The treatment of coronary bifurcation lesions with single stenting in the main vessel and provisional side branch stenting may be limited by the degree of anatomical/morphological complexity. Side branch predilation, a procedural step that is typically avoided, may be required to maintain side branch patency. The impact of side branch predilation on the immediate results of percutaneous coronary intervention in complex coronary bifurcation lesions was investigated.
MethodsBetween May, 2008 and August, 2009, 59 patients with single coronary bifurcation lesions and significant involvement of the main and side branches were included in the study. The main exclusion criteria were the involvement of the left main coronary artery, ST-elevation acute myocardial infarction (< 72 hours) and in-stent restenosis.
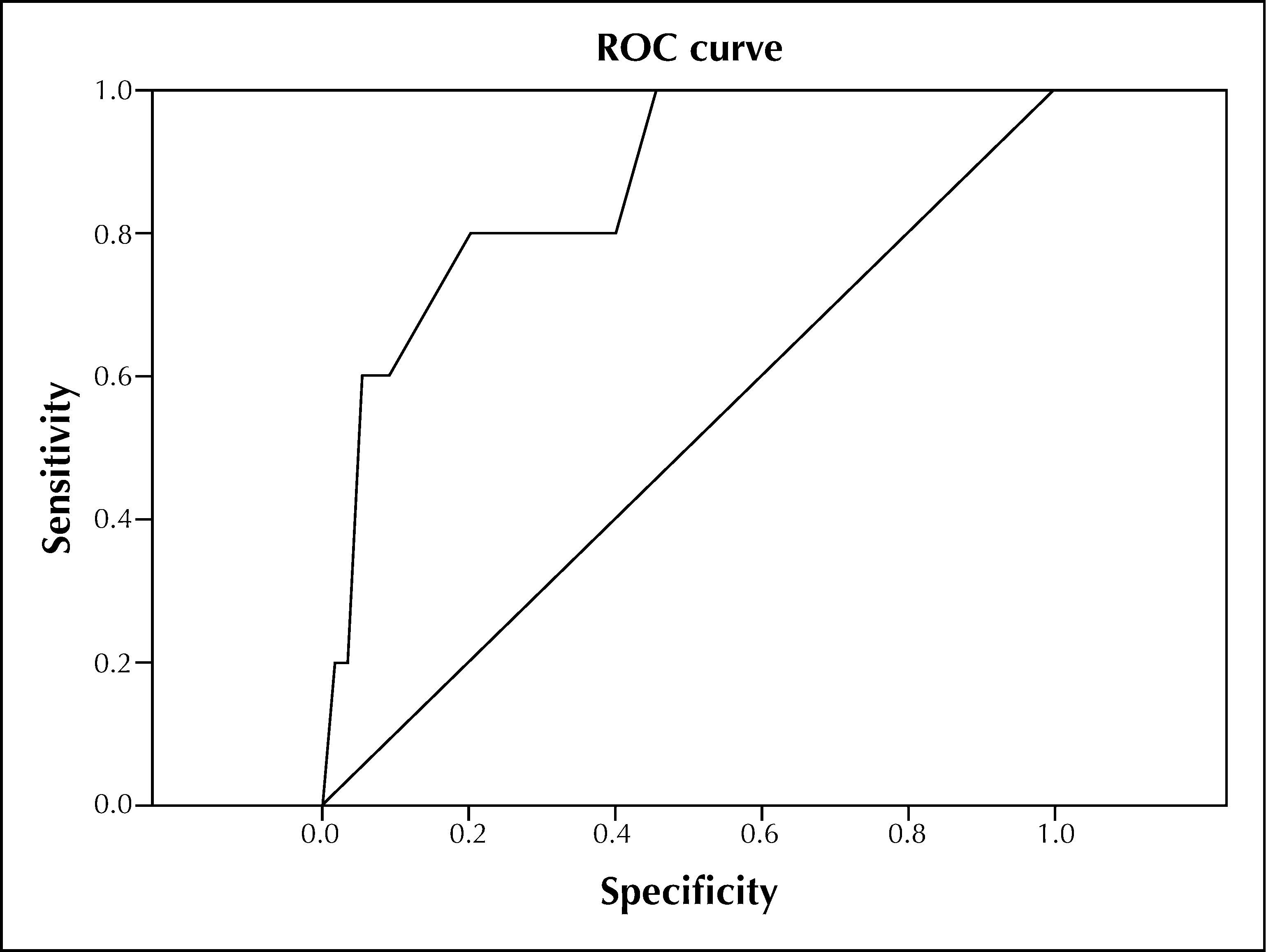
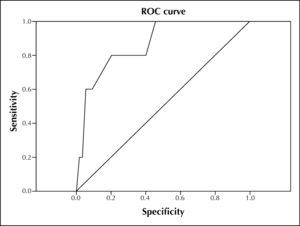
ResultsThe mean age of patients was 61.2±11 years, 25.4% were female, and 30.1% had diabetes mellitus. Lesions were most prevalent in the left anterior descending artery/diagonal branch (86.4%). During the procedure, 8.5% (5/59) of lesions had unsuccessful side branch predilation, and four of these bifurcations were treated with two stents. In the multivariate model, side branch stenosis at baseline was the only significant predictor of unsuccessful side branch predilation (odds ratio 1.15, 95%CI: 1.01–1.30; P=0.04), and side branch stenosis > 87.6% was identified as the most accurate cut-off value to predict failure in the receiver operating characteristic (ROC) curve.
