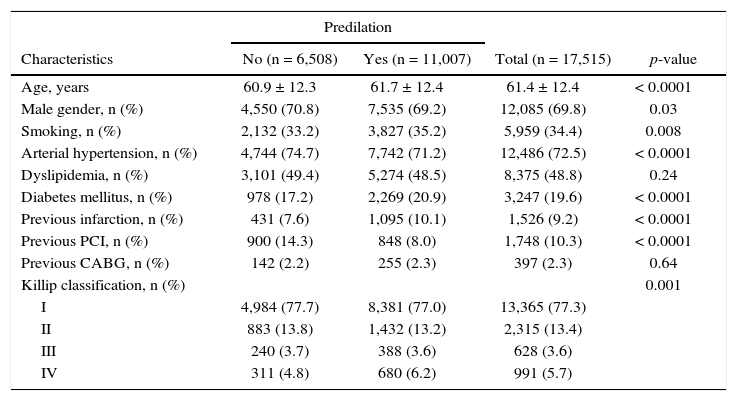
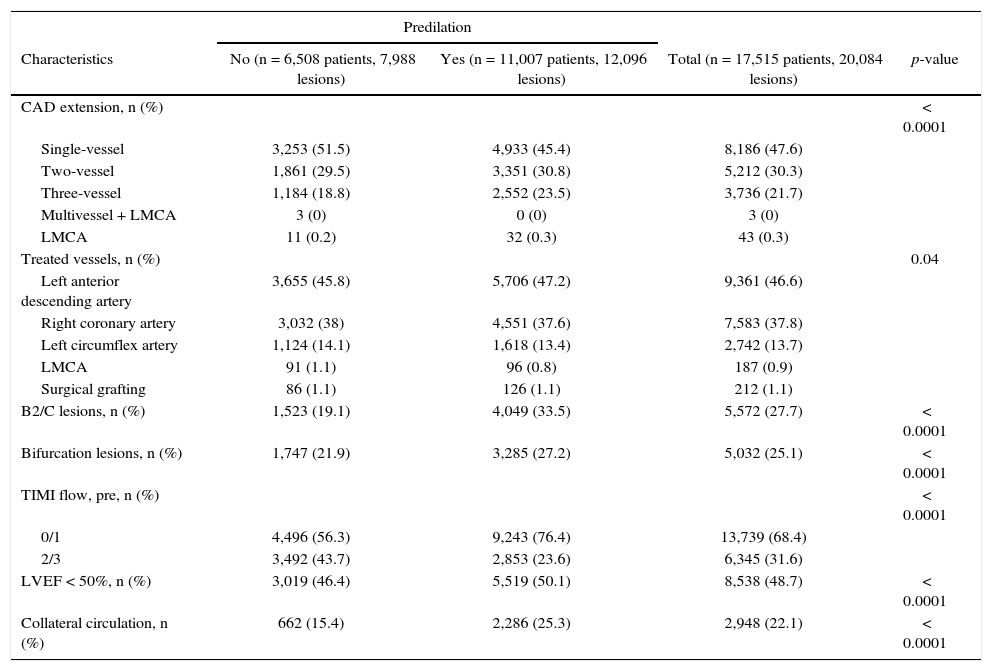
ResultsThe sample of the present analysis consisted of 17,515 patients and 20,084 lesions treated between June 2006 and March 2016. Those who underwent primary PCI with predilation differed from those who underwent direct stent implantation in relation to clinical characteristics, with a higher prevalence of elderly individuals, women, and associated comorbidities (Table 1). Moreover, there was a higher rate of calcified lesions, bifurcations, occlusions, and multivessel coronary artery disease in the first group, which resulted in greater angiographic complexity of the cases (Table 2).
Patients’ characteristics.
