Mid-ventricular hypertrophic obstructive cardiomyopathy is a rare variant form (1%) of hypertrophic obstructive cardiomyopathy. In this case, we report a patient referred for elective cardiac catheterization due to angina and dyspnea on moderate exertion, with no significant coronary obstruction, and left ventriculography indicating the presence of mid-ventricular hypertrophic obstructive cardiomyopathy with an intraventricular pressure gradient of 130mmHg.
Cardiomiopatia Hipertrófica Obstrutiva Médio-Ventricular
A cardiomiopatia hipertrófica obstrutiva médio-ventricular é uma variante rara (1%) da miocardiopatia hipertrófica obstrutiva. Neste relato de caso, apresentamos uma paciente encaminhada para realização de cateterismo cardíaco eletivo por angina e dispneia aos moderados esforços, sem obstrução coronariana significativa e com ventriculografia esquerda, demostrando cardiomiopatia hipertrófica obstrutiva médio-ventricular com um gradiente pressórico intraventricular de 130mmHg.
Mid-ventricular hypertrophic obstructive cardiomyopathy, first described by Falicov et al.1 in 1976, is a rare type (1%) of hypertrophic obstructive cardiomyopathy.2 In this variant, there is a significant mid-ventricular hypertrophy associated with a mid-ventricular stenosis, which confers the aspect of a dumbbell to the left ventricle,3 with generation of a pressure gradient between the apical and basal chambers, as well as an absence of obstruction of outflow.2
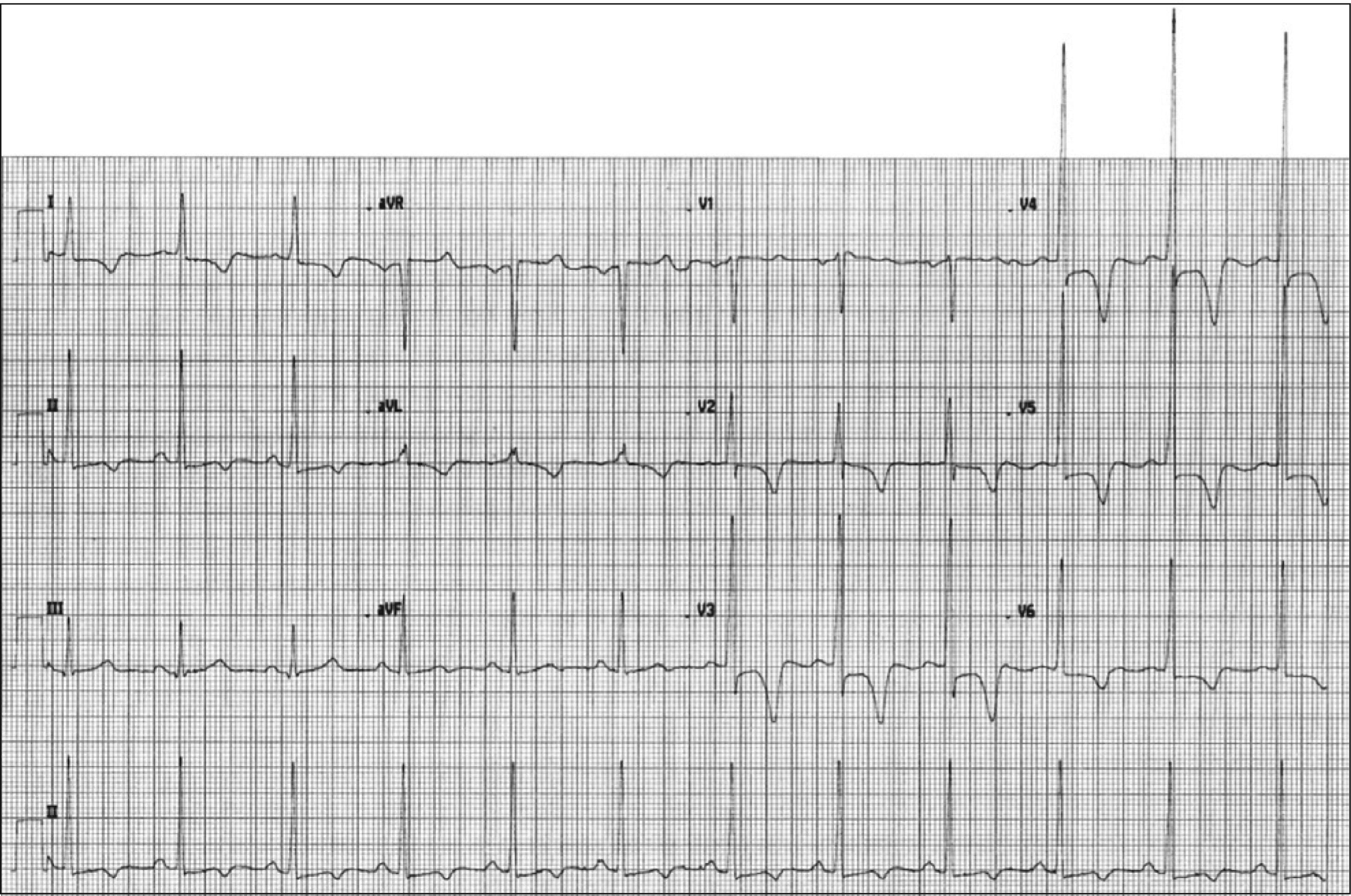
CASE REPORTA female patient, 80 years, was referred for elective cardiac catheterization due to angina and dyspnea on moderate exertion. Physical examination revealed mid-systolic murmur without other significant findings. An electrocardiogram showed criteria for left ventricular hypertrophy and secondary changes in ventricular repolarization (Figure 1). The coronary angiography showed no significant coronary stenoses; however, a left ventriculography in the right anterior oblique projection (30°) revealed mid-ventricular hypertrophic obstructive cardiomyopathy (Figure 2); after analysis of intracavitary pressures, a gradient of 130mmHg was calculated (Figure 3).
Midventricular hypertrophic obstructive cardiomyopathy is a phenotype distinct of hypertrophic obstructive cardiomyopathy, associated with an unfavorable prognosis. Efthimiadis et al.,4 in a study comparing clinical characteristics and natural history of patients with hypertrophic cardiomyopathy, with and without mid-ventricular obstruction, observed that its presence is a strong and independent predictor of sudden death, as well as a determinant of progression to end-stage hypertrophic obstructive cardiomyopathy and to heart failure-related death.