ConclusionsSide branch predilation was associated with immediate side branch failure in < 10% of cases, and the only significant predictor in the multivariate model was side branch stenosis severity (> 85%) at baseline.
Impacto da Pré-Dilatação do Ramo Lateral no Procedimento de Intervenção Coronária Percutânea em Lesões de Bifurcação Coronária Complexas
IntroduçãoO tratamento de lesões de bifurcação com implante de stent único no vaso principal e stent provisional no ramo lateral pode ser limitado pelo grau de complexidade anatômica/ morfológica da lesão. A pré-dilatação do ramo lateral, um passo do procedimento geralmente evitado, pode ser necessária para manter a patência do ramo lateral. Investigamos o impacto da pré-dilatação do ramo lateral nos resultados imediatos de intervenção coronária percutânea em lesões de bifurcação coronária complexas.
MétodosEntre maio de 2008 e agosto de 2009, 59 pacientes com lesão de bifurcação coronária única e comprometimento significativo de vaso principal e ramo lateral foram incluídos no estudo. Os principais critérios de exclusão foram: envolvimento do tronco de coronária esquerda, infarto agudo do miocárdio com elevação do segmento ST (< 72 horas) e reestenose intrastent.
ResultadosA média de idade foi de 61,2±11 anos, 25,4% eram do sexo feminino e 30,1% tinham diabetes. As lesões mais frequentemente se localizaram em artéria descendente anterior/ramo diagonal (86,4%). Durante o procedimento, 8,5% (5/59) das lesões tiveram pré-dilatação do ramo lateral sem sucesso, e 4 dessas bifurcações foram tratadas com 2 stents. No modelo multivariado, a estenose do ramo lateral no pré-procedimento foi o único preditor significativo de pré-dilatação sem sucesso do ramo lateral (odds ratio 1,15, intervalo de confiança de 95% 1,01-1,30; P=0,04), e estenose > 87,6% no ramo lateral foi identificada na curva ROC como valor de corte com maior acurácia para predizer o insucesso.
ConclusõesA pré-dilatação do ramo lateral esteve associada a falência imediata do ramo lateral em < 10% dos casos e o único preditor significativo na análise multivariada foi a gravidade da estenose (> 85%) no ramo lateral no pré-procedimento.
Coronary bifurcation lesions represent up to 20% of lesions submitted to percutaneous coronary intervention (PCI).1 Notably, the use of PCI in bifurcation lesions has been associated with complex procedures and relatively low success rates (< 90%), primarily due to the occurrence of side branch complications.2–7 In recent years, several percutaneous techniques have been developed for the treatment of bifurcation lesions; however, the risk of side branch impairment (failure) through dissection, flow disturbance, occlusion, and/or significant residual stenosis remains of great concern to interventionists.8,9 Among the currently used technical approaches is treatment with a single stent, that is, a planned stent implantation in the main vessel and stent implantation in the side branch only if necessary. This simple approach is known as a provisional strategy.10 Alternatives include more complex treatments, such as stenting in both branches of the bifurcation (the main vessel and the side branch).11 Specifically, side branch predilation as an initial step in the PCI procedure in bifurcations (regardless of the technique employed) remains controversial, as it can cause impairment of the branch and difficulty of access; however, its performance, mainly in lesions with complex morphology, including severe disease at the side branch ostium, may be critical for maintaining branch patency during the procedure.12
This study aimed to evaluate the impact of side branch predilation on the immediate outcomes in a cohort of patients with complex coronary bifurcation lesions undergoing PCI with drug-eluting stent (DES) implantation, in a comparative study between a provisional strategy and the elective implant of 2 stents.
