The epidemiology of acute myocardial infarction with ST-segment elevation (STEMI) has been modified in recent years, focusing on young people. Our goal was compare the clinical profile, laboratory, angiographic, and 30-day clinical outcomes of patients ≤ 40 years with those > 40 years undergoing primary percutaneous coronary intervention (pPCI).
MethodsProspective cohort study of consecutive patients undergoing pPCI between 2009 and 2011.
ResultsA total of 1,055 patients were included, 3.3% of them ≤ 40 years. Young patients were more often black, smokers and with a family history of coronary artery disease, and less often hypertensive and dyslipidemic. In patients ≤ 40 years, leukocyte count and ultrasensitive troponin levels at admission were higher, and high density lipoprotein-cholesterol, lower. The left anterior descending artery as a culprit vessel and left ventricular ejection fraction did not differ between groups. Although the TIMI 3 flow pre-intervention was similar, young people showed higher prevalence of myocardial blush 3 pre-procedure. The door-to-balloon time was lower in younger patients (1.0 hour [0.8-1.4 hour] vs. 1.3 hour [0.9-1.7 hour]; p = 0.03). At 30 days, patients ≤ 40 years had a mortality of 0% vs. 8.8% for patients > 40 years (p = 0.07).
ConclusionsPatients ≤ 40 years with STEMI and undergoing pPCI show differences in clinical, angiographic and procedural characteristics compared to those > 40 years. In this analysis, representative of the current medical practice, the 30-day mortality of these patients was very low.
A epidemiologia do infarto agudo do miocárdio com supradesnivelamento do segmento ST (IAMCST) tem se modificado nos últimos anos, com incidência maior em jovens. Nosso objetivo foi comparar o perfil clínico, laboratorial e angiográfico, e os desfechos clínicos em 30 dias de pacientes ≤ 40 anos àqueles > 40 anos submetidos à intervenção coronária percutânea primária (ICPp).
MétodosEstudo de coorte prospectivo com pacientes consecutivos submetidos à ICPp entre 2009 e 2011.
ResultadosNo período, 1.055 pacientes foram incluídos, sendo identificados 3,3% com ≤ 40 anos. Pacientes jovens eram mais frequentemente negros, tabagistas e com história familiar de doença coronária, e menos frequentemente hipertensos e dislipidêmicos. Nos pacientes ≤ 40 anos, a dosagem de leucócitos e da troponina ultrassensível na admissão foi maior, e a lipoproteína de alta densidade-colesterol, menor. A artéria descendente anterior como vaso culpado e a fração de ejeção do ventrículo esquerdo não foram diferentes entre os grupos. Apesar de o fluxo TIMI 3 pré ser similar, os jovens mostraram maior prevalência de blush miocárdico 3 pré-procedimento. O tempo porta-balão foi menor nos pacientes mais jovens (1,0 hora [0,8-1,4 hora] vs. 1,3 hora [0,9-1,7 hora]; p = 0,03). Em 30 dias, os pacientes ≤ 40 anos apresentaram mortalidade de 0% vs. 8,8% nos pacientes > 40 anos (p = 0,07).
ConclusõesPacientes ≤ 40 anos com IAMCST e submetidos à ICPp apresentam diferenças nos perfis clínico, angiográfico e do procedimento quando comparados àqueles > 40 anos. Nesta análise, representativa da prática médica atual, a mortalidade em 30 dias desses pacientes foi muito baixa.
Cardiovascular diseases are the leading cause of mortality in Brazil and worldwide. Acute myocardial infarction (AMI) is the cardiovascular disease with greatest mortality, and its incidence in young patients has increased over the years.1–3 Currently, the incidence in patients under 40 years is around 4%-10%.4–7In several studies, it was observed that myocardial infarction in young patients is most often associated with smoking, family his-tory of coronary artery disease, and dyslipidemia.4,5,7,8 However, there are few Brazilian studies evaluating this question.
The objective of this study was to evaluate the clinical and angiographic characteristics as well as the clinical outcome for young patients with ST-segment elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention (pPCI) in contemporary clinical practice.
MethodsPatientsAll patients diagnosed with AMI admitted to this institution from December 1st, 2009 to December 31st, 2011 were prospectively evaluated. Inclusion criteria were clinical and electrocardiographic diagnosis of myocardial infarction, and indication for pPCI by the attending physician. Exclusion criteria were Dt > 12hours, age < 18 years, and refusal to sign the informed consent.
STEMI was defined as the presence of a typical pain at rest associated to ST-segment elevation in two contiguous leads of at least 1mm in the frontal plane or 2mm in the horizontal plane, or the presence of a typical chest pain at rest in patients with a new left bundle branch block.