Apical aneurysms were observed in approximately 25% of patients with mid-ventricular obstructive hypertrophic cardiomyopathy, and were almost unique to this group. Their presence served as a marker of an even worse clinical course.
Apical dilation may occur in cases of severe narrowing and of progression to a “burned out apex”, with apical aneurysm formation in approximately 10% of patients.3 The pathogenesis of myocardial necrosis remains unknown. It has been suggested that the apical aneurysm may be secondary to after-load and to an increase of apical pressure, as a result of a mid-ventricular obstruction seen in the degenerative process of hypertrophic cardiomyopathy. Other possible causes of aneurysm formation are small vessel disease with decreased coronary flow reserve, coronary stenosis due to an increased wall stress in the hypertrophied myocardial segment, decreased coronary perfusion pressure due to the mid-ventricular obstruction, coronary spasm, and decreased capillary/ myocardial fiber ratio.5
If left untreated, the midventricular obstructive hypertrophic cardiomyopathy can cause fatal ventricular arrhythmias and sudden death. Beta-blockers are the first therapeutic choice for hypertrophic obstructive cardiomyopathy, but the treatment of mid-ventricular obstructive hypertrophic cardiomyopathy remains unclear. Dual-chamber pacemaker6 and percutaneous myocardial ablation7,8 have been proposed as non-surgical treatments, but the long-term benefits and safety of these therapeutic options require further study.5 The surgical treatment of midventricular hypertrophic obstructive cardiomyopathy is poorly described in the literature, mostly in the form of case reports.9 Kunkala et al.,9 in a recent study involving 56 patients, described the results of a transapical approach, noting that this option allows an excellent approach for myectomy, as well as for the relief of the intraventricular gradient and associated symptoms without any complications related to the apical incision were observed with a five-year survival similar to that expected in the general population (95% vs. 97%).
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.
FUNDING SOURCENone.