The Angiocardio Registry, which comprises data from five different centers in the state of São Paulo, offers the opportunity to study the association between cardiovascular risk factors and coronary artery disease (CAD) extent, as assessed by coronary angiography. This study aimed to evaluate independent predictors of multivessel CAD in Brazil.
MethodsFrom August 2006 to January 2014, 16,320 patients with CAD were included and divided into the single- and multivessel groups.
ResultsPatients with multivessel disease (n = 9,512, 58.3%) were on average 3 years older, with a higher prevalence of males (69.4% vs. 65.4%; p < 0.01), arterial hypertension (80.0% vs. 73.5%; p < 0.01), diabetes (40.7% vs. 28.8%; p < 0.01), dyslipidemia (39.6% vs. 34.9%; p < 0.01), family history of CAD (23.0% vs. 21.3%; p < 0.01), chronic renal failure (4.1% vs. 2.6%; p < 0.01), previous stroke (3.8% vs. 2.8%; p < 0.01), peripheral vascular disease (4.0% vs. 3.3%; p = 0.02) and previous myocardial infarction (18.4% vs. 13.9%; p < 0.01), as well as a lower prevalence of smoking (20.0% vs. 24.5%; p < 0.01). At the multivariate analysis, the following were independent predictors of multivessel lesion: age > 40 years (odds ratio - OR = 1.996; 95% CI: 1.52-2.63; p < 0.01), male gender (OR = 1.202; 95% CI: 1.12-1.28; p < 0.01), arterial hypertension (OR = 1.439; 95% CI: 1.34-1.55; p < 0.01), diabetes (OR =1.697; 95% CI: 1.59-1.81; p < 0.01), dyslipidemia (OR = 1.223; 95% CI: 1.15-1.30; p < 0.01), previous acute myocardial infarction (OR = 1.393; 95% CI: 1.28-1.52; p < 0.01), and chronic renal failure (OR = 1.597; 95% CI: 1.33-1.91; p < 0.01).
ConclusionsMultivessel CAD in Brazil is associated with traditional risk factors for atherosclerosis, except for smoking. Age, diabetes, and chronic renal failure were the strongest predictors for multivessel CAD assessed by coronary angiography.
O Registro Angiocardio, que agrega dados de cinco diferentes centros do Estado de São Paulo, oferece a oportunidade de estudar a associação de fatores de risco cardiovasculares com a extensão da doença arterial coronária (DAC), avaliada pela cinecoronariografia. Este estudo buscou analisar preditores independentes de DAC multiarterial em nosso meio.
MétodosDe agosto de 2006 a janeiro de 2014, 16.320 pacientes com DAC foram incluídos e divididos nos grupos uni e multiarterial.
ResultadosPacientes multiarteriais (n = 9.512, 58,3%) apresentaram-se, em média, 3 anos mais idosos, com maior prevalência do sexo masculino (69,4% vs. 65,4%; p < 0,01), hipertensão arterial (80,0% vs. 73,5%; p < 0,01), diabetes (40,7% vs. 28,8%; p < 0,01), dislipidemia (39,6% vs. 34,9%; p < 0,01), antecedentes familiares de DAC precoce (23,0% vs. 21,3%; p < 0,01), insuficiência renal crônica (4,1% vs. 2,6%; p < 0,01), acidente vascular cerebral prévio (3,8% vs. 2,8%; p < 0,01), doença vascular periférica (4,0% vs. 3,3%; p = 0,02) e infarto do miocárdio prévio (18,4% vs. 13,9%; p < 0,01), além de menor prevalência de tabagismo (20,0% vs. 24,5%; p < 0,01). À análise multivariada, foram preditores independentes de lesão multiarterial idade > 40 anos (odds ratio - OR = 1,996; IC 95% 1,52-2,63; p < 0,01), sexo masculino (OR = 1,202; IC 95% 1,12-1,28; p < 0,01), hipertensão arterial (OR = 1,439; IC 95% 1,34-1,55; p < 0,01), diabetes (OR = 1,697; IC 95% 1,59-1,81; p < 0,01), dislipidemia (OR = 1,223; IC 95% 1,15-1,30; p < 0,01), infarto agudo do miocárdio prévio (OR = 1,393; IC 95% 1,28-1,52; p < 0,01) e insuficiência renal crônica (OR = 1,597; IC 95% 1,33-1,91; p < 0,01).
