Systemic arterial hypertension affects over 1.2 million people worldwide. Only 35% of hypertensive patients have controlled blood pressure levels. Renal sympathetic denervation (RSD) has shown to significantly decrease blood pressure levels in patients with resistant systemic hypertension.
METHODSProspective, single arm, observational, multicenter study including consecutive patients undergoing RSD. The primary endpoint was to assess systolic blood pressure levels at the 30-day follow-up. The secondary endpoint was to determine the presence of procedure-related adverse events.
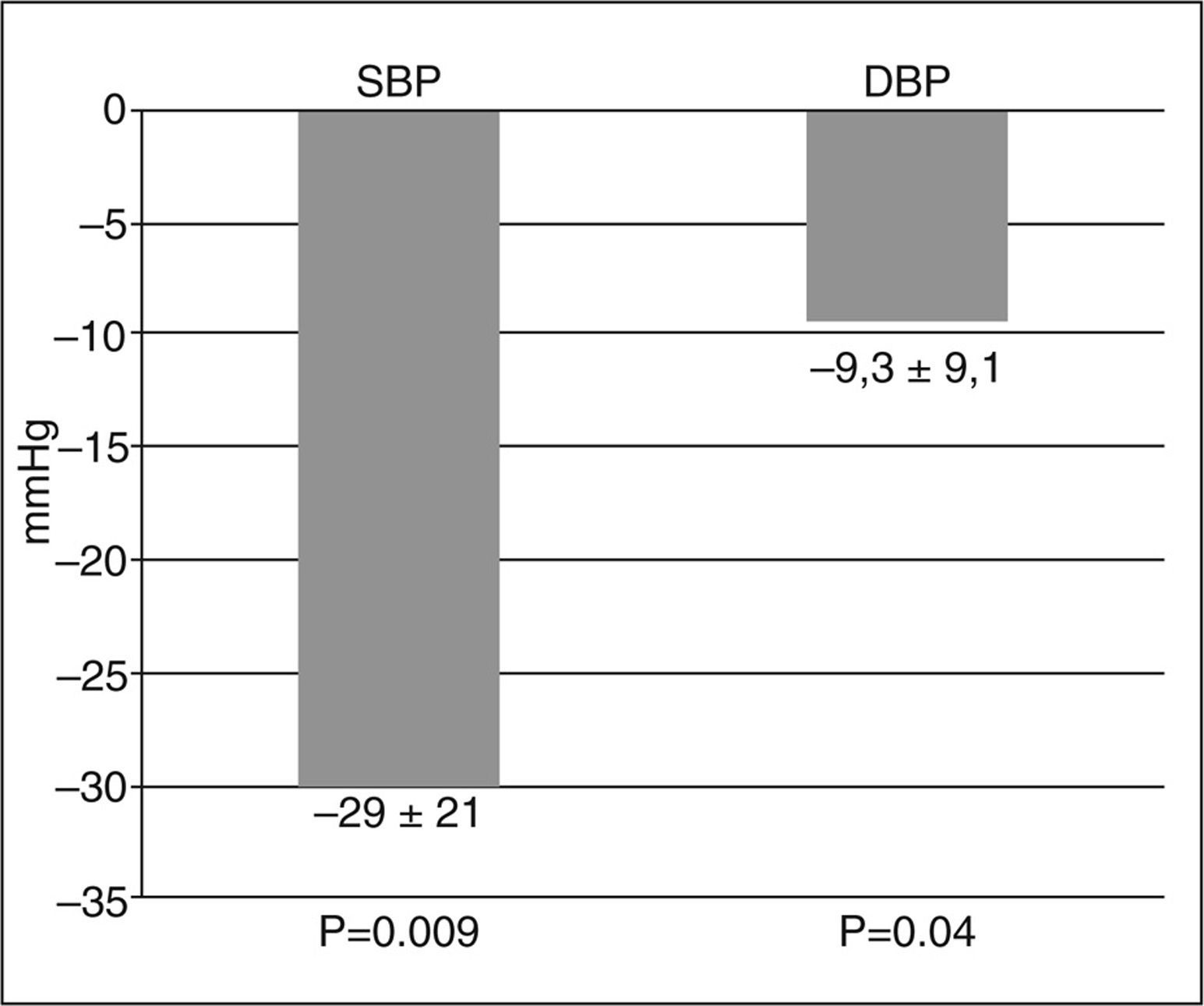
RESULTSThe first 20 patients undergoing RSD were included. The average blood pressure prior the procedure was 171.6/93.2±15.5/ 11.3mmHg, with the use of 4.1±1.5 antihypertensive drugs per patient. Success rate was 95%, and 11.1±1.9 ablations were performed per patient. A systolic blood pressure decrease of 29±21mmHg (P=0.009) was observed 30 days after the procedure. There were no procedure-related complications.
