Ad hoc percutaneous coronary intervention (PCI) has proven to be safe in certain subsets of patients and the number of procedures has grown steadily over the years. In face of the scarcity of literature publications, we performed a comparative analysis of in-hospital outcomes of ad hoc and elective PCIs.
MethodsFrom 2006 to 2010, 4,957 consecutive patients were submitted to PCI and were included in the Hospital Bandeirantes Registry. Patients undergoing primary or rescue PCI were excluded and of the remaining 4,048 patients, 1,510 (37.3%) were submitted to ad hoc PCI and 2,538 to elective PCI.
ResultsThe ad hoc PCI group was younger, had a lower prevalence of comorbidities and a greater number of patients were treated in the presence of acute coronary syndrome. They exhibited less complex coronary lesions, used larger diameter stents and had more transient flow impairments during PCI. Procedure success was similar between groups (97% vs. 96.8%; P=0.70) as well as the occurrence of death (0.5% vs. 0.3%; P=0.19), myocardial infarction (1.3% vs. 1.8%; P=0.17), emergency coronary artery bypass graft surgery (0.4% vs. 0.2%; P=0.36), stroke (0.1% vs. 0; P=0.71) and major vascular complications (0.3% vs. 0.4%; P=0.64).
ConclusionsAd hoc PCI is performed in lower risk patients and the outcomes demonstrate it is a safe procedure for most of the selected patients.
Resultados Hospitalares da Intervenção Coronária Percutânea Ad Hocvs. Eletiva
IntroduçãoA realização de intervenções coronárias percutâneas (ICPs) ad hoc tem mostrado ser segura em certos subgrupos de pacientes e o número de procedimentos tem aumentado progressivamente ao longo dos anos. Diante da escassez de estudos na literatura, realizamos análise comparativa dos re sultados hospitalares das ICPs ad hoc e eletiva.
MétodosNo período de 2006 a 2010, 4.957 pacientes consecutivos fo ram submetidos a ICP e incluídos no Registro do Hospital Bandeirantes. Foram excluídos os pacientes submetidos a ICP primária ou de resgate, restando 4.048 pacientes, 1.510 (37,3%) submetidos a ICP ad hoc e 2.538, a ICP eletiva.
ResultadosO grupo ICP ad hoc mostrou ser mais jovem, com menor prevalência de comorbidades e maior número de pacientes tratados na vigencia da síndrome coronária aguda. Mostraram ter menor gravidade angiográfica, utilizaram stents de maior diâmetro e apresentaram mais distúrbios de fluxo transitórios durante a ICP. O sucesso do procedimento foi semelhante entre os grupos (97% vs. 96,8%; P=0,70), assim como a ocorrência de óbito (0,5% vs. 0,3%; P=0,19), infarto do miocárdio (1,3% vs. 1,8%; P=0,17), revascularização miocárdica de emergência (0,4% vs. 0,2%; P=0,36), acidente vascular cerebral (0,1% vs. 0; P=0,71) e complicações vasculares maiores (0,3% vs. 0,4%; P=0,64).
ConclusõesA ICP ad hoc é realizada em pacientes de menor risco e seus resultados demonstram que é um procedimento seguro para a maioria dos pacientes selecionados.
The expression ad hoc is of Latin origin, and its literal translation is “for this” or “for this purpose”.1,2 In interventional cardiology, this expression has been used to define percutaneous coronary intervention (PCI) performed immediately after coronary angiography.
The use of PCI in the treatment of coronary heart disease is well established and is increasing.3 In the United States, the number of PCIs increased from 400,000 procedures performed in 2000 to 1,265,000 in the year 2005.4 Over the past two decades, there has been a proportionally significant increase in the number of ad hoc PCIs worldwide.1,5 Rahman et al.5 report that during a ten-year period (1990 to 2000), the occurrence of these interventions increased from 54% to 88%, and had less significant complication rates. These data are similar to those from the State of New York registry, where 80% of the PCIs are ad hoc.6
The use of ad hoc PCI has been frequent in Brazil. The procedure is safe compared with elective PCI in selected cases,7 and it is more comfortable for the patient, since it prevents additional procedures and brings a potential reduction in the rate of vascular complications at the puncture site.7-10 However, some disadvantages have been reported, such as increased exposure to radiation, a greater volume of contrast used (and therefore a greater chance of developing contrast-induced nephropathy), increased procedure time, difficulty in obtaining informed consent for the therapeutic procedure, and pressure for faster decision-making that compromises the concept of the “heart team”.7-10
Considering the advantages and disadvantages of ad hoc PCI and the scarcity of studies in our country, a comparative analysis of in-hospital outcomes of elective vs. ad hoc PCIs was performed.