Patients were categorized into two groups: patients aged ≤ 40 years and controls (> 40 years). The clinical characteristics and outcomes were compared. The study was approved by the Ethics Committee of this institution.
Percutaneous procedureThe Hemodynamics Service of this institution operates full-time, 24hours a day, 7 days a week. Approximately 500 pPCI procedures are performed annually. The institutional routine is an acetylsalicylic acid loading dose of 300mg and clopidogrel 300-600mg at admission to emergency department and heparin 60-100 U/kg. pPCI procedures are performed as described in the literature.9 Specific technical aspects, such as access route, drug administration, type of stent, and thromboaspiration, are at operators’ discretion.
Clinical, laboratory, and angiographic evaluationThe clinical interview was conducted by trained researchers. Demographics, risk factors for ischemic heart disease, medical history, and clinical presentation of the event data were collected. Laboratory tests were conducted according to the institutional criteria and included, among others, serum glucose concentration, renal function, and inflammation and myocardial necrosis markers.
Angiographic evaluations were performed by a digital electronic system AXIOM Artis (Siemens, Munich, Germany). Target vessel reference diameter was defined as the average of proximal and distal diameters from the lesion, and stenosis severity was evaluated in two orthogonal projections; the most severe was considered, both before and after stent implantation. The lesion length was measured shoulder-to-shoulder and lesions with a normal arterial segment < 10mm between them were considered as a single lesion. The coronary flow before and after the procedure was evaluated and described according to Thrombolysis In Myocardial Infarction (TIMI) criteria. Myocardial perfusion was assessed by myocardial blush, as previously described.10
30-day clinical outcomesThe 30-day follow-up was conducted by phone, and occurrences of death, stroke, reinfarction, need for a new percutaneous or surgical revascularization, and/or stent thrombosis were registered.
Statistical analysisSPSS version 17.0 for Windows was used for statistical analysis. Continuous variables were presented as mean and standard deviation, and compared using Student's t-test. Continuous variables with non-normal distribution were described as median and interquartile range and compared using the Mann-Whitney test. Categorical variables were described as absolute number and percentage and compared by the Chi-squared test or Fisher's exact test, as appropriate. Statistical significance was defined by a two-tailed p-value < 0.05.
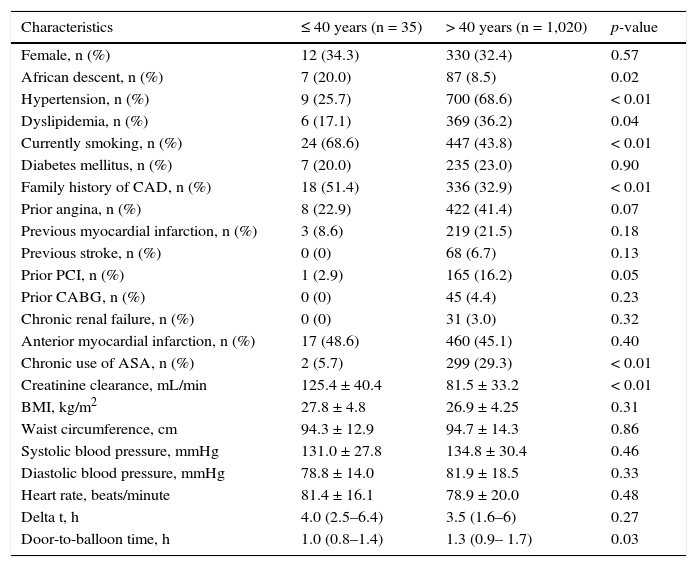
ResultsDuring the study period, 1,055 patients were included, of whom 35 (3.3%) were aged ≤ 40 years. The mean age of young patients was 34.1 ± 4.5 years and 61.3 ± 11.1 years for those aged > 40 years. Table 1 shows the clinical characteristics of both groups. African descent, smoking, and family history of premature coronary artery disease were more frequent among patients ≤ 40 years. On the contrary, younger patients were less frequently affected by hypertension or dyslipidemia, and this group had lower rates of previous percutaneous revascularization. The prevalence of diabetes mellitus was similar. The door-to-balloon time was lower in patients aged ≤ 40 years (1.0h [0.8-1.4h] vs. 1.3h [0.9–1.7h]; p = 0.03).
