Invasive coronary procedures are common in patients with previous coronary artery bypass graft surgery. Data on the actual role and possible limitations of the radial approach in this subgroup of patients are sparse. The objective of this study was to evaluate the feasibility and safety of radial access in patients surgically revascularized and who underwent subsequent invasive diagnostic or therapeutic coronary procedures, comparing it to the femoral access.
MethodsBetween May 2008 and November 2014, 959 procedures were included; 539 performed by radial access and 420 by femoral access. All operators were familiar with both vascular accesses, and the final decision on the route to be used was left to the operators discretion.
ResultsThe failure rate was 6.1% vs. 0.5% (p < 0.0001), favoring the femoral approach. Major adverse cardiac events (0.4% vs. 0.7%) and vascular complications (1.5% vs. 1.9%) rates were low, with no difference between groups. The choice of the radial approach resulted in greater fluoroscopy time and crossover rate between access routes, especially in diagnostic procedures.
ConclusionsThe radial approach was a safe and effective option for invasive coronary procedures in post- coronary artery bypass graft patients, especially for therapeutic procedures.
Procedimentos coronários invasivos são comuns em pacientes com revascularização miocárdica cirúrgica prévia. Dados acerca do real papel e das possíveis limitações do acesso radial nesse subgrupo de pacientes são infrequentes. O objetivo deste estudo foi avaliar a factibilidade e a segurança do acesso radial em pacientes revascularizados cirurgicamente e que foram submetidos a procedimentos coronários invasivos diagnósticos ou terapêuticos subsequentes, comparando-o ao acesso femoral.
MétodosEntre maio de 2008 e novembro de 2014, foram analisados 959 procedimentos, sendo 539 realizados pelo acesso radial e 420 pelo femoral. Todos os operadores estavam familiarizados com ambos os acessos vasculares, cabendo a eles a decisão final sobre a via a ser utilizada.
ResultadosA prevalência de insucesso foi de 6,1% vs. 0,5% (p < 0,0001), favorecendo a técnica femoral. As taxas de eventos cardíacos adversos graves (0,4% vs. 0,7%) e de complicações vasculares (1,5% vs. 1,9%) foram baixas, sem diferença entre os grupos. A opção pela técnica radial implicou em maior tempo de fluoroscopia e necessidade de cruzamento entre vias de acesso, principalmente em procedimentos diagnósticos.
ConclusõesO acesso radial representou uma opção segura e eficaz para a realização de procedimentos coronários invasivos em pacientes cirurgicamente revascularizados, notadamente para os procedimentos terapêuticos.
Invasive coronary procedures are common in patients with a history of coronary artery bypass graft surgery (CABG), traditionally performed via femoral access. However, the radial technique has progressively gained wide acceptance because of its effectiveness in reducing vascular complications, with a potential prognostic impact, as well as offering earlier ambulation and/or hospital discharge.1–3
However, studies on the actual role and possible limitations of the radial approach in patients with a history of CABG are infrequent, since this represents a high-risk subgroup with diffuse atherosclerosis and complex lesions, and is usually excluded or poorly represented in comparative studies between access routes.4,5
This analysis aimed to evaluate the feasibility and safety of the radial approach in patients with history of CABG who underwent subsequent invasive diagnostic or therapeutic coronary procedures, comparing it to the femoral approach, with emphasis on technical aspects such as the need for crossover, procedure duration, fluoroscopy time, number of catheters used, and vascular complications.
MethodsStudy populationThis study retrospectively reviewed all patients with history of CABG referred for invasive coronary diagnostic or therapeutic procedures in the period between May 2008 and November 2014, in a single center. All surgeons were familiar with both vascular accesses, and the final decision regarding approach was left to their discretion.
ProceduresThe radial artery was punctured with a 20-22 Jelco catheter using the Seldinger technique or a modified Seldinger technique, using a short hydrophilic-coated 5F or 6F sheath. A solution containing 5,000 IU of unfractionated heparin (UFH) and 10mg of isosorbide mononitrate was administered through an extension of the sheath, and the UFH dose was complemented to 100 IU/kg in the case of a percutaneous coronary intervention (PCI). At the end of the procedure, the sheath was immediately removed, and hemostasis was performed with a pressure dressing (a porous elastic adhesive bandage in diagnostic tests or a selective compressive bracelet in therapeutic interventions). Allen's test was not routinely performed.