ConclusionsCatheter-based RSD in daily clinical practice patients significantly decreased blood pressure levels. In our experience, RSD proved to be feasible and safe.
Denervação Simpática Renal para o Controle daHipertensão Arterial Resistente
IntroduçãoA hipertensão arterial sistêmica afeta mais de 1,2 milhão de pessoas no mundo. Apenas 35% dos pacientes hiper-tensos têm valores de pressão arterial controlados. Recentemente a denervação simpática renal (DSR) tem demonstrado diminuir significativamente os valores de pressão arterial nos pacientes com hipertensão arterial sistêmica resistente.
MétodosEstudo prospectivo, de braço único, observacional, multicêntrico, in-cluindo pacientes consecutivos submetidos a DSR. O objetivo primário foi avaliar os níveis da pressão arterial sistólica aos 30 dias de seguimento. O objetivo secundário foi determinar a ocorrência de qualquer evento adverso relacionado com o procedimento.
ResultadosForam incluídos os primeiros 20 pacientes submetidos a DSR. A média de pressão arterial antes do procedimento foi de 171,6/93,2±15,5/11,3mmHg, com média de uso de 4,1±1,5 fármacos anti-hipertensivos por paciente. A taxa de sucesso foi de 95%, tendo sido aplicadas 11,1±1,9 ablações por paciente. Foi observada diminuição média de 29±21mmHg (P=0,009) na pressão arterial sistólica 30 dias após o procedimento. Não houve complicação associada ao procedimento.
ConclusõesA DSR por cateter em pacientes da prática clínica diária diminuiu significativamente os valores de pressão arterial. Em nossa experiência, a DSR demonstrou ser factível e segura.
Systemic arterial hypertension (SAH) affects over 1.2 million people worldwide, with a prevalence of 28% in the adult population.1,2 The consequences and progressive damage of SAH on target organs reduce patient survival, accounting for half of coronary and cerebrovascular events.3,4
Adequate control of SAH reduces the occurrence of adverse events. A 5mmHg reduction in the systolic blood pressure is associated with a 10% decrease in relative risk of death from cerebrovascular causes and acute coronary syndrome. Conversely, a 20mmHg increase in systolic blood pressure doubles the risk of mortality from cardiovascular causes.5 However, only 35% of hypertensive patients have blood pressure values within the targets proposed by the guidelines,5 in most cases due to poor adherence to prescribed treatment, suboptimal treatment, or secondary causes of SAH. However, approximately 10% of patients with appropriate use of three or more antihypertensive drugs do not manage to control their blood pressure levels; this group of patients, known as resistant hypertensive patients, have a high risk for the occurrence of adverse cardiovascular events.6
In the resistant hypertensive population, studies using microneurography and measurement of blood catecholamines demonstrated the participation of the sympathetic nervous system in the genesis and main-tenance of SAH.7−9 Surgical sympathectomy was shown to be effective in reducing blood pressure in patients with resistant SAH; however, this technique was aban-doned due to high rates of complications.10−12 More recently, a less invasive approach with percutaneous renal sympathetic denervation performed by applying radiofrequency to the renal artery wall was shown to decrease adrenergic tone, release of norepinephrine, and blood pressure.13 Catheter-guided (Symplicity®, Ardian Medtronic – Minneapolis, USA) renal sympathetic denervation was tested in the clinical trials Symplicity HTN-1-first-in-man and Symplicity HTN-2, presenting a significant and sustained decrease in systolic blood pressure.13,14 Recently, this system was made available for clinical use in Venezuela, initiating the authors’ experience with this procedure.
This study aimed to describe the characteristics of patients undergoing renal sympathetic denervation, as well as to evaluate the efficacy and safety of the procedure in daily clinical practice.
METHODSRenal sympathetic denervation systemThe components of the renal sympathetic denervation system are the Symplicity® catheter and radiofre-quency generator. The generator consists of two parts: the console and the pedal (Figure 1). The generator produces energy through radiofrequency, following a predetermined algorithm. During the radiofrequency application, voltage, temperature, and impedance of the application point on the renal artery are continuously monitored and controlled. The maximum voltage is 8W, and the system generates energy with impedances between 20 ohms and 500 ohms. The Symplicity® catheter, compatible with 6 Fr, applies radiofrequency energy to the renal artery wall. It comprises the handle lever and a flexible portion, 108cm long, with a platinum monopolar electrode at the tip, with two radiopaque marks 5mm apart from each other. By manipulating the handle lever, the catheter tip can be flexed and/or rotated to reach the correct position for the application of radiofrequency (Figure 2).
