The knowledge of risk factors related to vascular access complications in patients undergoing early invasive strategy allows the adoption of methods to minimize them.
MethodsWe performed a subanalysis of the ARISE study, aiming to identify predictors of vascular complications in patients randomized to the radial or femoral techniques with the use of vascular closure device (VCD).
ResultsA total of 240 patients with a mean age of 63.0 ± 10.7 years were included, with 30.8% of diabetics. Except for a higher prevalence of women in the radial group, there were no clinical differences between the groups. Percutaneous coronary intervention was performed in 86.7% of the cases. The rate of vascular complications after 30 days was 13.3% in the radial group, due to hematoma > 5cm (6.7%) and asymptomatic artery occlusion (5.8%), and 12.5% in femoral group, due to hematoma > 5cm, without significant difference. The following were identified as risk factors for vascular access complications: body mass index (BMI), previous stroke, longer duration of the procedure, and VCD failure. At the stratified analysis, female gender and high or very high-risk CRUSADE score were predictors of complications only for the femoral group. In the multivariate model, the factors that remained significant were BMI and VCD failure.
ConclusionsThe radial and femoral techniques, with the use of VCD, shared variables that were predictors of complications. Risk factors, such as female gender and high-risk CRUSADE score, were attenuated by the use of the radial technique.
O conhecimento dos fatores de risco relacionados às complicações do acesso vascular em pacientes submetidos à estratégia invasiva precoce permite adotar estratégias capazes de minimizá-las.
MétodosRealizamos subanálise do estudo ARISE, com o objetivo de identificar preditores de complicações vasculares em pacientes randomizados para as técnicas radial ou femoral com emprego de dispositivo de oclusão vascular (DOV).
ResultadosForam incluídos 240 pacientes, com média de idade de 63,0 ± 10,7 anos, sendo 30,8% diabéticos e, exceto pela maior prevalência de mulheres no grupo radial, não foram observadas diferenças clínicas entre os grupos. Intervenção coronária percutânea foi realizada em 86,7% dos casos. A taxa de complicações vasculares aos 30 dias foi de 13,3% no grupo radial, à custa de hematomas > 5cm (6,7%) e oclusão arterial assintomática (5,8%), e de 12,5% no grupo femoral, à custa de hematomas > 5cm, sem diferença significativa. Foram identificados como fatores de risco para complicações do acesso vascular o índice de massa corporal (IMC), o acidente vascular encefálico prévio, a maior duração do procedimento e o insucesso do DOV. Pela análise estratificada, o sexo feminino e o escore CRUSADE de alto ou muito alto risco foram variáveis preditoras de complicações apenas para o grupo femoral. No modelo multivariado, os fatores que permaneceram significantes foram o IMC e o insucesso do DOV.
ConclusõesAs técnicas radial e femoral, com o emprego de DOV, compartilharam variáveis preditoras de complicações. Fatores de risco, como sexo feminino e escore CRUSADE de alto risco, foram atenuados pela utilização da técnica radial.
The prevalence of severe hemorrhagic complications in patients with acute coronary syndrome (ACS) can reach up to 5%, with a potential prognostic impact.1 Although intracranial or gastrointestinal bleeding episodes are associated with worse outcomes, arterial access-related bleeding in invasive coronary procedures increases the risk of mortality by up to 1.7-fold.2,3
In this sense, knowledge of risk factors related to the occurrence of vascular complications in patients undergoing percutaneous coronary intervention (PCI) in current practice allows the adoption of strategies to minimize their prevalence.4 The ARISE (AngioSeal versus Radial approach In acute coronary Syndrome) study evaluated the incidence of complications at 30 days in the puncture site in patients with ACS without ST elevation undergoing early invasive strategy.5
The aim of the present subanalysis of the ARISE study was to identify the predictors of complications using the two types of arterial access, the radial or femoral approach, using a vascular closure device (VCD) to attain hemostasis.
MethodsThe complete description of the ARISE study methods has been previously published.5 In brief, it was a prospective, randomized, single-center, comparative, non-inferiority clinical trial between the radial technique using the TR Band® selective compression device (Terumo Medical, Tokyo, Japan) and the femoral technique using the Angio-SealTM VCD (St. Jude Medical, St. Paul, USA) in reducing complications related to arterial puncture site at 30 days of follow-up.
Among the arterial access-related complications, the following were considered: hematoma ≥ 5cm, severe bleeding type 3 or 5 according to the Bleeding Academic Research Consortium (BARC) criteria,6 pseudoaneurysm, retroperitoneal hemorrhage, arterial occlusion, adjacent nerve damage, limb ischemia, compartment syndrome, arteriovenous fistula, infection, or need for vascular repair surgery.