| Predilation | ||||
|---|---|---|---|---|
| Characteristics | No (n = 6,508) | Yes (n = 11,007) | Total (n = 17,515) | p-value |
| Age, years | 60.9 ± 12.3 | 61.7 ± 12.4 | 61.4 ± 12.4 | < 0.0001 |
| Male gender, n (%) | 4,550 (70.8) | 7,535 (69.2) | 12,085 (69.8) | 0.03 |
| Smoking, n (%) | 2,132 (33.2) | 3,827 (35.2) | 5,959 (34.4) | 0.008 |
| Arterial hypertension, n (%) | 4,744 (74.7) | 7,742 (71.2) | 12,486 (72.5) | < 0.0001 |
| Dyslipidemia, n (%) | 3,101 (49.4) | 5,274 (48.5) | 8,375 (48.8) | 0.24 |
| Diabetes mellitus, n (%) | 978 (17.2) | 2,269 (20.9) | 3,247 (19.6) | < 0.0001 |
| Previous infarction, n (%) | 431 (7.6) | 1,095 (10.1) | 1,526 (9.2) | < 0.0001 |
| Previous PCI, n (%) | 900 (14.3) | 848 (8.0) | 1,748 (10.3) | < 0.0001 |
| Previous CABG, n (%) | 142 (2.2) | 255 (2.3) | 397 (2.3) | 0.64 |
| Killip classification, n (%) | 0.001 | |||
| I | 4,984 (77.7) | 8,381 (77.0) | 13,365 (77.3) | |
| II | 883 (13.8) | 1,432 (13.2) | 2,315 (13.4) | |
| III | 240 (3.7) | 388 (3.6) | 628 (3.6) | |
| IV | 311 (4.8) | 680 (6.2) | 991 (5.7) | |
PCI: percutaneous coronary intervention; CABG: coronary artery bypass graft surgery.
Angiographic characteristics.
| Predilation | ||||
|---|---|---|---|---|
| Characteristics | No (n = 6,508 patients, 7,988 lesions) | Yes (n = 11,007 patients, 12,096 lesions) | Total (n = 17,515 patients, 20,084 lesions) | p-value |
| CAD extension, n (%) | < 0.0001 | |||
| Single-vessel | 3,253 (51.5) | 4,933 (45.4) | 8,186 (47.6) | |
| Two-vessel | 1,861 (29.5) | 3,351 (30.8) | 5,212 (30.3) | |
| Three-vessel | 1,184 (18.8) | 2,552 (23.5) | 3,736 (21.7) | |
| Multivessel + LMCA | 3 (0) | 0 (0) | 3 (0) | |
| LMCA | 11 (0.2) | 32 (0.3) | 43 (0.3) | |
| Treated vessels, n (%) | 0.04 | |||
| Left anterior descending artery | 3,655 (45.8) | 5,706 (47.2) | 9,361 (46.6) | |
| Right coronary artery | 3,032 (38) | 4,551 (37.6) | 7,583 (37.8) | |
| Left circumflex artery | 1,124 (14.1) | 1,618 (13.4) | 2,742 (13.7) | |
| LMCA | 91 (1.1) | 96 (0.8) | 187 (0.9) | |
| Surgical grafting | 86 (1.1) | 126 (1.1) | 212 (1.1) | |
| B2/C lesions, n (%) | 1,523 (19.1) | 4,049 (33.5) | 5,572 (27.7) | < 0.0001 |
| Bifurcation lesions, n (%) | 1,747 (21.9) | 3,285 (27.2) | 5,032 (25.1) | < 0.0001 |
| TIMI flow, pre, n (%) | < 0.0001 | |||
| 0/1 | 4,496 (56.3) | 9,243 (76.4) | 13,739 (68.4) | |
| 2/3 | 3,492 (43.7) | 2,853 (23.6) | 6,345 (31.6) | |
| LVEF < 50%, n (%) | 3,019 (46.4) | 5,519 (50.1) | 8,538 (48.7) | < 0.0001 |
| Collateral circulation, n (%) | 662 (15.4) | 2,286 (25.3) | 2,948 (22.1) | < 0.0001 |
CAD: coronary atherosclerotic disease; LMCA: left main coronary artery; TIMI: Thrombolysis in Myocardial Infarction; LVEF: left ventricular ejection fraction.