Clinical characteristics.
| Characteristics | ≤ 40 years (n = 35) | > 40 years (n = 1,020) | p-value |
|---|---|---|---|
| Female, n (%) | 12 (34.3) | 330 (32.4) | 0.57 |
| African descent, n (%) | 7 (20.0) | 87 (8.5) | 0.02 |
| Hypertension, n (%) | 9 (25.7) | 700 (68.6) | < 0.01 |
| Dyslipidemia, n (%) | 6 (17.1) | 369 (36.2) | 0.04 |
| Currently smoking, n (%) | 24 (68.6) | 447 (43.8) | < 0.01 |
| Diabetes mellitus, n (%) | 7 (20.0) | 235 (23.0) | 0.90 |
| Family history of CAD, n (%) | 18 (51.4) | 336 (32.9) | < 0.01 |
| Prior angina, n (%) | 8 (22.9) | 422 (41.4) | 0.07 |
| Previous myocardial infarction, n (%) | 3 (8.6) | 219 (21.5) | 0.18 |
| Previous stroke, n (%) | 0 (0) | 68 (6.7) | 0.13 |
| Prior PCI, n (%) | 1 (2.9) | 165 (16.2) | 0.05 |
| Prior CABG, n (%) | 0 (0) | 45 (4.4) | 0.23 |
| Chronic renal failure, n (%) | 0 (0) | 31 (3.0) | 0.32 |
| Anterior myocardial infarction, n (%) | 17 (48.6) | 460 (45.1) | 0.40 |
| Chronic use of ASA, n (%) | 2 (5.7) | 299 (29.3) | < 0.01 |
| Creatinine clearance, mL/min | 125.4 ± 40.4 | 81.5 ± 33.2 | < 0.01 |
| BMI, kg/m2 | 27.8 ± 4.8 | 26.9 ± 4.25 | 0.31 |
| Waist circumference, cm | 94.3 ± 12.9 | 94.7 ± 14.3 | 0.86 |
| Systolic blood pressure, mmHg | 131.0 ± 27.8 | 134.8 ± 30.4 | 0.46 |
| Diastolic blood pressure, mmHg | 78.8 ± 14.0 | 81.9 ± 18.5 | 0.33 |
| Heart rate, beats/minute | 81.4 ± 16.1 | 78.9 ± 20.0 | 0.48 |
| Delta t, h | 4.0 (2.5–6.4) | 3.5 (1.6–6) | 0.27 |
| Door-to-balloon time, h | 1.0 (0.8–1.4) | 1.3 (0.9– 1.7) | 0.03 |
CAD: coronary artery disease; PCI: percutaneous coronary intervention; CABG: coronary artery bypass graft; ASA: acetylsalicylic acid.
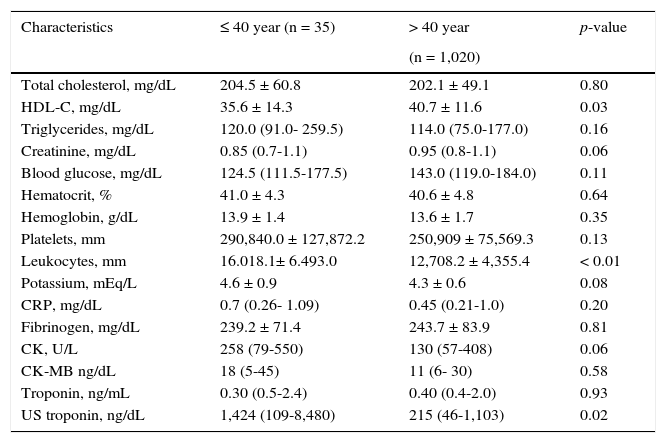
Table 2 describes laboratory characteristics of each group. In patients aged ≤ 40 years, the leukocyte count and ultrasensitive troponin level at admission were higher, and the high-density lipoprotein cholesterol (HDL-C) level was lower. There was no significant difference in other markers of myocardial necrosis or inflammation between groups.
Laboratory characteristics.