Statistical analysisThe independent variables assessed were gender, age, body mass index (BMI), diabetes mellitus, systemic arterial hypertension, dyslipidemia, smoking, previous cardiac or cerebrovascular events (acute myocardial infarction, PCI, coronary artery bypass graft surgery and stroke), chronic renal failure, chronic peripheral arterial insufficiency, GRACE (Global Registry of Acute Coronary Events) score, CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines) score, introducer sheath diameter, number of catheters, contrast volume, total duration of the procedure, fluoroscopy time, sedation, antithrombotic therapy, ventricular ejection fraction, and success of the hemostasis device.
The effect of the independent variables on the outcome of interest was assessed in three different ways, namely, considering the overall group, analyzing the radial and femoral groups separately (stratified analysis), and considering the overall group, while maintaining the type of access as the control variable. For that purpose, the interaction terms between the assessed variable and the group were analyzed, considering the possibility that the predictors were not the same for the different vascular access types.
In the three approaches, the isolated effect of each variable was initially assessed through simple logistic regression models (univariate analysis). Then, the variables with p < 0.20 in the univariate analysis were evaluated simultaneously in a multiple logistic regression model (multivariate analysis). For qualitative independent variables, the category with the lowest frequency of complications was considered as the reference. The results were expressed as odds ratios (OR) and 95% confidence intervals (95% CI). The statistical program used was the IBM Statistical Package for Social Sciences (SPSS), version 19.0.
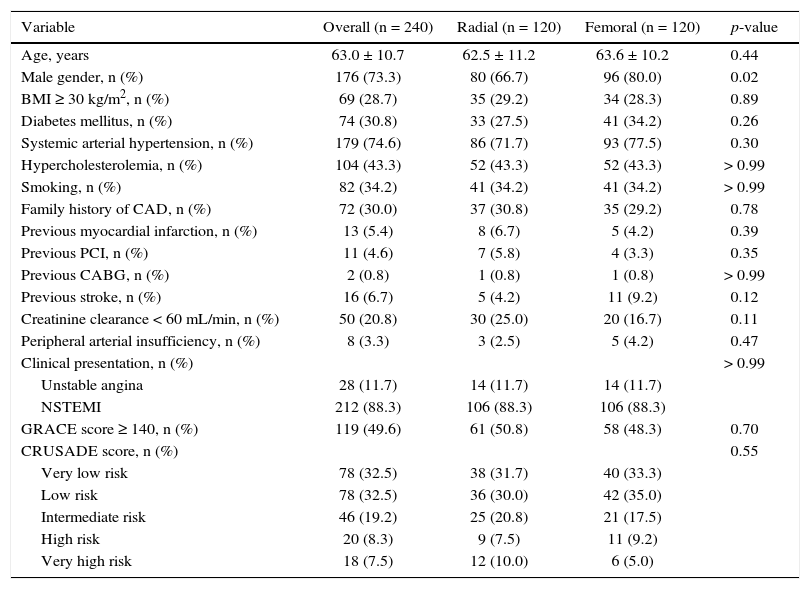
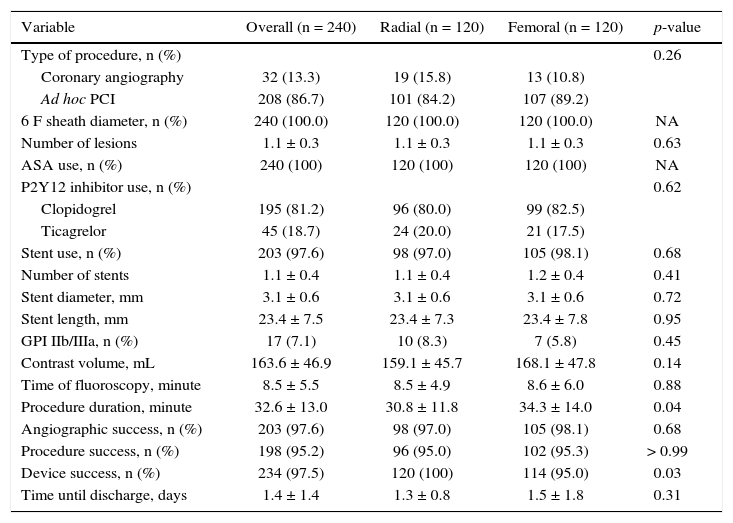
ResultsFrom July 2012 to March 2015, a total of 240 patients were included in the study, randomized at a 1:1 ratio to radial or femoral access. The mean age was 63.0 ± 10.7 years; 74 (30.8%) were diabetics and, except for a higher prevalence of women (33.3% vs. 20%) in the radial group, no significant differences were observed among the groups (Table 1). PCI was performed in 86.7% of cases, and the characteristics of procedures are shown in Table 2. The mean duration of procedures was higher for the group of patients in whom the femoral access was used (30.8 ± 11.8minutes vs. 34.3 ± 14minutes; p = 0.04).