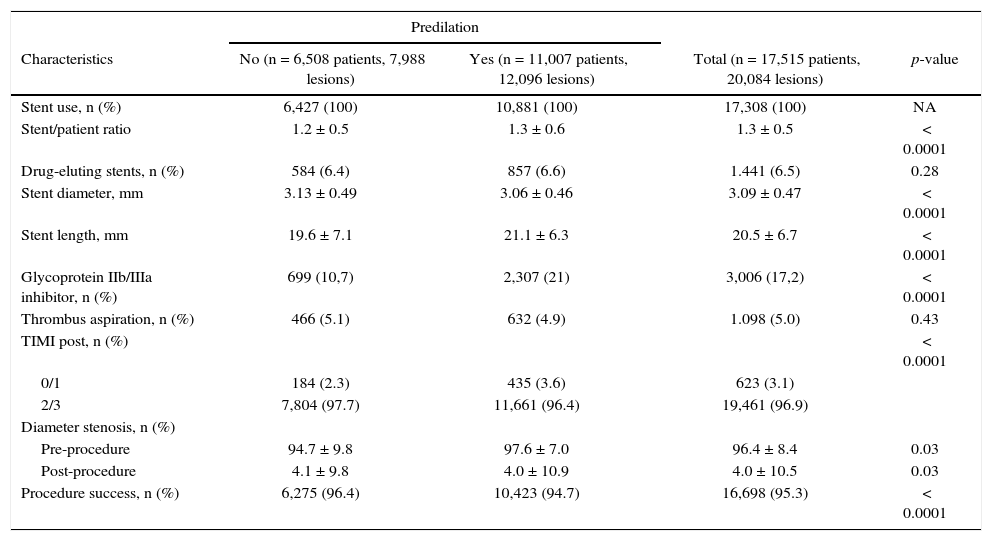
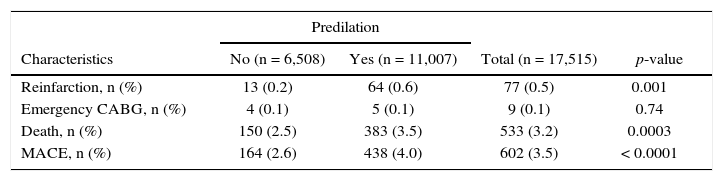
Stents were implanted in all procedures. The rates of intervention failure and use of glycoprotein IIb/IIIa inhibitors were higher among patients submitted to predilation (Table 3), as well as the rates of major adverse cardiac events at the expense of death and reinfarction (Table 4).
Characteristics of the procedures.
| Predilation | ||||
|---|---|---|---|---|
| Characteristics | No (n = 6,508 patients, 7,988 lesions) | Yes (n = 11,007 patients, 12,096 lesions) | Total (n = 17,515 patients, 20,084 lesions) | p-value |
| Stent use, n (%) | 6,427 (100) | 10,881 (100) | 17,308 (100) | NA |
| Stent/patient ratio | 1.2 ± 0.5 | 1.3 ± 0.6 | 1.3 ± 0.5 | < 0.0001 |
| Drug-eluting stents, n (%) | 584 (6.4) | 857 (6.6) | 1.441 (6.5) | 0.28 |
| Stent diameter, mm | 3.13 ± 0.49 | 3.06 ± 0.46 | 3.09 ± 0.47 | < 0.0001 |
| Stent length, mm | 19.6 ± 7.1 | 21.1 ± 6.3 | 20.5 ± 6.7 | < 0.0001 |
| Glycoprotein IIb/IIIa inhibitor, n (%) | 699 (10,7) | 2,307 (21) | 3,006 (17,2) | < 0.0001 |
| Thrombus aspiration, n (%) | 466 (5.1) | 632 (4.9) | 1.098 (5.0) | 0.43 |
| TIMI post, n (%) | < 0.0001 | |||
| 0/1 | 184 (2.3) | 435 (3.6) | 623 (3.1) | |
| 2/3 | 7,804 (97.7) | 11,661 (96.4) | 19,461 (96.9) | |
| Diameter stenosis, n (%) | ||||
| Pre-procedure | 94.7 ± 9.8 | 97.6 ± 7.0 | 96.4 ± 8.4 | 0.03 |
| Post-procedure | 4.1 ± 9.8 | 4.0 ± 10.9 | 4.0 ± 10.5 | 0.03 |
| Procedure success, n (%) | 6,275 (96.4) | 10,423 (94.7) | 16,698 (95.3) | < 0.0001 |
NA: not applicable; TIMI: Thrombolysis in Myocardial Infarction.
Clinical outcomes during the in-hospital phase.
| Predilation | ||||
|---|---|---|---|---|
| Characteristics | No (n = 6,508) | Yes (n = 11,007) | Total (n = 17,515) | p-value |
| Reinfarction, n (%) | 13 (0.2) | 64 (0.6) | 77 (0.5) | 0.001 |
| Emergency CABG, n (%) | 4 (0.1) | 5 (0.1) | 9 (0.1) | 0.74 |
| Death, n (%) | 150 (2.5) | 383 (3.5) | 533 (3.2) | 0.0003 |
| MACE, n (%) | 164 (2.6) | 438 (4.0) | 602 (3.5) | < 0.0001 |
CABG: coronary artery bypass graft surgery; MACE: major adverse cardiac events.