ConclusõesA DAC multiarterial em nosso meio é associada aos fatores de risco tradicionais para aterosclerose, com exceção do tabagismo. A idade, o diabetes e a insuficiência renal crônica foram os fatores preditores mais fortes para a DAC multiarterial avaliada pela cinecoronariografia.
Cardiovascular disease is the most common cause of death in developed or developing countries. From an epidemiological perspective, a risk factor is a characteristic of an individual or population, which is present early and is associated with an increased risk of disease development in the future.
Arterial hypertension, diabetes, dyslipidemia, obesity, sedentary lifestyle, genetic inheritance, and smoking are well-defined risk factors for the development of coronary artery disease (CAD). New factors have been constantly researched in order to better understand the severity and extent of CAD, including C-reactive protein, type-B natriuretic peptide, osteoprotegerin, infection by Chlamydia pneumoniae, and genetic polymorphism, among others.1–4
The extent of CAD is crucial for treatment decision-making and patient prognosis.5 Some nonrandomized studies have suggested a greater influence of certain risk factors, in spite of others, on the severity of coronary disease.6–8 However, the association between traditional risk factors and the extent of coronary atherosclerotic involvement in one or more vessels is still unclear in the literature, and studies in Brazil are still scarce.9,10
The present study aimed to evaluate the association between traditional risk factors and the extent of CAD, detected by coronary angiography, in search for multivessel disease predictors.
MethodsPopulation and definitionsPatients with suspected CAD submitted to coronary angiography at one of the five centers that comprise the Angiocardio Registry (Hospital Bandeirantes, Hospital Rede D’Or São Luiz Anália Franco, and Hospital Leforte, in São Paulo; Hospital Vera Cruz, in Campinas and Hospital Regional do Vale do Paraíba, in Taubaté − all in the state of São Paulo, Brazil), and who had angiographic confirmation of CAD, were included in this study. Data were prospectively collected and stored in a computerized database available through the internet for all centers participating in the registry.
The population was divided into the single-vessel group, which had coronary obstruction ≥ 50% in only one major epicardial branch or its branches, or the multivessel group, which had coronary obstruction ≥ 50% in more than one major epicardial branch or their branches.
ProcedureMost coronary angiographies were performed through the femoral approach, whereas the radial approach was used as an option in some cases. The choice of technique and material used during the procedure was at the interventionists’ discretion.
The femoral sheaths were removed immediately after the procedure, except in cases in which rescue or ad hoc primary percutaneous coronary intervention (PCI) was performed, when they were removed 4hours after the start of heparinization. The radial sheaths were removed immediately after the procedure was finished.
Angiographic analyses were performed by experienced interventionists, using digital quantitative angiography.
Statistical analysisThe data stored in an Oracle-based database were plotted in Excel spreadsheets and analyzed using the Statistical Package for Social Sciences (SPSS), version 15.0. Continuous variables were expressed as mean ± standard deviation, and categorical variables, as absolute number and percentile. The associations between the continuous variables were evaluated using the Analysis of Variance (ANOVA). The associations between categorical variables were assessed by Chi-squared test, Fischer's exact test, or likelihood ratio, when appropriate. The significance level was set at p < 0.05. Simple and multiple logistic regression models were applied to identify predictors of multivessel disease. In these regression models, age, due to its importance as a variable, was stratified into age groups.