Basal clinical characteristics.
| Variable | Overall (n = 240) | Radial (n = 120) | Femoral (n = 120) | p-value |
|---|---|---|---|---|
| Age, years | 63.0 ± 10.7 | 62.5 ± 11.2 | 63.6 ± 10.2 | 0.44 |
| Male gender, n (%) | 176 (73.3) | 80 (66.7) | 96 (80.0) | 0.02 |
| BMI ≥ 30 kg/m2, n (%) | 69 (28.7) | 35 (29.2) | 34 (28.3) | 0.89 |
| Diabetes mellitus, n (%) | 74 (30.8) | 33 (27.5) | 41 (34.2) | 0.26 |
| Systemic arterial hypertension, n (%) | 179 (74.6) | 86 (71.7) | 93 (77.5) | 0.30 |
| Hypercholesterolemia, n (%) | 104 (43.3) | 52 (43.3) | 52 (43.3) | > 0.99 |
| Smoking, n (%) | 82 (34.2) | 41 (34.2) | 41 (34.2) | > 0.99 |
| Family history of CAD, n (%) | 72 (30.0) | 37 (30.8) | 35 (29.2) | 0.78 |
| Previous myocardial infarction, n (%) | 13 (5.4) | 8 (6.7) | 5 (4.2) | 0.39 |
| Previous PCI, n (%) | 11 (4.6) | 7 (5.8) | 4 (3.3) | 0.35 |
| Previous CABG, n (%) | 2 (0.8) | 1 (0.8) | 1 (0.8) | > 0.99 |
| Previous stroke, n (%) | 16 (6.7) | 5 (4.2) | 11 (9.2) | 0.12 |
| Creatinine clearance < 60 mL/min, n (%) | 50 (20.8) | 30 (25.0) | 20 (16.7) | 0.11 |
| Peripheral arterial insufficiency, n (%) | 8 (3.3) | 3 (2.5) | 5 (4.2) | 0.47 |
| Clinical presentation, n (%) | > 0.99 | |||
| Unstable angina | 28 (11.7) | 14 (11.7) | 14 (11.7) | |
| NSTEMI | 212 (88.3) | 106 (88.3) | 106 (88.3) | |
| GRACE score ≥ 140, n (%) | 119 (49.6) | 61 (50.8) | 58 (48.3) | 0.70 |
| CRUSADE score, n (%) | 0.55 | |||
| Very low risk | 78 (32.5) | 38 (31.7) | 40 (33.3) | |
| Low risk | 78 (32.5) | 36 (30.0) | 42 (35.0) | |
| Intermediate risk | 46 (19.2) | 25 (20.8) | 21 (17.5) | |
| High risk | 20 (8.3) | 9 (7.5) | 11 (9.2) | |
| Very high risk | 18 (7.5) | 12 (10.0) | 6 (5.0) |
BMI: body mass index; CAD: coronary artery disease; PCI: percutaneous coronary intervention; CABG: coronary artery bypass grafting surgery; NSTEMI: non-ST myocardial infarction.
Angiographic and procedure characteristics.
| Variable | Overall (n = 240) | Radial (n = 120) | Femoral (n = 120) | p-value |
|---|---|---|---|---|
| Type of procedure, n (%) | 0.26 | |||
| Coronary angiography | 32 (13.3) | 19 (15.8) | 13 (10.8) | |
| Ad hoc PCI | 208 (86.7) | 101 (84.2) | 107 (89.2) | |
| 6 F sheath diameter, n (%) | 240 (100.0) | 120 (100.0) | 120 (100.0) | NA |
| Number of lesions | 1.1 ± 0.3 | 1.1 ± 0.3 | 1.1 ± 0.3 | 0.63 |
| ASA use, n (%) | 240 (100) | 120 (100) | 120 (100) | NA |
| P2Y12 inhibitor use, n (%) | 0.62 | |||
| Clopidogrel | 195 (81.2) | 96 (80.0) | 99 (82.5) | |
| Ticagrelor | 45 (18.7) | 24 (20.0) | 21 (17.5) | |
| Stent use, n (%) | 203 (97.6) | 98 (97.0) | 105 (98.1) | 0.68 |
| Number of stents | 1.1 ± 0.4 | 1.1 ± 0.4 | 1.2 ± 0.4 | 0.41 |
| Stent diameter, mm | 3.1 ± 0.6 | 3.1 ± 0.6 | 3.1 ± 0.6 | 0.72 |
| Stent length, mm | 23.4 ± 7.5 | 23.4 ± 7.3 | 23.4 ± 7.8 | 0.95 |
| GPI IIb/IIIa, n (%) | 17 (7.1) | 10 (8.3) | 7 (5.8) | 0.45 |
| Contrast volume, mL | 163.6 ± 46.9 | 159.1 ± 45.7 | 168.1 ± 47.8 | 0.14 |
| Time of fluoroscopy, minute | 8.5 ± 5.5 | 8.5 ± 4.9 | 8.6 ± 6.0 | 0.88 |
| Procedure duration, minute | 32.6 ± 13.0 | 30.8 ± 11.8 | 34.3 ± 14.0 | 0.04 |
| Angiographic success, n (%) | 203 (97.6) | 98 (97.0) | 105 (98.1) | 0.68 |
| Procedure success, n (%) | 198 (95.2) | 96 (95.0) | 102 (95.3) | > 0.99 |
| Device success, n (%) | 234 (97.5) | 120 (100) | 114 (95.0) | 0.03 |
| Time until discharge, days | 1.4 ± 1.4 | 1.3 ± 0.8 | 1.5 ± 1.8 | 0.31 |
PCI: percutaneous coronary intervention; ASA: acetylsalicylic acid; GPI: glycoprotein inhibitor.