METHODSStudy design and populationThe present study represents a subanalysis of a prospective clinical, randomised study conducted in a single centre (Instituto de Cardiologia Dante Pazzanese, São Paulo, SP, Brazil) between May of 2008 and August of 2009.13 The primary inclusion criteria were age≥18 years; clinical presentation of stable or unstable angina or presence of silent ischemia; and presence of a single de novo lesion involving coronary bifurcation with significant impairment of the main vessel and side branch (‘true’ bifurcation lesion), with a branch lesion extending beyond the ostium (> 5mm). In contrast, the main exclusion criteria were myocardial infarction within 72 hours of the index procedure; renal failure, with a basal serum creatinine level≥2mg/dL; allergy, hypersensitivity, and/or contraindication to antithrombotic therapy with aspirin, thienopyridines (clopidogrel) and heparin; lesion located in the left main coronary artery; stent restenosis; and left ventricular ejection fraction < 30%.
The investigation protocol was in accordance with the Declaration of Helsinki related to research in humans and was approved by the ethics committee of the institution. All patients signed an informed consent prior to the index PCI procedure.
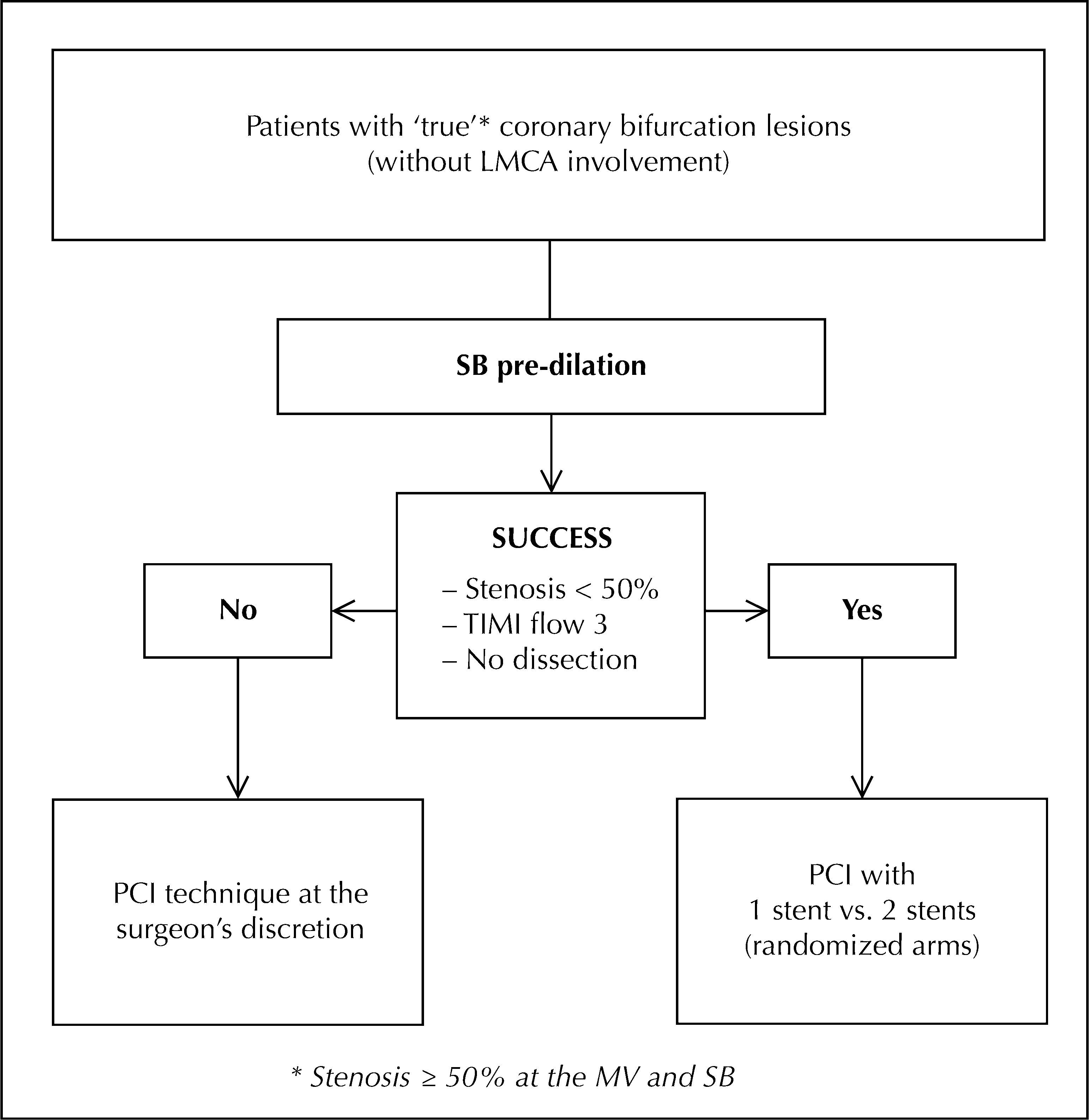
ProcedureThe technical approach proposed by the protocol included side branch predilation with subsequent randomisation, depending on the predilation outcome. The side branch predilation procedure was performed with a semi-compliant balloon-catheter with a diameter approximately 0.5mm smaller than that of the reference vessel. A successful side branch predilation was defined when the result of the control angiography showed a) residual stenosis < 50% (by visual estimation), b) a thrombolysis in myocardial infarction (TIMI) 3 flow, and c) the absence of any dissection. In cases of stenosis≥50%, TIMI flow < 3 and/or the presence of dissection, side branch predilation was considered unsuccessful (side branch failure). Patients who had unsuccessful side branch predilation were treated according to the surgeon’s discretion. Those with successful side branch predilation were subsequently randomised to PCI with a single-stent strategy (provisional technique) vs. an elective implant of 2 stents (any technique) (Figure 1). All patients were treated exclusively with second-generation, everolimus-releasing Xience™ V DES (Abbott Vascular – Santa Clara, CA, USA), which has been previously described in detail.14