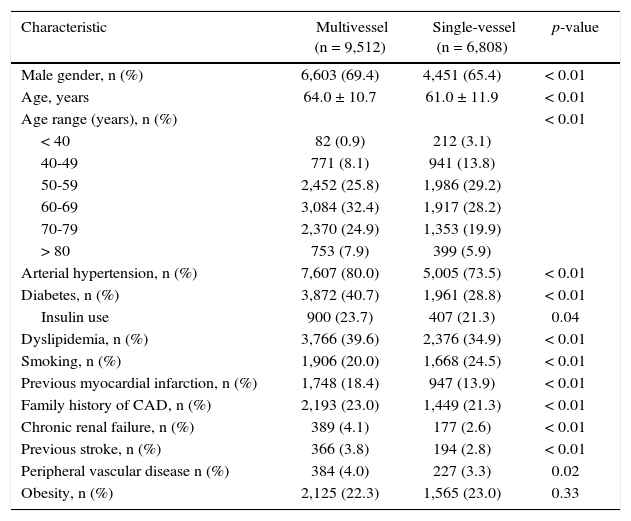
ResultsFrom August 2006 to January 2014, 29,538 patients with suspected CAD were submitted to coronary angiography, of whom 16,320 (55.3%) were confirmed and divided into the multivessel (n = 9,512, 58.3%) and single-vessel (n = 6,808) groups. The multivessel group was, on average, 3 years older, with a greater predominance of males (69.4% vs. 65.4%; p < 0.01). In this group, arterial hypertension (80.0% vs. 73.5%; p < 0.01), diabetes (40.7% vs. 28.8%; p < 0.01), dyslipidemia (39.6% vs. 34.9%; p < 0.01), and a family history of CAD (23.0% vs. 21.3%; p < 0.01) were more frequent than in the single-vessel group, as well as the presence of chronic renal failure (4.1% vs. 2.6%; p < 0.01), previous stroke (3.8% vs. 2.8%; p < 0.01), peripheral vascular disease (4.0% vs. 3.3%; p = 0.02), and acute myocardial infarction (18.4% vs. 13.9%; p < 0.01). In the group with single-vessel involvement, smoking prevailed (24.5% vs. 20%; p < 0.01). The obesity rate did not differ between the two groups (Table 1).
Clinical characteristics.
| Characteristic | Multivessel (n = 9,512) | Single-vessel (n = 6,808) | p-value |
|---|---|---|---|
| Male gender, n (%) | 6,603 (69.4) | 4,451 (65.4) | < 0.01 |
| Age, years | 64.0 ± 10.7 | 61.0 ± 11.9 | < 0.01 |
| Age range (years), n (%) | < 0.01 | ||
| < 40 | 82 (0.9) | 212 (3.1) | |
| 40-49 | 771 (8.1) | 941 (13.8) | |
| 50-59 | 2,452 (25.8) | 1,986 (29.2) | |
| 60-69 | 3,084 (32.4) | 1,917 (28.2) | |
| 70-79 | 2,370 (24.9) | 1,353 (19.9) | |
| > 80 | 753 (7.9) | 399 (5.9) | |
| Arterial hypertension, n (%) | 7,607 (80.0) | 5,005 (73.5) | < 0.01 |
| Diabetes, n (%) | 3,872 (40.7) | 1,961 (28.8) | < 0.01 |
| Insulin use | 900 (23.7) | 407 (21.3) | 0.04 |
| Dyslipidemia, n (%) | 3,766 (39.6) | 2,376 (34.9) | < 0.01 |
| Smoking, n (%) | 1,906 (20.0) | 1,668 (24.5) | < 0.01 |
| Previous myocardial infarction, n (%) | 1,748 (18.4) | 947 (13.9) | < 0.01 |
| Family history of CAD, n (%) | 2,193 (23.0) | 1,449 (21.3) | < 0.01 |
| Chronic renal failure, n (%) | 389 (4.1) | 177 (2.6) | < 0.01 |
| Previous stroke, n (%) | 366 (3.8) | 194 (2.8) | < 0.01 |
| Peripheral vascular disease n (%) | 384 (4.0) | 227 (3.3) | 0.02 |
| Obesity, n (%) | 2,125 (22.3) | 1,565 (23.0) | 0.33 |
CAD: coronary artery disease.