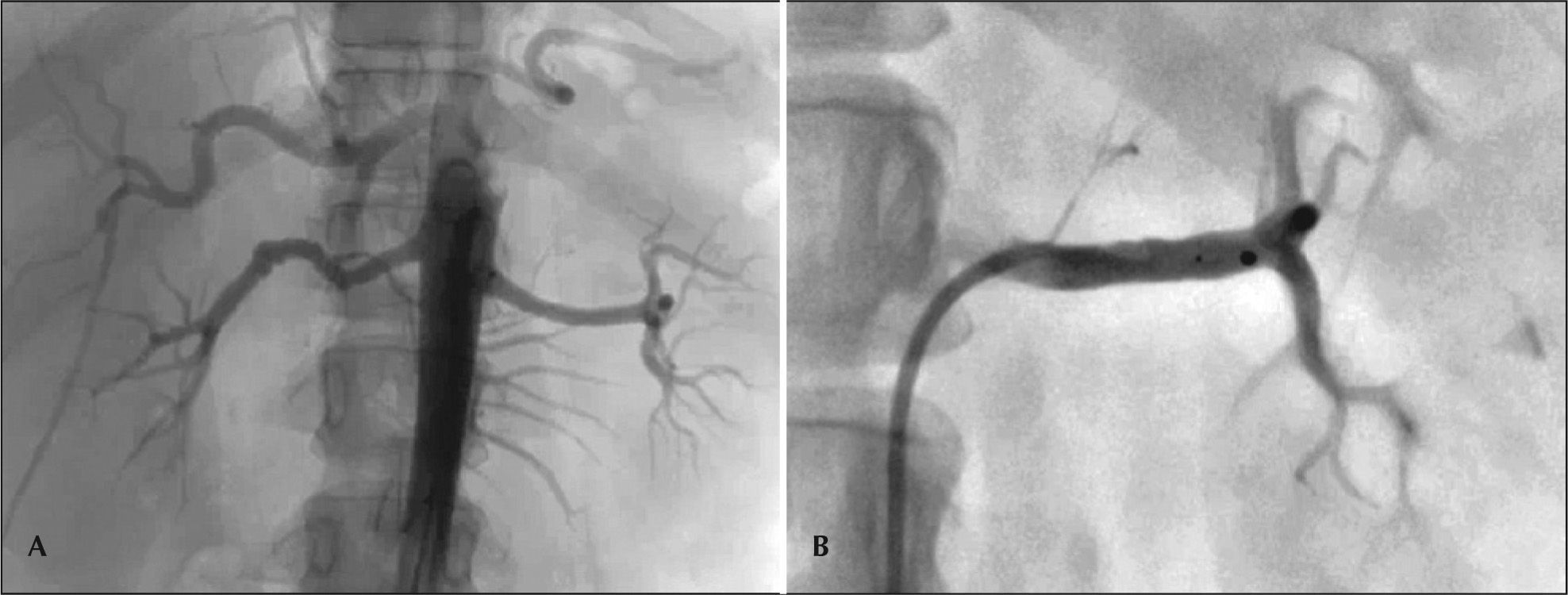
ProcedureAn abdominal aortography was performed by femoral approach to assess the renal arteries and the technical feasibility of the procedure. Subsequently, the renal arteries were selectively catheterized, and the Symplicity® catheter was advanced within the vessel. Four to eight ablations were applied from the distal to the proximal portion, 5mm apart, with duration of 120 seconds in both renal arteries (Figure 3). Each radiofrequency application has a maximum of 8W and increases in impedance and temperature are controlled by the system in order to avoid tissue injury due to overheating. All patients were anticoagulated with un-fractionated heparin (70 U/kg until an activated clotting time >250s was attained) during the procedure, and analgesia with benzodiazepines and opioids was used for pain control.
Study DesignThis was a prospective, single-arm, observational multicenter study that included consecutive patients undergoing renal sympathetic denervation between March and December 2012 at three centers in Venezu-ela. The primary outcome was the decrease of systolic blood pressure at 30 days of follow-up. The secondary outcome was the occurrence of any procedure-related adverse event.
The criteria for patient inclusion were: age >18years with resistant SAH, defined as systolic blood pressure >160mmHg despite adequate use of three or more antihypertensive agents (at least one diuretic), or patients taking>four antihypertensive medications. The assessment of renal artery anatomy was recommended before the procedure using renal artery Doppler and/or imaging studies (computed tomography [CT] or magnetic resonance imaging [MRI]) or aortography.