The antithrombotic protocol followed current guidelines15 and consisted of the administration of two antiplatelet agents: acetylsalicylic acid (aspirin) and thienopyridine (clopidogrel). The pretreatment includes aspirin at a dose of 100–200mg/day in cases of chronic use (> seven days) or a single dose of 500mg administered > 24 hours prior to PCI; for clopidogrel, a loading dose of 300mg was administered either > 24 hours before the intervention in elective cases or 600mg were administered > 2 hours before the procedure in cases of acute coronary syndrome. After the PCI, the use of aspirin (100–200mg/day) was recommended indefinitely, and clopidogrel (75mg/day) was administered for a minimum of 12 months. Regarding antithrombin therapy during the procedure, intravenous heparin was administered at a dose of 70–100 U/kg to maintain an activated coagulation time > 250 seconds (> 200 seconds in cases of concomitant administration of glycoprotein IIb/IIIa according to the surgeon’s discretion).
DefinitionsMajor adverse cardiac events (MACEs) were defined by the composite outcome of cardiac death, myocardial infarction, and target lesion revascularisation. All deaths were considered to be cardiac unless a noncardiac cause could be clearly established by clinical or pathological analysis. Severe bleeding was defined according to the TIMI major bleeding criteria,16 which include intracranial haemorrhage, a decrease in haemoglobin levels≥5g/dL, or an absolute decrease in hematocrit≥15%. Angiographic success was defined by the presence of residual stenosis < 30% in the main vessel and < 50% in the side branch, according to the quantitative coronary angiography (QCA) analysis, in addition to the presence of anterograde TIMI 3 flow and the absence of dissection in the two bifurcation branches. Procedural success included angiographic success combined with the absence of MACE/severe bleeding during hospitalisation at the index procedure.