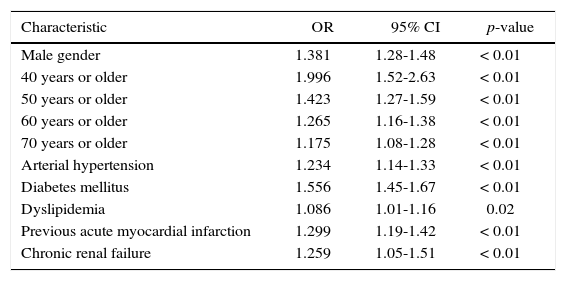
In the multivariate analysis, age > 40 years (odds ratio - OR = 1.996; 95% CI: 1.52-2.63; p < 0.01), male gender (OR = 1.381; 95% CI: 1.28-1.48; p < 0.01), arterial hypertension (OR = 1.234; 95% CI: 1.14-1.33; p < 0.01), diabetes (OR = 1.556; 95% CI: 1.45-1.67; p < 0.01), dyslipidemia (OR = 1.086; 95% CI: 1.01-1.16; p < 0.02), previous acute myocardial infarction (OR = 1.299; 95% CI: 1.19-1.42; p < 0.01) and chronic renal failure (OR = 1.259; 95% CI: 1.05-1.51; p < 0.01) were the most important variables to differentiate single-vessel patients from those with multivessel involvement (Table 2).
Independent predictors of multivessel coronary disease.
| Characteristic | OR | 95% CI | p-value |
|---|---|---|---|
| Male gender | 1.381 | 1.28-1.48 | < 0.01 |
| 40 years or older | 1.996 | 1.52-2.63 | < 0.01 |
| 50 years or older | 1.423 | 1.27-1.59 | < 0.01 |
| 60 years or older | 1.265 | 1.16-1.38 | < 0.01 |
| 70 years or older | 1.175 | 1.08-1.28 | < 0.01 |
| Arterial hypertension | 1.234 | 1.14-1.33 | < 0.01 |
| Diabetes mellitus | 1.556 | 1.45-1.67 | < 0.01 |
| Dyslipidemia | 1.086 | 1.01-1.16 | 0.02 |
| Previous acute myocardial infarction | 1.299 | 1.19-1.42 | < 0.01 |
| Chronic renal failure | 1.259 | 1.05-1.51 | < 0.01 |
OR, odds ratio; 95% CI, 95% confidence interval.
The role of traditional risk factors in the development of CAD has been well known since the early Framingham results, and new variables have been constantly studied. Despite an increasingly better pathophysiological understanding, the reasons why CAD shows a great variety in its angiographic presentation still raise questions. One of them is whether one or more risk factors may be directly associated with single- or multivessel disease, as demonstrated by angiography. The present study was the first study carried out in Brazil that associates traditional risk factors with the angiographic extension of CAD in a large cohort of patients.
In this study, among the assessed risk factors, diabetes mellitus, dyslipidemia, arterial hypertension, family history of CAD, as well as male gender, age, chronic renal failure, and clinical evidence of previously manifested atherosclerosis were more frequent among individuals with multivessel disease, whereas only smoking was more frequent among those with single-vessel disease. The independent predictors of multivessel involvement were age older than 40 years, male gender, diabetes, hypertension, dyslipidemia, chronic renal failure, and previous acute myocardial infarction.
Several studies have shown a greater or lesser influence of these factors on disease severity and some have identified the presence of diabetes as a fundamental condition for atherosclerotic disease progression in multivessel coronary territory. Zand Parsa et al.,6 in a small series, showed that only diabetes mellitus was closely associated with the presence of multivessel disease. In the report by Veeranna et al.,11 only diabetes showed to be an independent predictor of multivessel CAD.