After a subcutaneous infiltration with 15-20mL of 2% xylocaine, the femoral artery was punctured below the inguinal ligament with an 18G needle, using the modified Seldinger technique, with insertion of a 5F or 6F sheath. 2,500 IU of UFH were administered through the sheath extension, and the dose was complemented to 100 IU/kg in the case of PCI. Hemostasis was obtained by manual compression 2hours after the procedure, or in case of an activated clotting time < 180seconds.
Coronary angiography was performed by Judkins technique, using preformed catheters for selective cannulation of coronary arteries and surgical grafts. A pigtail catheter was systematically used for left ventriculography in femoral access, but not in radial access; in the latter case, a Tiger, Judkins right, or multipurpose catheter was preferably used, to avoid excessive handling and arterial spasm.
Outcomes and definitionsThe effectiveness of the study techniques was evaluated by the success rate of the procedure, defined as the completion of a coronary angiography and left ventriculography with adequate coronary and graft opacification; or, with respect to therapeutic interventions, obtaining a residual lesion < 20%, with no need to change the access port. The duration of the procedure and the fluoroscopy time were measured from the beginning of the arterial puncture to the removal of the last catheter.
Procedural safety was evaluated by the incidence of vascular complications related to the puncture site, including severe bleeding, hematoma > 5cm, arteriovenous fistula, pseudoaneurysm, arterial occlusion, or the need for a reconstructive vascular surgery. Bleedings of type 3 or 5 were classified as severe events, according to the definition of the Bleeding Academic Research Consortium.6
Statistical analysisThe qualitative variables were summarized in absolute frequencies and percentages. Quantitative data were expressed as means ± standard deviations or medians (25th percentile – 75th percentile), according to the distribution of each variable. Comparisons between groups were performed through the Chi-squared test or Fisher's exact test for qualitative variables and Student's t-test or the Mann-Whitney test for quantitative variables. Results with p < 0.05 were considered statistically significant.
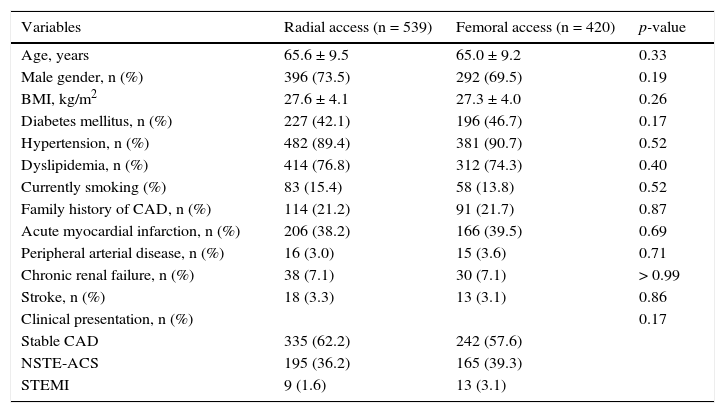
ResultsAmong 13,579 procedures performed, 959 (7.1%) involved patients with previous CABG; of these, 539 (56.2%) were performed by radial, and 420 (43.8%) by femoral access. Baseline clinical characteristics did not differ between groups and are summarized in Table 1. In this population, the high rates of comorbidities are noteworthy, such as diabetes mellitus, hypertension, dyslipidemia, and prior myocardial infarction. Stable coronary atherosclerosis was the predominant clinical presentation.