Angiographic analysisThe QCA and qualitative angiographic analyses were performed before and after the procedure. In general, these assessments followed the recommendations made by the Angiographic Subcommittee of the European Bifurcation Club.17 Image acquisition occurred after the intracoronary administration of nitrate (100–200μg), unless clinically contraindicated, and included two to three orthogonal projections (separated > 30 degrees), which aimed to optimise the visualisation of the target lesion. Bifurcation lesions were classified according to the Medina classification. 18 QCA analyses were performed off-line by experienced operators that were blinded to the procedure data through a validated and commercially available computer program (QAngio XA ® version 7.2, Medis – Leiden, the Netherlands) that incorporates a tool for performing dedicated segmental QCA analysis for coronary bifurcations. Lesion extension was delimited by the distance between the points immediately before and after the target stenosis considered to be free of the atheromatous process, i.e., the transition between the stenotic segment and the normal references (5–10mm) of the proximal and distal main vessel. In the side branch, lesion extension was considered from the ostium to the transition from the stenotic segment to the normal distal reference (5–10mm). The minimal lumen diameter and reference vessel diameter were used to calculate the stenosis diameter with the following formula:
DS (%)=[1−(MLD/RD)]×100,
in which DS=diameter stenosis, MLD=minimal lumen diameter, and RD=reference diameter.
Statistical analysisQuantitative variables were expressed as the mean and standard deviation and compared using Student’s t-test. Qualitative variables were expressed as absolute frequencies and percentages, and were compared by either the chi-squared test or Fisher’s exact test, as appropriate. A logistic regression model was used to evaluate the independent variables predictive of side branch predilation failure. The receiver operating characteristic (ROC) curve was constructed to evaluate cut-offs of quantitative variables identified by logistic regression with greater accuracy. The level of significance was set at 5% (α).
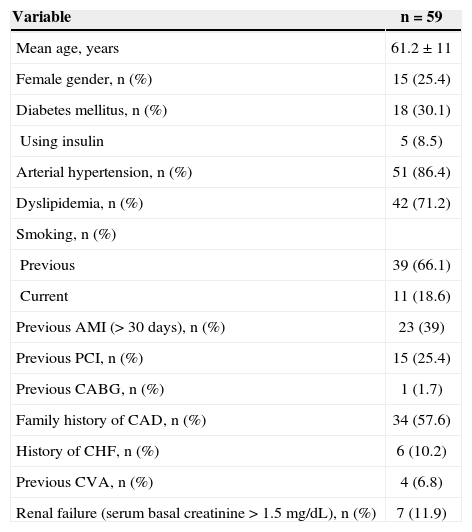
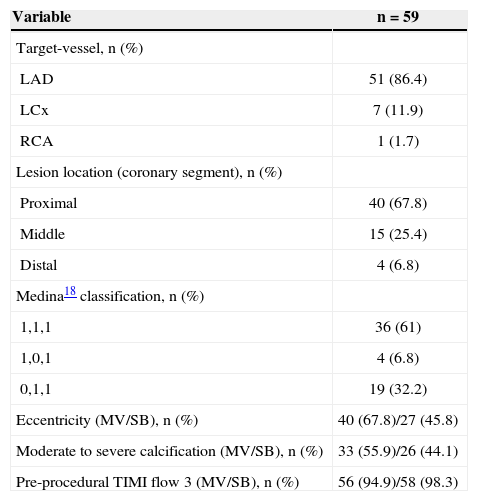
RESULTSThe study included 59 patients (59 coronary bifurcation lesions) who were submitted to the side branch predilation protocol. The mean age of the patients was 61.2±11 years, 30.1% were diabetics, 39% had a previous acute myocardial infarction (AMI) (19% with AMI < 30 days) and 11.9% had renal failure (Table 1). Regarding the clinical presentation, stable angina showed the highest prevalence (42.4%, n=25), followed by acute coronary syndrome in 25.4% (n=15), asymptomatic after recent AMI in 20.3% (n=12) and silent ischemia in 11.9% (n=7). Table 2 shows the angiographic data. Most bifurcation lesions (86.4%) involved the left anterior descending artery and the diagonal branch; additionally, most were located in the proximal segment of the coronary artery. All considered lesions showed significant impairment of the two bifurcation branches, and lesions of type 1,1,1, according to the classification of Medina,18 were found in 61% of cases. Regarding the left ventricular function, 36% of patients had some degree of dysfunction (< 50%).
Baseline Clinical Characteristics of Patients
| Variable | n=59 |
|---|---|
| Mean age, years | 61.2±11 |
| Female gender, n (%) | 15 (25.4) |
| Diabetes mellitus, n (%) | 18 (30.1) |
| Using insulin | 5 (8.5) |
| Arterial hypertension, n (%) | 51 (86.4) |
| Dyslipidemia, n (%) | 42 (71.2) |
| Smoking, n (%) | |
| Previous | 39 (66.1) |
| Current | 11 (18.6) |
| Previous AMI (>30days), n (%) | 23 (39) |
| Previous PCI, n (%) | 15 (25.4) |
| Previous CABG, n (%) | 1 (1.7) |
| Family history of CAD, n (%) | 34 (57.6) |
| History of CHF, n (%) | 6 (10.2) |
| Previous CVA, n (%) | 4 (6.8) |
| Renal failure (serum basal creatinine>1.5mg/dL), n (%) | 7 (11.9) |
CVA=cerebrovascular accident; CABG=coronary artery bypass graft; CAD=coronary artery disease; AMI=acute myocardial infarction; CHF=congestive heart failure; PCI=percutaneous coronary intervention; n=number of patients.