| Characteristics | ≤ 40 year (n = 35) | > 40 year | p-value |
|---|---|---|---|
| (n = 1,020) | |||
| Total cholesterol, mg/dL | 204.5 ± 60.8 | 202.1 ± 49.1 | 0.80 |
| HDL-C, mg/dL | 35.6 ± 14.3 | 40.7 ± 11.6 | 0.03 |
| Triglycerides, mg/dL | 120.0 (91.0- 259.5) | 114.0 (75.0-177.0) | 0.16 |
| Creatinine, mg/dL | 0.85 (0.7-1.1) | 0.95 (0.8-1.1) | 0.06 |
| Blood glucose, mg/dL | 124.5 (111.5-177.5) | 143.0 (119.0-184.0) | 0.11 |
| Hematocrit, % | 41.0 ± 4.3 | 40.6 ± 4.8 | 0.64 |
| Hemoglobin, g/dL | 13.9 ± 1.4 | 13.6 ± 1.7 | 0.35 |
| Platelets, mm | 290,840.0 ± 127,872.2 | 250,909 ± 75,569.3 | 0.13 |
| Leukocytes, mm | 16.018.1± 6.493.0 | 12,708.2 ± 4,355.4 | < 0.01 |
| Potassium, mEq/L | 4.6 ± 0.9 | 4.3 ± 0.6 | 0.08 |
| CRP, mg/dL | 0.7 (0.26- 1.09) | 0.45 (0.21-1.0) | 0.20 |
| Fibrinogen, mg/dL | 239.2 ± 71.4 | 243.7 ± 83.9 | 0.81 |
| CK, U/L | 258 (79-550) | 130 (57-408) | 0.06 |
| CK-MB ng/dL | 18 (5-45) | 11 (6- 30) | 0.58 |
| Troponin, ng/mL | 0.30 (0.5-2.4) | 0.40 (0.4-2.0) | 0.93 |
| US troponin, ng/dL | 1,424 (109-8,480) | 215 (46-1,103) | 0.02 |
HDL-C: high-density lipoprotein cholesterol; CRP: C-reactive protein; CK: creatine phosphokinase; CK-MB: creatine kinase-MB isoenzyme; US: ultrasensitive.
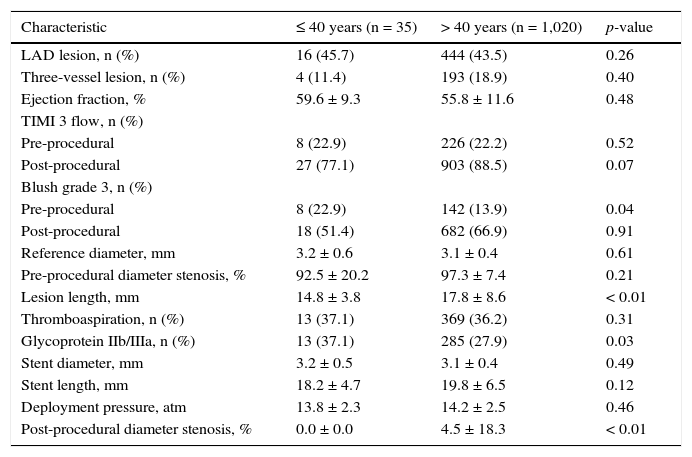
Table 3 shows angiographic and procedural characteristics; note that three-vessel involvement, left anterior descending artery as the culprit vessel, and left ventricular ejection fraction did not differ between groups. Although there was equivalence of pre-procedural TIMI-3 flows, the younger group had a higher prevalence of grade 3 myocardial blush before the procedure. The reference diameter was similar, but younger patients showed shorter lesions. The use of glycoprotein IIb/IIIa inhibitors was higher among young patients.
Angiographic and procedural characteristics.
| Characteristic | ≤ 40 years (n = 35) | > 40 years (n = 1,020) | p-value |
|---|---|---|---|
| LAD lesion, n (%) | 16 (45.7) | 444 (43.5) | 0.26 |
| Three-vessel lesion, n (%) | 4 (11.4) | 193 (18.9) | 0.40 |
| Ejection fraction, % | 59.6 ± 9.3 | 55.8 ± 11.6 | 0.48 |
| TIMI 3 flow, n (%) | |||
| Pre-procedural | 8 (22.9) | 226 (22.2) | 0.52 |
| Post-procedural | 27 (77.1) | 903 (88.5) | 0.07 |
| Blush grade 3, n (%) | |||
| Pre-procedural | 8 (22.9) | 142 (13.9) | 0.04 |
| Post-procedural | 18 (51.4) | 682 (66.9) | 0.91 |
| Reference diameter, mm | 3.2 ± 0.6 | 3.1 ± 0.4 | 0.61 |
| Pre-procedural diameter stenosis, % | 92.5 ± 20.2 | 97.3 ± 7.4 | 0.21 |
| Lesion length, mm | 14.8 ± 3.8 | 17.8 ± 8.6 | < 0.01 |
| Thromboaspiration, n (%) | 13 (37.1) | 369 (36.2) | 0.31 |
| Glycoprotein IIb/IIIa, n (%) | 13 (37.1) | 285 (27.9) | 0.03 |
| Stent diameter, mm | 3.2 ± 0.5 | 3.1 ± 0.4 | 0.49 |
| Stent length, mm | 18.2 ± 4.7 | 19.8 ± 6.5 | 0.12 |
| Deployment pressure, atm | 13.8 ± 2.3 | 14.2 ± 2.5 | 0.46 |
| Post-procedural diameter stenosis, % | 0.0 ± 0.0 | 4.5 ± 18.3 | < 0.01 |
LAD: left anterior descendent coronary.