Baseline clinical characteristics.
| Variables | Radial access (n = 539) | Femoral access (n = 420) | p-value |
|---|---|---|---|
| Age, years | 65.6 ± 9.5 | 65.0 ± 9.2 | 0.33 |
| Male gender, n (%) | 396 (73.5) | 292 (69.5) | 0.19 |
| BMI, kg/m2 | 27.6 ± 4.1 | 27.3 ± 4.0 | 0.26 |
| Diabetes mellitus, n (%) | 227 (42.1) | 196 (46.7) | 0.17 |
| Hypertension, n (%) | 482 (89.4) | 381 (90.7) | 0.52 |
| Dyslipidemia, n (%) | 414 (76.8) | 312 (74.3) | 0.40 |
| Currently smoking (%) | 83 (15.4) | 58 (13.8) | 0.52 |
| Family history of CAD, n (%) | 114 (21.2) | 91 (21.7) | 0.87 |
| Acute myocardial infarction, n (%) | 206 (38.2) | 166 (39.5) | 0.69 |
| Peripheral arterial disease, n (%) | 16 (3.0) | 15 (3.6) | 0.71 |
| Chronic renal failure, n (%) | 38 (7.1) | 30 (7.1) | > 0.99 |
| Stroke, n (%) | 18 (3.3) | 13 (3.1) | 0.86 |
| Clinical presentation, n (%) | 0.17 | ||
| Stable CAD | 335 (62.2) | 242 (57.6) | |
| NSTE-ACS | 195 (36.2) | 165 (39.3) | |
| STEMI | 9 (1.6) | 13 (3.1) |
CAD: coronary artery disease; NSTE-ACS: non-ST-segment elevation acute coronary syndrome; STEMI: ST-segment elevation myocardial infarction.
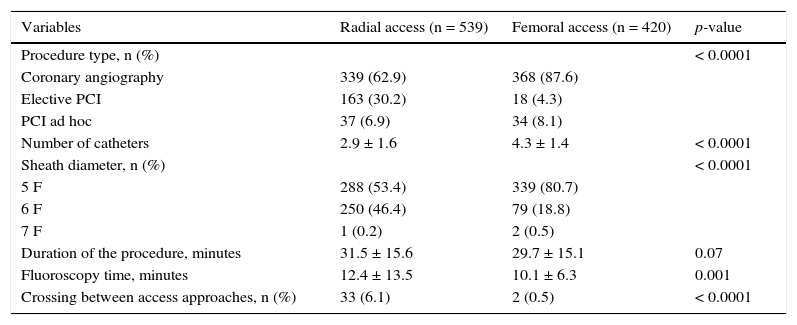
Diagnostic procedures accounted for 73.7% of the total, and were more commonly performed by femoral approach (Table 2). Elective percutaneous coronary interventions constituted 18.9% of the sample, and in these events the use of radial access prevailed. The overall failure rate was 6.1% vs. 0.5% (p < 0.0001) favoring the femoral technique. During hospitalization, serious adverse cardiac events occurred in two patients (0.4%) of the radial group and in three (0.7%) of the femoral group, with no statistically significant difference (p = 0.66). The prevalence of vascular complications was low and did not differ between groups (1.5 vs. 1.9%; p = 0.62).
Characteristics of procedures.
| Variables | Radial access (n = 539) | Femoral access (n = 420) | p-value |
|---|---|---|---|
| Procedure type, n (%) | < 0.0001 | ||
| Coronary angiography | 339 (62.9) | 368 (87.6) | |
| Elective PCI | 163 (30.2) | 18 (4.3) | |
| PCI ad hoc | 37 (6.9) | 34 (8.1) | |
| Number of catheters | 2.9 ± 1.6 | 4.3 ± 1.4 | < 0.0001 |
| Sheath diameter, n (%) | < 0.0001 | ||
| 5 F | 288 (53.4) | 339 (80.7) | |
| 6 F | 250 (46.4) | 79 (18.8) | |
| 7 F | 1 (0.2) | 2 (0.5) | |
| Duration of the procedure, minutes | 31.5 ± 15.6 | 29.7 ± 15.1 | 0.07 |
| Fluoroscopy time, minutes | 12.4 ± 13.5 | 10.1 ± 6.3 | 0.001 |
| Crossing between access approaches, n (%) | 33 (6.1) | 2 (0.5) | < 0.0001 |
PCI: percutaneous coronary intervention.