Angiographic Characteristics of Patients
| Variable | n=59 |
|---|---|
| Target-vessel, n (%) | |
| LAD | 51 (86.4) |
| LCx | 7 (11.9) |
| RCA | 1 (1.7) |
| Lesion location (coronary segment), n (%) | |
| Proximal | 40 (67.8) |
| Middle | 15 (25.4) |
| Distal | 4 (6.8) |
| Medina18 classification, n (%) | |
| 1,1,1 | 36 (61) |
| 1,0,1 | 4 (6.8) |
| 0,1,1 | 19 (32.2) |
| Eccentricity (MV/SB), n (%) | 40 (67.8)/27 (45.8) |
| Moderate to severe calcification (MV/SB), n (%) | 33 (55.9)/26 (44.1) |
| Pre-procedural TIMI flow 3 (MV/SB), n (%) | 56 (94.9)/58 (98.3) |
RCA=right coronary artery; LCx=left circumflex artery; LAD=left anterior descending artery; n=number of patients; SB=side branch; TIMI=thrombolysis in myocardial infarction; MV=main vessel.
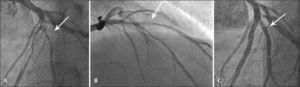
During the procedure, 8.5% of the lesions (5/59) showed side branch predilation failure due to dissection (4/5) or significant residual stenosis (1/5). Figure 2 shows a case involving the left anterior descending artery/ diagonal branch with a lateral branch with severe and diffuse disease, which showed dissection after predilation and was treated with a mini-crush technique. Of the five patients with side branch predilation failure, four were treated with a 2-stent strategy (T-stenting technique, two; mini-crush, two). The other patient with side branch predilation failure had severe lesion calcification, which proved to be non-responsive to successive dilation attempts with a balloon catheter; thus, he was ultimately treated with the single-stent technique, as it was not possible to deliver the stent to that branch. The patients who achieved successful side branch predilation (54/59) were treated with a 2-stent technique in 59.3% (n=32) and a single stent in 40.7% of cases (n=22). Simultaneous post-dilation with a kissing-balloon was performed in 100% of the lesions that showed unsuccessful side branch predilation vs. 96.3% in successfully dilated lesions. At the end of the procedure, the angiographic success rate was 80% (4/5) in the group without side branch predilation success (one lesion showed significant residual stenosis of the side branch) vs. 98.2% (53/54) in the group with successful side branch predilation, in which one lesion showed side branch occlusion after treatment with a single stent (P=0.09). The procedural success was similar for both groups (80% vs. 87%). In the successful predilation group, seven patients had MACE/bleeding, including periprocedural AMI (n=6), and major bleeding (n=1) associated with the use of a glycoprotein IIb / IIIa inhibitor.
– Image of a ‘true’ coronary bifurcation lesion located in the proximal segment of the anterior descending artery (A), which showed dissection of the diagonal branch after predilation with a balloon-catheter (B), treated with a 2-stent (mini-crush) technique with good angiographic results (C).