METHODSPatientsFrom August 2006 to November 2010, 4,957 consecutive patients undergoing PCI were included in the Hospital Bandeirantes registry (São Paulo, SP, Brazil). Patients undergoing primary or rescue PCI were excluded, leaving a total of 4,048 patients, of whom 1,510 (37.3%) were submitted to ad hoc and 2,538, to elective PCI. Data were collected prospectively and stored in an electronic database. Clinical outcomes were recorded at hospital discharge.
PCIThe PCIs were performed (almost entirely) via femoral access, and the radial approach was employed in a few cases. The choice of the material and technique used during the procedure, as well as decisions regarding the use of glycoprotein IIb/IIIa inhibitors, were at the surgeon’s discretion. Unfractionated heparin was used at the beginning of the procedure at a dose of 70 U/kg and 100 U/kg, except in patients who were already using low-molecular weight heparin.
All patients received combined antiplatelet therapy with acetylsalicylic acid (ASA, a loading dose of 300mg and a maintenance dose of 100mg/day to 200mg/day), and clopidogrel (with a loading dose of 300mg to 600mg and a maintenance dose of 75mg/day). The femoral sheaths were removed four hours after the start of heparinization. The radial sheaths were removed immediately after the procedure.
Angiographic analysis and definitionsAnalyses were performed using at least two orthogonal projections by professionals who had experience with quantitative coronary angiography. This study used the same angiographic criteria as listed in the database of the National Center of Cardiovascular Intervention (Central Nacional de Intervenção Cardiovascular – CENIC) of Brazilian Society of Interventional Cardiology.11 The type of lesion was classified according to the criteria of American College of Cardiology and American Heart Association (ACC/AHA).12 The Thrombolysis in Myocardial Infarction (TIMI) classification was used to determine coronary flow prior to and after the procedure.13 Procedural success was defined as angiographic success achievement (residual stenosis<30% with TIMI 3 flow) and the absence of major adverse cardiac or cerebrovascular events including death from any cause, myocardial infarction, stroke, or emergency CABG surgery.14
Myocardial infarction was indicated by the presence of new ischemic EKG alterations and/or alterations in laboratory markers of myocardial necrosis three-fold above the upper normal value and/or angiographic evidence of target vessel occlusion. Emergency CABG surgery was considered when performed immediately after the PCI.
Statistical analysisThe data stored in the Oracle-based database were plotted in Excel spreadsheets and were analyzed using the SPSS, release 15.0. Continuous variables were expressed as means±standard deviation, and categorical variables were expressed as absolute numbers and percentages. The associations between continuous variables were evaluated using an analysis of variance (ANOVA). Associations between categorical variables were evaluated using the chi-square or Fisher’s exact test or likelihood ratio when appropriate. The significance level was set at P<0.05.
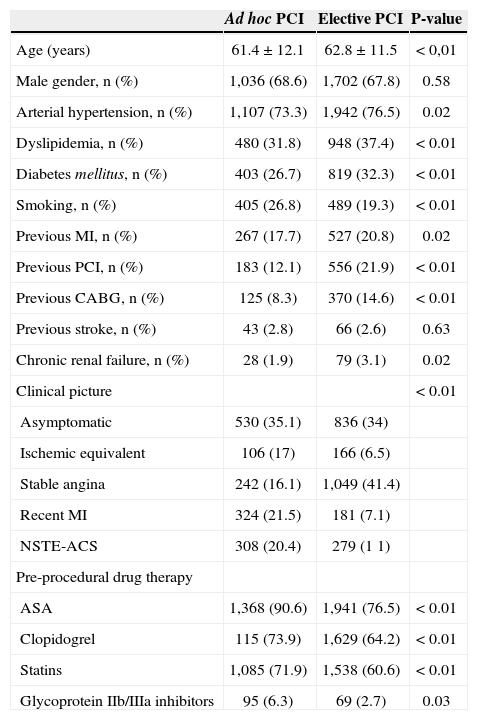
RESULTSThe clinical characteristics are shown in Table 1. The ad hoc PCI group was on average one year younger (61.4±12.1years vs. 62.8±11.5years; P<0.01) and had a lower prevalence of risk factors for atherosclerosis, with the exception of smoking (26.8% vs. 19.3%; P<0.01). This group also had a lower prevalence of previous revascularization procedures (percutaneous 12.1% vs. 21.9%; P<0.01; surgical 8.3% vs. 14.6%; P=0.02), as well as a lower prevalence of comorbidities such as myocardial infarction (17.7% vs. 20.8%; P=0.02) or chronic renal failure (1.9% vs. 3.1%; P=0.02). Regarding clinical presentation, a greater number of the patients in the ad hoc PCI group were treated in the evolved phase of myocardial infarction (21.5% vs. 7.1%) or were treated in the presence of non-ST-elevation acute coronary syndrome (20.4% vs.% 11). Regarding the pre-procedure pharmacotherapy, the ad hoc PCI group had more patients receiving ASA (90.6% vs. 76.5%; P<0.01), clopidogrel (73.9% vs. 64.2%; P<0.01), and statins (71.9% vs. 60.6%, P<0.01). Glycoprotein IIb / IIIa inhibitors were also more frequently used in the ad hoc PCI group (6.3% vs. 2.7%; P=0.03).