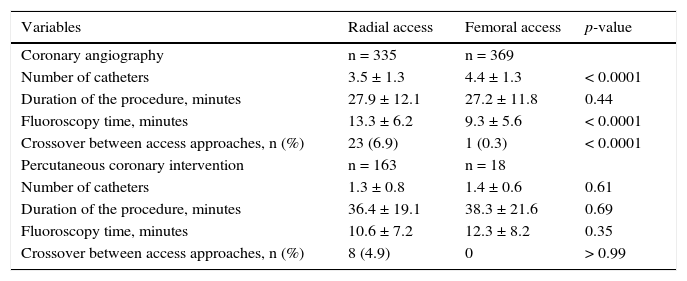
Table 3 illustrates the differences in procedure duration, fluoroscopy time, number of catheters used, and failure rate, stratified according to the type of procedure performed. The choice of the radial technique in diagnostic catheterizations was associated with a greater fluoroscopy time and need for crossover compared to the femoral technique, and such findings were attenuated in the therapeutic interventions.
Technical characteristics according to type of procedure performed.
| Variables | Radial access | Femoral access | p-value |
|---|---|---|---|
| Coronary angiography | n = 335 | n = 369 | |
| Number of catheters | 3.5 ± 1.3 | 4.4 ± 1.3 | < 0.0001 |
| Duration of the procedure, minutes | 27.9 ± 12.1 | 27.2 ± 11.8 | 0.44 |
| Fluoroscopy time, minutes | 13.3 ± 6.2 | 9.3 ± 5.6 | < 0.0001 |
| Crossover between access approaches, n (%) | 23 (6.9) | 1 (0.3) | < 0.0001 |
| Percutaneous coronary intervention | n = 163 | n = 18 | |
| Number of catheters | 1.3 ± 0.8 | 1.4 ± 0.6 | 0.61 |
| Duration of the procedure, minutes | 36.4 ± 19.1 | 38.3 ± 21.6 | 0.69 |
| Fluoroscopy time, minutes | 10.6 ± 7.2 | 12.3 ± 8.2 | 0.35 |
| Crossover between access approaches, n (%) | 8 (4.9) | 0 | > 0.99 |
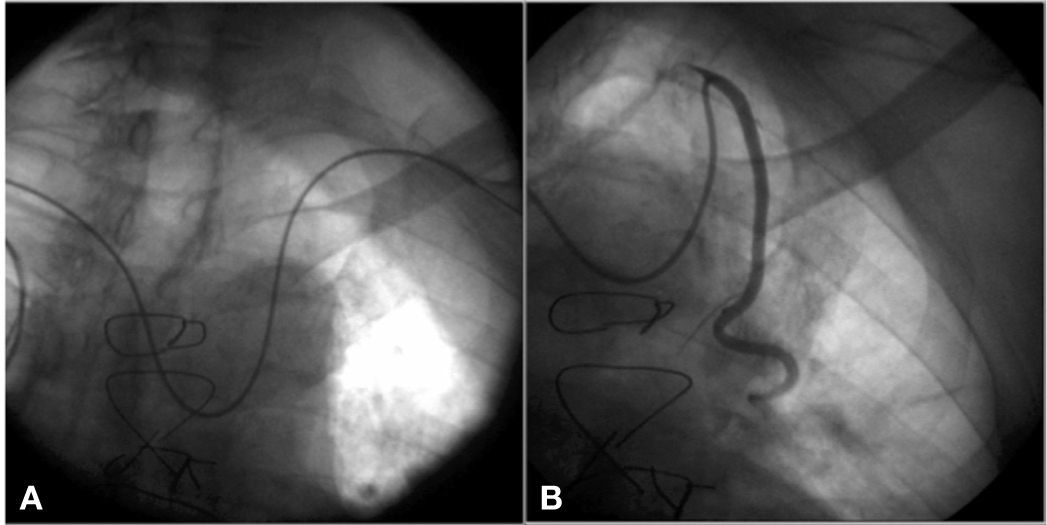
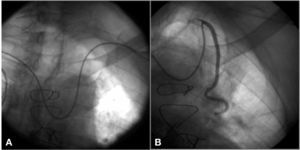
Eight patients with left internal mammary artery (LIMA) anastomosis for left anterior descending artery underwent diagnostic catheterization through the right radial access (Fig. 1). The selective cannulation of the LIMA was feasible, using a Simmons catheter for placement of a 260cm long, 0.35-inch guidewire in the left subclavian artery and with subsequent exchange by a mammary guide catheter; however, this procedure was associated with high fluoroscopy times (19.3 ± 6.4minutes) and total duration of the procedure (46.3 ± 11.3minutes).