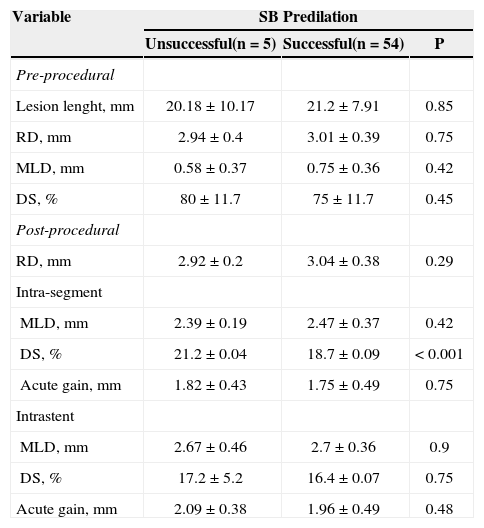
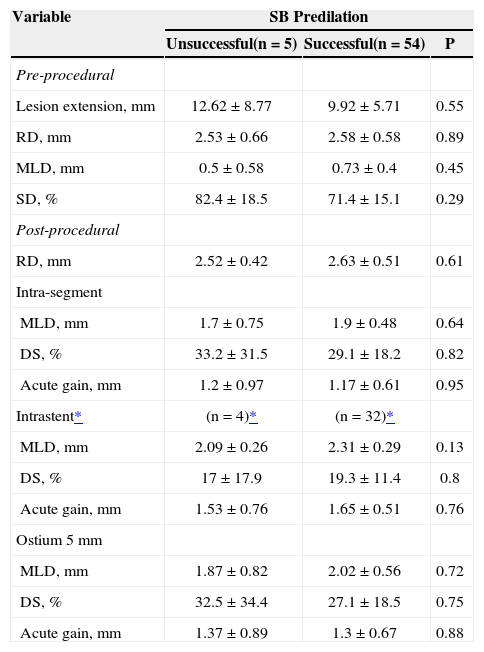
The comparisons of the QCA data of the main vessels and side branches are shown in Tables 3 and 4, respectively. In general, the group with unsuccessful side branch predilations had more extensive side branch lesions, a smaller minimal lumen diameter, and more severe obstruction compared with the side branches of the group with successful predilations. The multivariate analysis evaluated the presence of calcification, distal and proximal angles, eccentricity, lesion extension, reference vessel diameter, minimal lumen diameter, and stenosis diameter percentages. The only significant predictor of side branch predilation failure was the percentage of diameter stenosis at the ostium of the side branch by QCA analysis (odds ratio 1.15 for each percentage unit; 95% confidence interval: 1.01–1.30; P=0.04). The analysis of the ROC curve (Figure 3) with a cut-off value of the side branch percent diameter stenosis > 87.6% before the procedure was identified as a predictor of side branch predilation failure, with an accuracy of 86.5%.
Quantitative Coronary Angiography of the Main Vessel Comparing Lesions with Successful vs. Unsuccessful Predilation
| Variable | SB Predilation | ||
|---|---|---|---|
| Unsuccessful(n=5) | Successful(n=54) | P | |
| Pre-procedural | |||
| Lesion lenght, mm | 20.18±10.17 | 21.2±7.91 | 0.85 |
| RD, mm | 2.94±0.4 | 3.01±0.39 | 0.75 |
| MLD, mm | 0.58±0.37 | 0.75±0.36 | 0.42 |
| DS, % | 80±11.7 | 75±11.7 | 0.45 |
| Post-procedural | |||
| RD, mm | 2.92±0.2 | 3.04±0.38 | 0.29 |
| Intra-segment | |||
| MLD, mm | 2.39±0.19 | 2.47±0.37 | 0.42 |
| DS, % | 21.2±0.04 | 18.7±0.09 | < 0.001 |
| Acute gain, mm | 1.82±0.43 | 1.75±0.49 | 0.75 |
| Intrastent | |||
| MLD, mm | 2.67±0.46 | 2.7±0.36 | 0.9 |
| DS, % | 17.2±5.2 | 16.4±0.07 | 0.75 |
| Acute gain, mm | 2.09±0.38 | 1.96±0.49 | 0.48 |
Values expressed as the means±SD. DS, %=percentage of diameter stenosis; MLD=minimum lumen diameter; RD=reference diameter; n=number of patients; SB=side branch.
Quantitative Coronary Angiography of the Side Branch Comparing Lesions with Successful vs. Unsuccessful Predilation
| Variable | SB Predilation | ||
|---|---|---|---|
| Unsuccessful(n=5) | Successful(n=54) | P | |
| Pre-procedural | |||
| Lesion extension, mm | 12.62±8.77 | 9.92±5.71 | 0.55 |
| RD, mm | 2.53±0.66 | 2.58±0.58 | 0.89 |
| MLD, mm | 0.5±0.58 | 0.73±0.4 | 0.45 |
| SD, % | 82.4±18.5 | 71.4±15.1 | 0.29 |
| Post-procedural | |||
| RD, mm | 2.52±0.42 | 2.63±0.51 | 0.61 |
| Intra-segment | |||
| MLD, mm | 1.7±0.75 | 1.9±0.48 | 0.64 |
| DS, % | 33.2±31.5 | 29.1±18.2 | 0.82 |
| Acute gain, mm | 1.2±0.97 | 1.17±0.61 | 0.95 |
| Intrastent* | (n=4)* | (n=32)* | |
| MLD, mm | 2.09±0.26 | 2.31±0.29 | 0.13 |
| DS, % | 17±17.9 | 19.3±11.4 | 0.8 |
| Acute gain, mm | 1.53±0.76 | 1.65±0.51 | 0.76 |
| Ostium 5mm | |||
| MLD, mm | 1.87±0.82 | 2.02±0.56 | 0.72 |
| DS, % | 32.5±34.4 | 27.1±18.5 | 0.75 |
| Acute gain, mm | 1.37±0.89 | 1.3±0.67 | 0.88 |
Values expressed as the means±SD.