Patients with glomerular filtration rate<45mL/ min/1.73m2 (calculated by the Cockcroft-Gault formula), 15 renal artery<4mm in diameter, < 20mm in length, previous interventions in renal arteries, renal artery stenosis, and acute coronary syndrome or stroke<six months were excluded. Procedural success was defined as attaining the procedure in both renal arteries without procedure-related complications.
Patient follow-up was performed by their respective attending physicians, who were instructed not to modify the antihypertensive treatment, if clinically possible,
within the first 30 days after the procedure, and to report an average of three blood pressure measure-ments obtained at the office at 30 days of follow-up, according to the recommended guidelines.5
This study was performed in accordance with the Declaration of Helsinki and the principles of good clini-cal practice. All patients signed an informed consent before the procedure.
Statistical analysisQuantitative variables are shown as means and standard deviations, and qualitative variables are shown as percentages. Student’s t-test was used to compare quantitative variables. A P-value<0.05 was considered significant. Statistical analysis was performed with SPSS software, version 16.0 (SPSS Inc., Chicago, USA).
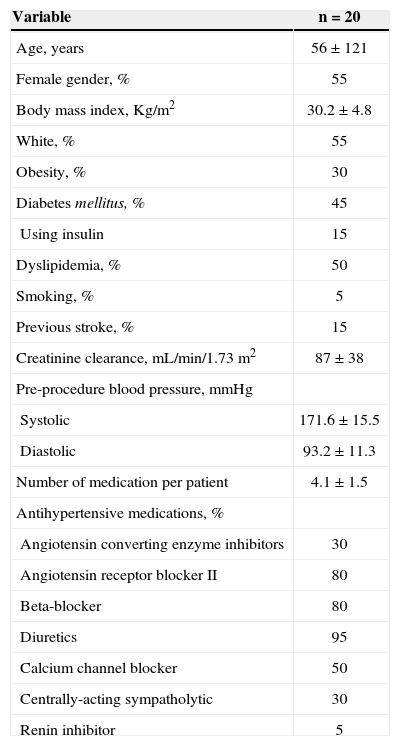
RESULTSThis analysis included the first 20 patients undergoing renal sympathetic denervation. The mean age was 56±12.1years, 55% were females, and 55% were whites. Blood pressure (BP) before the procedure was 171.6/93.2±15.5/11.3mmHg, using 4.1±1.5 anti-hypertensive drugs per patient (Table 1).
Baseline clinical characteristics
| Variable | n=20 |
|---|---|
| Age, years | 56±121 |
| Female gender, % | 55 |
| Body mass index, Kg/m2 | 30.2±4.8 |
| White, % | 55 |
| Obesity, % | 30 |
| Diabetes mellitus, % | 45 |
| Using insulin | 15 |
| Dyslipidemia, % | 50 |
| Smoking, % | 5 |
| Previous stroke, % | 15 |
| Creatinine clearance, mL/min/1.73m2 | 87±38 |
| Pre-procedure blood pressure, mmHg | |
| Systolic | 171.6±15.5 |
| Diastolic | 93.2±11.3 |
| Number of medication per patient | 4.1±1.5 |
| Antihypertensive medications, % | |
| Angiotensin converting enzyme inhibitors | 30 |
| Angiotensin receptor blocker II | 80 |
| Beta-blocker | 80 |
| Diuretics | 95 |
| Calcium channel blocker | 50 |
| Centrally-acting sympatholytic | 30 |
| Renin inhibitor | 5 |
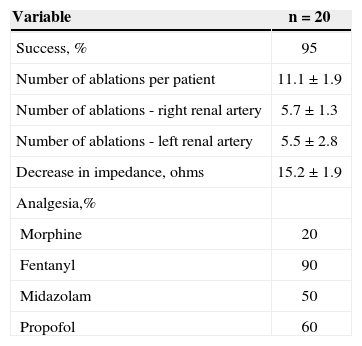
Regarding the characteristics of the procedure, success rate was 95%; 11.1±1.9 ablations were applied per patient, 5.7±1.3 in the right renal artery and 5.5±2.8 in the left renal artery, and the mean decrease in impedance was 15.2±1.9 ohms (Table 2).