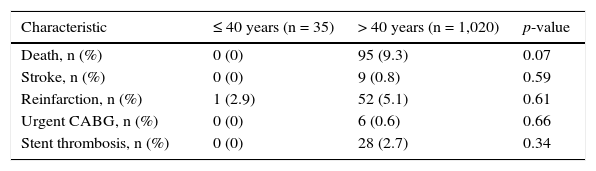
During hospitalization, there were no differences between groups as to the need for mechanical ventilation (8.6% vs. 9.3%; p = 0.98), acute renal failure (5.7% vs. 4.1%, p = 0.54), or sepsis (2.9% vs. 3.6%, p = 0.88). In patients aged ≤ 40 years, no clinical events, except for reinfarction (2.9% vs. 5.1%, p = 0.61), occurred in the first 30 days (Table 4).
Clinical outcomes in 30 days.
| Characteristic | ≤ 40 years (n = 35) | > 40 years (n = 1,020) | p-value |
|---|---|---|---|
| Death, n (%) | 0 (0) | 95 (9.3) | 0.07 |
| Stroke, n (%) | 0 (0) | 9 (0.8) | 0.59 |
| Reinfarction, n (%) | 1 (2.9) | 52 (5.1) | 0.61 |
| Urgent CABG, n (%) | 0 (0) | 6 (0.6) | 0.66 |
| Stent thrombosis, n (%) | 0 (0) | 28 (2.7) | 0.34 |
CABG: coronary artery bypass graft.
This study analyzed the clinical and angiographic profiles and clinical outcomes of patients ≤ 40 years of age who had STEMI in a tertiary cardiology center. Among younger patients, African descent, smoking, and family history of ischemic heart disease were more frequent, but no difference for diabetes mellitus frequency was noted. Younger patients had other comorbidities and multivessel disease less often and there was a trend for a better clinical outcome after 30 days in this group. In Brazil, contemporary studies analyzing the clinical characteristics of young patients with AMI are few,1,2,11 and it is believed that the data presented here can contribute to the development of public health policies and prevention campaigns.
This study showed high prevalence of smoking in younger patients with AMI (around 70%), which is consistent with reports from other studies that included patients with the same age group. This association has been identified in most published studies, with a prevalence of 65% to 95%.5,12–18 Smoking plays an important role in the genesis, progression and destabilization of atherosclerotic plaques, and its specific association with younger patients is important and deserves further evaluation.
A significantly higher frequency of a positive family history of ischemic heart disease in young patients analyzed in this study represents another important aspect. Family history is also a classic risk factor for ischemic heart disease, and the data presented in this study are also consistent with other reports in the literature.19–21 The influence of a genetic factor and its greater association in this age group are other important aspects, considering the pathophysiology and possible predisposing factors for AMI in patients ≤ 40 years of age.
Among younger patients, African descent was more frequent vs. patients over 40 years. This finding has not been described in previous studies evaluating patients with STEMI in this age group. The influence of genetic traits or associations among socioeconomic and cultural factors, the adherence to medications, and lifestyle could explain these findings, and deserve to be better evaluated in Brazilian populations.
The diagnosis of dyslipidemia was less common in younger patients, but they had lower HDL-C levels vs. older patients. Kaukola et al.22 also showed similar values for total cholesterol in younger patients and in those over 40 years, but with HDL values slightly lower in younger patients, with a slightly higher triglyceride level in this group. A low level of HDL has been associated with acute myocardial infarction in young patients.23 Some studies indicated only high cholesterol level as a risk factor,5,17,24,25 but the establishment of an association with other laboratory findings is essential, in order to prevent diseases in this age group. An association between dyslipidemia and AMI at an early age has been documented in other studies.12
In the present study, the early clinical outcome of younger patients was better vs. patients over 40 years, although without statistical significance. These findings are also consistent with most studies, which pointed to a lower incidence of adverse outcomes in young patients, and this could be due to a better capacity for regeneration and of response to injury and to a lower association with comorbidities.4,5,8
ConclusionsThe frequency of acute myocardial infarction with ST-segment elevation in patients ≤ 40 years of age is small, but these patients have different clinical and laboratory characteristics and early clinical outcomes vs. older patients. Population studies, with larger numbers of patients in Brazil, are important for a better understanding of this problem, as well as to guide prevention and public health campaigns.
Funding sourcesConselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), through a scientific initiation grant for the author Karine Elisa Schmidt.
Conflicts of interestThe authors declare no conflicts of interest.