In the current analysis, a technical approach was proposed with side branch predilation prior to stenting implant in bifurcation lesions. However, the systematic performance of such a procedure has been the subject of controversy, as lumen enlargement at the side branch ostium location can lead to dissections, which can hinder or even prevent access to the side branch through the stent struts in cases of treatment with the provisional strategy.10 Another issue has been the possibility that side branch predilation promotes guidewire recrossing in the side branch through the proximal struts, which could also compromise, at least in theory, the structural stent conformation in the main vessel in relation to the side branch origin.19 Conversely, side branch predilation has been indicated in cases where access to the side branch is difficult or when the stenosis is severe and calcified.10,19 In these situations, such a procedure may facilitate access to the side branch, while providing an increased vascular lumen. In general, the difficulty or impossibility of access (or recrossing) to the side branch remains a limiting factor for PCI in coronary bifurcation lesions. Previous studies have identified several predictors of poor access to the side branch, which include significant calcification involving the proximal segment of the main vessel or the side branch, severe stenosis with massive plaque build-up in the proximal segment of the main vessel, excessive tortuosity in the proximal segment of the bifurcation lesion, distal angle > 90 degrees, and compromised side branch flow.20,21
The present study included only coronary bifurcation lesions with significant side branch impairments, with lesions extending beyond the ostium. The pre-procedural angiographic analysis of the side branch showed mean values of the lesion extension and degree of obstruction in patients in the randomised study arms (group with successful side branch predilation) of 9.9mm and 71%, respectively. The group with unsuccessful side branch predilation had more complex lesions, including a mean lesion length and degree of obstruction of the side branch of 12.6mm and 82%, respectively. Nonetheless, these differences were not significant, which was likely due to the small sample size. Additionally, 44% of lesions had moderate to severe calcification in the side branch. Previous studies observed that the risk of occlusion of the side branch is proportional to the degree of stenosis. An analysis by Chaudhry et al.22 demonstrated that for each increase of 10 percentage points in the degree of stenosis, the risk of side branch impairment increased by 23% during a percutaneous approach with single stenting. In the present study, the presence of calcification was also associated with a compromised side branch (P=0.06). It is noteworthy that the side branch involvement was associated with the occurrence of periprocedural myocardial infarction.
Therefore, the use of a technical approach with systematic side branch predilation in the present study is justified by the complexity of the included lesions. Furthermore, the side branch predilation failure in this situation could lead to early identification of the morphologies that are unsuitable for treatment with a provisional strategy, as changing to the 2-stent strategy can be difficult, and there is no guarantee of success, especially due to side branch involvement.20 In such cases, techniques that allow for a primary stent implant in the side branch, such as crush or Culotte stenting, should be preferred.11 In the present study, side branch predilation failure occurred in 8.5% of cases, and the only independent predictor identified in the multivariate analysis was the degree of stenosis of the side branch. Specifically, a degree of stenosis of 87.6% was identified as a poor response predictor cut-off of the side branch predilation. However, further studies that are properly designed and have adequate statistical power are needed to completely evaluate the impact of side branch predilation on complex coronary bifurcation lesions.
CONCLUSIONSThe side branch predilation procedure in complex coronary bifurcation lesions treated by PCI was associated with relatively low immediate side branch failure rates (< 10%). Nonetheless, this procedure was able to identify at an early stage certain morphologies that are most likely inadequate for the provisional strategy approach, which must be considered when selecting the PCI technique in this complex subgroup. In the multivariate analysis, the degree of side branch stenosis before the procedure was the only independent predictor of the predilation failure of the identified side branch.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.