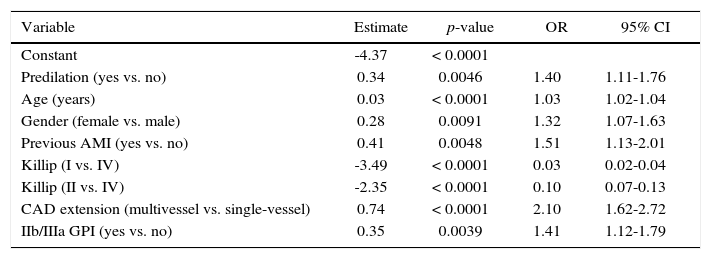
In the multiple logistic regression model, the variables that best correlated with the occurrence of death were predilation, advanced age, female gender, pre-existing coronary atherosclerotic disease, multivessel coronary artery disease, Killip classification, and use of glycoprotein IIb/IIIa inhibitors (Table 5).
Multiple logistic regression evaluating the influence of independent variables in relation to in-hospital death.
| Variable | Estimate | p-value | OR | 95% CI |
|---|---|---|---|---|
| Constant | -4.37 | < 0.0001 | ||
| Predilation (yes vs. no) | 0.34 | 0.0046 | 1.40 | 1.11-1.76 |
| Age (years) | 0.03 | < 0.0001 | 1.03 | 1.02-1.04 |
| Gender (female vs. male) | 0.28 | 0.0091 | 1.32 | 1.07-1.63 |
| Previous AMI (yes vs. no) | 0.41 | 0.0048 | 1.51 | 1.13-2.01 |
| Killip (I vs. IV) | -3.49 | < 0.0001 | 0.03 | 0.02-0.04 |
| Killip (II vs. IV) | -2.35 | < 0.0001 | 0.10 | 0.07-0.13 |
| CAD extension (multivessel vs. single-vessel) | 0.74 | < 0.0001 | 2.10 | 1.62-2.72 |
| IIb/IIIa GPI (yes vs. no) | 0.35 | 0.0039 | 1.41 | 1.12-1.79 |
OR: odds ratio; 95% CI: 95% confidence interval; AMI: acute myocardial infarction; CAD: coronary atherosclerotic disease; GPI: glycoprotein inhibitor.
The analysis of the CENIC database, which has national representativeness, shows that patients submitted to primary PCI requiring predilation have clinical, angiographic, and procedural characteristics that categorize them as having higher risk and technical complexity. Furthermore, it constitutes an independent predictor of in-hospital mortality. Similar findings have been reported in the literature. In the large, randomized, multicenter, HORIZONS-AMI (Harmonizing Outcomes With RevasculariZatiON and Stents in Acute Myocardial Infarction) study, involving 2,528 patients, direct stent implantation in patients eligible for the technique was associated with higher final epicardial flow rates – Thrombolysis in Myocardial Infarction (TIMI) 3, resolution of ST-elevation, and survival at 1 year of follow-up.10 The EUROTRANSFER (European Registry on STEMI Patients Transferred for PCI With Upstream Use of Abciximab) registry, which analyzed 1,143 patients, observed a significant reduction of 55% in 1-year mortality favorable to the group not requiring predilation, which was maintained even after adjustment by propensity score.11
The use of strategies aimed to minimize the risk of distal embolization and coronary flow impairment during primary PCI is an investigation hypothesis evaluated in different clinical trials. Manual or mechanical aspiration thrombectomy, distal protection filter, or delayed stent implantation were not shown to be effective in improving patients’ survival.12,13 Regarding direct stent implantation, a meta-analysis encompassing 12 studies and 9,331 patients, mostly observed a significant 44% reduction in mortality, suggesting this is a desirable technique when anatomically feasible.14
Although the absence of predilation can reduce the risk of periprocedural complications and adverse events, this intervention is technically associated to the presence of variables that allow its use.15,16 In fact, vessels greater than 2.5mm in diameter, absence of severe calcification, angulation greater than 45°, TIMI flow 0-1, and lesions involving bifurcations are characteristics that are more prevalent in the group submitted to direct stent implantation.17,18
Among the main limitations of the analysis, the authors highlight its observational, retrospective design, as well as the non-application of a propensity score for pairing and comparison between the groups. Additionally, in the CENIC registry, data is sent spontaneously, not including the total number of procedures performed in the period, although the high number of registered interventions (greater than 17,500) constitutes one of the largest series on the subject presented to date.
ConclusionsPrimary percutaneous coronary intervention requiring predilation was characterized by a higher prevalence of clinical comorbidities in patients and by angiographic and technical complexity of the procedures when compared to direct stent implantation. Predilation is an independent predictor of hospital mortality in this clinical setting.
Funding sourcesNone declared.
Conflicts of interestThe authors declare no conflicts of interest.
Peer review under the responsibility of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.