Clinical characteristics
| Ad hoc PCI | Elective PCI | P-value | |
|---|---|---|---|
| Age (years) | 61.4±12.1 | 62.8±11.5 | < 0,01 |
| Male gender, n (%) | 1,036 (68.6) | 1,702 (67.8) | 0.58 |
| Arterial hypertension, n (%) | 1,107 (73.3) | 1,942 (76.5) | 0.02 |
| Dyslipidemia, n (%) | 480 (31.8) | 948 (37.4) | < 0.01 |
| Diabetes mellitus, n (%) | 403 (26.7) | 819 (32.3) | < 0.01 |
| Smoking, n (%) | 405 (26.8) | 489 (19.3) | < 0.01 |
| Previous MI, n (%) | 267 (17.7) | 527 (20.8) | 0.02 |
| Previous PCI, n (%) | 183 (12.1) | 556 (21.9) | < 0.01 |
| Previous CABG, n (%) | 125 (8.3) | 370 (14.6) | < 0.01 |
| Previous stroke, n (%) | 43 (2.8) | 66 (2.6) | 0.63 |
| Chronic renal failure, n (%) | 28 (1.9) | 79 (3.1) | 0.02 |
| Clinical picture | < 0.01 | ||
| Asymptomatic | 530 (35.1) | 836 (34) | |
| Ischemic equivalent | 106 (17) | 166 (6.5) | |
| Stable angina | 242 (16.1) | 1,049 (41.4) | |
| Recent MI | 324 (21.5) | 181 (7.1) | |
| NSTE-ACS | 308 (20.4) | 279 (1 1) | |
| Pre-procedural drug therapy | |||
| ASA | 1,368 (90.6) | 1,941 (76.5) | < 0.01 |
| Clopidogrel | 115 (73.9) | 1,629 (64.2) | < 0.01 |
| Statins | 1,085 (71.9) | 1,538 (60.6) | < 0.01 |
| Glycoprotein IIb/IIIa inhibitors | 95 (6.3) | 69 (2.7) | 0.03 |
MI, myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft; NSTE-ACS, non-ST-elevation acute coronary syndrome; ASA, acetylsalicylic acid.