The presence of type 1 diabetes is markedly related to multivessel disease, of greater severity and with the involvement of the distal coronaries, especially among women (loss of gender difference).12 In type 2 diabetes patients, the prevalence of multivessel involvement in both genders also occurs, as shown in a coronary angiotomography study that also showed a greater occurrence of calcified plaques among them.13 However, the greater severity and extent of CAD seems to already occur among glucose-intolerant patients. These had greater lumen narrowing and longer coronary obstructions when compared to non-diabetic patients.14 Diabetes also has an important association with CAD progression. In the MESA (Multi-Ethnic Study of Atherosclerosis) study, in which 5,756 patients were evaluated by angiotomography, diabetes was the strongest predictor of coronary calcification progression (an important CAD marker) during a mean period of 2.4 years.15
Age and male gender have been listed as independent predictors of more extensive CAD along with diabetes, high blood pressure, and alterations in cholesterol.16 In a study carried out with angiotomography performed in 1,015 asymptomatic patients, age and male gender were the strongest predictors of the presence of coronary plaques (calcified, non-calcified, or mixed).17 Smoking was a strong predictor of non-calcified and more vulnerable plaques. The association of smoking with non-calcified plaques and single-vessel CAD, as in the present study, might lead to the wrong interpretation that it is a less expressive risk factor. However, its more frequent presence among younger individuals7 contributes to this angiographic characteristic, since age is a predictor of more extensive disease and often brings other factors, such as hypertension, diabetes, and dyslipidemia. In a recent review of the ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) study,18 Robertson et al. described that the angiographic pattern of smokers was comparable to that of non-smokers, but the former were approximately 10 years younger.
Among young individuals, family history of premature CAD, together with smoking, is often a risk factor.7 Although little associated to CAD extension, it is strongly related to its presence, regardless of the presence of other concomitant risk factors.19 Fischer et al.20 found a correlation of heredity – not with the number of affected vessels, but with the presence of lesions in proximal portions of the coronary arteries or in the left main coronary artery.
Dyslipidemia, one of the predictors of multivessel atherosclerotic involvement in the present study, has been quantitatively associated with CAD severity and extent. Higher values of triglycerides, Lp (a),10 non-high density lipoprotein cholesterol (HDL-c), low-density lipoprotein cholesterol (LDL-c),21 and oxidized LDL22 have been positively correlated with the multivessel presentation of CAD, while HDL-c and ApoA are inversely related.7
Obesity was present in more than 20% of the studied population, which reflects the statistics of its prevalence in Brazil. Although it is not an independent predictor of CAD, its association with hypertension, dyslipidemia, and diabetes deserves attention. Because obese patients are referred for coronary angiography at a younger age, the occurrence of less severe and less extensive CAD is justified – this is the “obesity paradox”.23
The increase in visceral adiposity regardless of body mass index, assessed by computed tomography, was positively correlated with the extent of CAD in the study by Lee et al.,24 in which patients in the highest tertile showed a four- to five-fold higher chance of having multivessel CAD when compared to the lower tertiles.
Based on the results, the authors can establish a differentiated line of care for patients with predictors of greater severity and extent of CAD, even during the period that precedes the invasive diagnostic investigation with coronary angiography, improving prevention, care, and clinical outcomes.
Study limitationsThe main limitations of the present study were its retrospective evaluation of the data in a population with CAD selected by coronary angiography and an analysis limited to the risk factors commonly measured in a clinical setting, while other factors might have been relevant.
ConclusionsMultivessel coronary artery disease in Brazil was associated with traditional risk factors for atherosclerosis, except for smoking. Age, diabetes, and chronic renal failure were the strongest predictors of coronary artery disease assessed by coronary angiography.
Funding sourcesNone declared.
Conflicts of interestThe authors declare no conflicts of interest.
Peer review under the responsibility of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.