DiscussionWith a comparative analysis of data from 959 invasive coronary procedures performed in patients with history of CABG in a center that favors the radial technique as its first vascular access option, it was established that the femoral approach remains the most used technique in this subgroup of patients for diagnostic catheterizations (52.1% vs. 47.9%), providing a venue for the radial technique with respect to percutaneous coronary interventions (90.1% vs 9.9%) at the expense of a significant increase in fluoroscopy time and need for crossover. This analysis also showed that, in the contemporary practice of a reference service, the rate of vascular complications is low, regardless of the technique used.
In the randomized trial Radial versus Femoral Access for Coronary Artery Bypass Graft Angiography and Intervention (RADIAL-CABG), involving 128 patients, the use of the radial access was associated with more consumption of contrast and higher numbers of catheters, procedure duration, surgeon's exposure to radiation, and the need for crossover (17.2 vs. 0.0%; p < 0.01).7
The high failure rate with the use of the radial technique could be justified due to its undertaking by less experienced surgeons, and the other findings are consistent with those observed in the present study. The exception would be the larger number of catheters in the femoral group, justified by the additional use of the pigtail catheter in procedures conducted by this route. However, the higher proportion of 6F catheters in the radial group is explained by the choice of this route in 90.1% of all percutaneous coronary interventions in the sample.
Previous CABG surgery is a recognized variable predictive of radial technique failure, as are age and female gender.8 In fact, this represents a subgroup of patients requiring care in the selection of the access, given the propensity to radial spasm due to excessive handling and frequent exchange of catheters, the difficulty of selective cannulation of grafts and of obtaining an adequate support, the need to use the left radial artery owing to the prevalence of anastomoses involving the LIMA, and to surgeries with the use of double mammary or of an ipsilateral radial graft, which makes this process more challenging. Although feasible, as demonstrated in this registry, the cannulation of the LIMA through the contralateral radial access will encounter difficulties inherent to the angulations and tortuosity often found; therefore, this option should be reserved for exceptional situations.9
Thus, the radial technique in patients previously treated by CABG would not represent the first choice for interventional cardiologists in the beginning of the learning curve, but this option can be integrated gradually into their routine as experience is being gained, until high success rates with low complication rates are achieved.10 Compliance with aspects such as knowledge of the number and type of grafts, the use of the radial access ipsilateral to the internal mammary graft, and the appropriate selection of the catheter to obtain an adequate support are important steps to be achieved in this process.11 Currently, the identification of situations in which the reduction of vascular complications and the comfort afforded to the patient outweigh the increased fluoroscopy time, and hence the radiological exposure, as well as the higher failure rate, are subject to debate and require individualization of cases.
LimitationsThe main limitation of this study was its non-random design. The choice of the vascular access was left to the operator's discretion, who, though accustomed to the radial technique, were in different stages of experience, which could explain the high percentage of failure observed. The absence of information on the average number and type of grafts used by each group, the total volume of contrast, the level of radiation exposure, and the causes of failure accounted for other important limitations. Nonetheless, this study had a large sample representative of the reality of a reference center for the radial access route. Care should be taken in generalizing these findings.
ConclusionsThe radial approach is a safe and effective option for invasive coronary procedures in patients with history of coronary artery bypass graft surgery, especially with respect to percutaneous interventions. When compared to femoral access, the radial approach is associated with a significant increase in fluoroscopy time and in technical failure rates.
Funding sourcesNone declared.
Conflicts of interestThe authors declare no conflicts of interest.
Peer Review under the responsability of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.