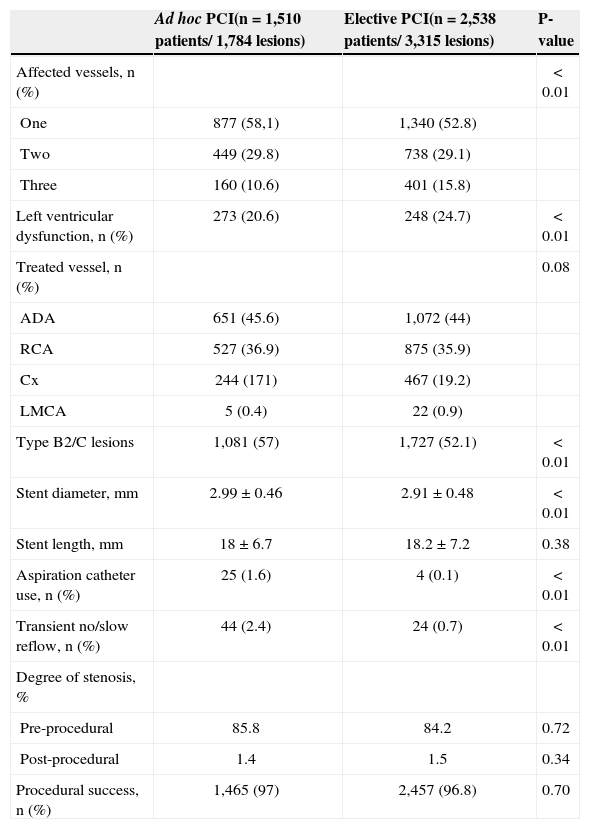
As presented in Table 2, the ad hoc PCI group had fewer severe patients, who also had a lower prevalence of three-vessel disease (10.6% vs. 15.8%) or left ventricular dysfunction (20.6% vs. 24.7%; P<0.01). However, type B2/C lesions were more frequently treated in this group (57% vs. 52.1%; P<0.01). The left anterior descending artery was the most frequently approached vessel in both groups (45.6% vs. 44%). Regarding the characteristics of the procedures (Table 2), the ad hoc PCI group had stents that were larger in diameter (2.99±0.46mm vs. 2.91±0.48mm), but were of equal length to those implanted in the elective PCI group (18±6.7mm vs. 18.2±7.2mm; P=0.38). In the ad hoc PCI group, aspiration catheters were more frequently used (1.6% vs. 0.1%; P<0.01), and transient flow disturbances occurred more frequently (no reflow and slow reflow) (2.4% vs. 0.7%; P<0.01) during the PCI. Procedural success was similar between the groups (97% vs. 96.8%; P=0.70).
Angiographic and procedural characteristics
| Ad hoc PCI(n=1,510 patients/ 1,784 lesions) | Elective PCI(n=2,538 patients/ 3,315 lesions) | P-value | |
|---|---|---|---|
| Affected vessels, n (%) | < 0.01 | ||
| One | 877 (58,1) | 1,340 (52.8) | |
| Two | 449 (29.8) | 738 (29.1) | |
| Three | 160 (10.6) | 401 (15.8) | |
| Left ventricular dysfunction, n (%) | 273 (20.6) | 248 (24.7) | < 0.01 |
| Treated vessel, n (%) | 0.08 | ||
| ADA | 651 (45.6) | 1,072 (44) | |
| RCA | 527 (36.9) | 875 (35.9) | |
| Cx | 244 (171) | 467 (19.2) | |
| LMCA | 5 (0.4) | 22 (0.9) | |
| Type B2/C lesions | 1,081 (57) | 1,727 (52.1) | < 0.01 |
| Stent diameter, mm | 2.99±0.46 | 2.91±0.48 | < 0.01 |
| Stent length, mm | 18±6.7 | 18.2±7.2 | 0.38 |
| Aspiration catheter use, n (%) | 25 (1.6) | 4 (0.1) | < 0.01 |
| Transient no/slow reflow, n (%) | 44 (2.4) | 24 (0.7) | < 0.01 |
| Degree of stenosis, % | |||
| Pre-procedural | 85.8 | 84.2 | 0.72 |
| Post-procedural | 1.4 | 1.5 | 0.34 |
| Procedural success, n (%) | 1,465 (97) | 2,457 (96.8) | 0.70 |
PCI, percutaneous coronary intervention; ADA, anterior descending artery; RCA, right coronary artery; Cx, circumflex artery; LMCA, left main coronary artery.
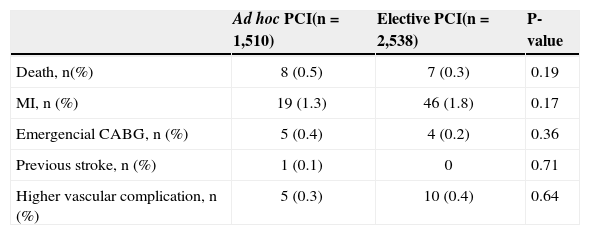
Regarding hospital clinical outcomes (Table 3), there was no significant difference between groups regarding the incidence of death (0.5% vs. 0.3%; P=0.19), myocardial infarction (1.3% vs. 1.8%; P=0.17), emergency CABG (0.4% vs. 0.2%; P=0.36), or stroke (0.1% vs. 0; P=0.71). The incidence of major vascular complications was also similar between the groups (0.3% vs. 0.4%; P=0.64).