Characteristics of the procedure
| Variable | n=20 |
|---|---|
| Success, % | 95 |
| Number of ablations per patient | 11.1±1.9 |
| Number of ablations - right renal artery | 5.7±1.3 |
| Number of ablations - left renal artery | 5.5±2.8 |
| Decrease in impedance, ohms | 15.2±1.9 |
| Analgesia,% | |
| Morphine | 20 |
| Fentanyl | 90 |
| Midazolam | 50 |
| Propofol | 60 |
Regarding the primary outcome, a decrease of 29±21mmHg (P=0.009) was observed in the systolic blood pressure 30 days after the procedure (Figure 4). Regarding the secondary safety outcome, there were no complications related to the procedure or the adverse events after 30 days of follow-up. Among the studied population, 80% had a decrease of at least 10mmHg in systolic blood pressure, and 68% of patients had blood pressure values within the targets proposed by the guidelines.5
DISCUSSIONIn the initial experience with the percutaneous renal sympathetic denervation system for the control of resistant hypertension, the authors observed a significant decrease in systolic blood pressure after 30 days. There were no complications related to the procedure.
Symplicity HTN-1, a single-arm trial that included 45 patients undergoing renal sympathetic denervation, observed a decrease of 14mmHg and 22mmHg at 30 days and six months of follow-up, respectively.13
Subsequently, the Symplicity HTN-2 trial randomized 106 patients with resistant SAH, in which the group allocated for renal sympathetic denervation had a BP of 178/96mmHg with the use of 5.2 antihypertensive medications. Six months after the procedure, a significant decrease of 32mmHg was observed in the group submit-ted to renal sympathetic denervation, when compared with the clinical treatment group.14 In the scenario of real-world clinical practice, the Venezuelan Symplicity registry presented a decrease of 34mmHg at 30 days of follow-up.16 In the present group, the decrease in BP at 30 days was 29±21mmHg, consistent with in the results of the Symplicity HTN-1 and HTN-2 trials and the Venezuelan Symplicity registry.13,14,16
Regarding safety, the complication rates during the procedure are low, mainly due the guide-catheter hand-ling during renal artery catheterization. In the Symplicity HTN-1 trial, among the 45 treated patients, one had re-nal artery dissection during catheterization with no need for additional treatment.13 In the Symplicity HTN-2 trial, there were no major adverse events and only one patient had lower back pain, which resolved spontaneously after 30 days, and 13% of the cases had bradycardia during the procedure, which was successfully reversed using atropine.14 It is important to emphasize that, although this is the initial phase of the learning curve with the study device, procedure-related adverse events were not observed. Except for one case in which it was not pos-sible to catheterize the renal artery due to extreme aortic tortuosity, all other cases were successful.
Renal sympathetic denervation has been shown an additional benefit besides the lowering of blood pressure. Brandt et al.17 demonstrated a significant reduction in left ventricular mass and improved diastolic function in patients undergoing renal sympathetic denervation. It is noteworthy that such findings were independent from the reduction in blood pressure.
Mahfoud et al.18 evaluated the effect of renal sympathetic denervation in diabetic patients, finding, at the three-month follow-up, a decrease in fasting glucose levels, from 118±3.4±mg/dL to 108±3.8mg/dL (P=0.039); insulin levels, from 20.8±3IU/ mL to 9.3±2.5IU/mL (P=0.006); and C peptide, from 5.3±0.6ng/mL to 3±0.9ng/mL (P=0.002). These findings suggest that renal sympathetic denerva-tion, in addition to lowering blood pressure, improves glucose metabolism and insulin sensitivity. Currently, new renal sympathetic denervation effects are being tested on heart failure, sleep apnoea, atrial fibrillation, and pulmonary hypertension.
Study limitationsThe main limitations of this study were the small sample size and the fact that it was an observational study; therefore, it is necessary to confirm its findings in larger populations and, preferably, in a randomized fashion. However, the results were similar to those observed in the largest recently published studies,13,14 which confers reliability to the present findings. Clinical follow-up of patients was performed by their attending physicians, who, despite strictly instructed not to modify the antihypertensive treatment within 30 days and to report any complaint or adverse effect, may have failed to follow such recommendations. Follow-up was con-ducted through mean blood pressure measured at the office, instead of 24-hour ambulatory blood pressure monitoring, a method that presents a better correlation with target-organ damage.19 Finally, although the results related to the decrease in BP values are promising, late follow-up is essential to verify the maintenance of these acquired benefits.
CONCLUSIONSIn this observational study, renal sympathetic denervation guided by Symplicity® catheter promoted decrease in systolic blood pressure in patients with resistant hypertension. This initial experience was shown to be safe, with no intraprocedure-related adverse events and at the 30-day follow-up.
CONFLICTS OF INTERESTCarlos Adolfo Collet is a proctor and speaker for Medtronic (Minneapolis, USA). Guilherme F. Attizzani is a consultant for St. Jude Medical (St. Paul, United States). The remaining authors declare to have no conflicts of interest.