Hospital clinical outcomes
| Ad hoc PCI(n=1,510) | Elective PCI(n=2,538) | P-value | |
|---|---|---|---|
| Death, n(%) | 8 (0.5) | 7 (0.3) | 0.19 |
| MI, n (%) | 19 (1.3) | 46 (1.8) | 0.17 |
| Emergencial CABG, n (%) | 5 (0.4) | 4 (0.2) | 0.36 |
| Previous stroke, n (%) | 1 (0.1) | 0 | 0.71 |
| Higher vascular complication, n (%) | 5 (0.3) | 10 (0.4) | 0.64 |
PCI, percutaneous coronary intervention; MI, myocardial infarction; CABG, coronary artery bypass graft.
PCI following the angiographic diagnostic procedure (ad hoc PCI) had limitations until two decades ago, due to the unavailability of digital technology for image acquisition and the need for surgical backup with a surgical center available for all procedures at all times. With the development of image acquisition, guide and catheter technology, and especially stents and dual antiplatelet therapy, the need for emergency surgeries lessened significantly, and the number of ad hoc procedures over the past two decades has increased.
In the present registry, ad hoc procedures account for little more than one third of the total PCIs. When compared with other studies,8 this low rate can be explained by the difficulty in justifying costs (particularly in the supplementary private health care) regarding the need for PCI following the diagnostic procedure in patients with a stable clinical condition. In the present registry, most patients undergoing ad hoc PCI had acute coronary syndrome or had a history of recent myocardial infarction, as opposed to the elective PCI group patients who primarily had stable angina.
Despite increased patient comfort, the performance of ad hoc PCI in stable patients can become a difficult or even inappropriate decision: in cases of unprotected trunk lesions or multivessel disease, in which the guidelines emphasize the need for the participation of clinicians and surgeons in therapeutic decision-making (the “heart team”); when there is a significant likelihood of exceeding the maximum doses of ionizing radiation or contrast media; when there are doubts regarding the effective use of optimized drug therapy or quantification of ischemia in non-invasive tests; and in cases where there is no informed consent from the patient regarding the procedure that will follow the diagnostic coronary angiography. These and other aspects have been addressed in the recent publication of a consensus by the Society for Cardiovascular Angiography and Interventions (SCAI).15
In the present registry, patients undergoing elective PCI were older and showed higher clinical complexity. The possibility of complications resulting from a greater amount of contrast and a longer procedure likely assisted in the selection of more severe patients for this group. These findings (previously reported by Goldstein et al.)10 demonstrated that patients undergoing ad hoc PCI had fewer comorbidities. The in-hospital mortality rates did not differ between the ad hoc and non-ad hoc groups (odds ratio [OR] 1.14; P=0.38) but were more significant in the ad hoc PCI group in the presence of comorbidities such as congestive heart failure or class IV stable angina.
Although the patients in the ad hoc PCI group had fewer comorbidities, as well as clinical characteristics that were more favorable for procedure performance, negative effects such as type B2/C lesions, the presence of flow disturbances, and the need for the use of aspiration catheters and glycoprotein IIb/IIIa inhibitors were more frequently observed in this group. This finding may be explained by the increased number of patients with acute coronary syndrome and recent myocardial infarction in this group. Similarly, since a higher percentage of antiplatelet agents prior to the ad hoc procedure was indicative of the patient’s condition, this factor facilitated decision-making in favor of the intervention following the coronary angiography.
The presence of multivessel disease was a factor against the performance of ad hoc PCI, which had a higher number of single-vessel patients. Single-vessel disease is an angiographic characteristic more commonly found in younger patients and smokers.16
There were no significant differences between the two groups regarding in-hospital clinical outcomes. In the American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR), in the period between 2001 and 2003, 60.6% of the patients who underwent ad hoc PCI also showed no differences between those who were electively treated for the occurrence of death, renal failure, or vascular complications during hospitalization.8 In another analysis of the New York registry, Hannan et al.6 assessed 46,565 PCIs that were performed between 2003 and 2005, and found no differences regarding in-hospital mortality between the ad hoc and elective PCI groups. At the three-year follow-up, however, the ad hoc PCI group had a lower mortality rate.
Study limitationsThe limitations of the present study include the retrospective analysis of data, its performance in a single center, and the absence of late follow-up.
CONCLUSIONSThe present results demonstrate that ad hoc PCI should be performed in patients with lower risks and is safe for most selected patients.
CONFLICT OF INTERESTThe authors declare no conflicts of interest.