There was no need for crossover between the techniques. Hemostasis with TR Band® was obtained in 100% of the radial approach procedures; patent antegrade flow was demonstrated by oximetric curve in 102 patients (85%). Of the seven cases of asymptomatic radial artery occlusion, all showed flow patency at the plethysmography test, performed immediately after the bracelet was applied. In six (5%) patients from the femoral group, the Angio-SealTM device was not enough to achieve hemostasis, which required additional manual compression for over 10minutes.
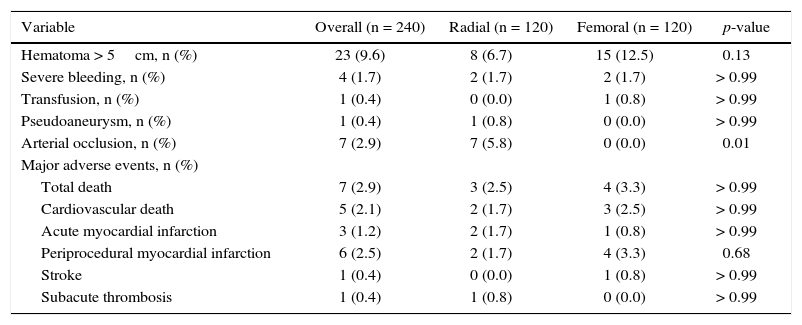
The rate of vascular complications in the arterial puncture site at 30 days was 13.3% in the radial group, due to hematoma > 5cm (6.7%) and asymptomatic occlusion of the radial artery (5.8%); this rate was 12.5% in the femoral group, due to hematoma > 5cm, with no difference between groups (Table 3). Severe bleeding occurred in 1.7% of both groups. There were no cases of arteriovenous fistula, retroperitoneal hematoma, compartment syndrome, limb ischemia, nerve damage, or need for vascular repair surgery.
Vascular complications at the puncture site and severe adverse events at 30 days.
| Variable | Overall (n = 240) | Radial (n = 120) | Femoral (n = 120) | p-value |
|---|---|---|---|---|
| Hematoma > 5cm, n (%) | 23 (9.6) | 8 (6.7) | 15 (12.5) | 0.13 |
| Severe bleeding, n (%) | 4 (1.7) | 2 (1.7) | 2 (1.7) | > 0.99 |
| Transfusion, n (%) | 1 (0.4) | 0 (0.0) | 1 (0.8) | > 0.99 |
| Pseudoaneurysm, n (%) | 1 (0.4) | 1 (0.8) | 0 (0.0) | > 0.99 |
| Arterial occlusion, n (%) | 7 (2.9) | 7 (5.8) | 0 (0.0) | 0.01 |
| Major adverse events, n (%) | ||||
| Total death | 7 (2.9) | 3 (2.5) | 4 (3.3) | > 0.99 |
| Cardiovascular death | 5 (2.1) | 2 (1.7) | 3 (2.5) | > 0.99 |
| Acute myocardial infarction | 3 (1.2) | 2 (1.7) | 1 (0.8) | > 0.99 |
| Periprocedural myocardial infarction | 6 (2.5) | 2 (1.7) | 4 (3.3) | 0.68 |
| Stroke | 1 (0.4) | 0 (0.0) | 1 (0.8) | > 0.99 |
| Subacute thrombosis | 1 (0.4) | 1 (0.8) | 0 (0.0) | > 0.99 |
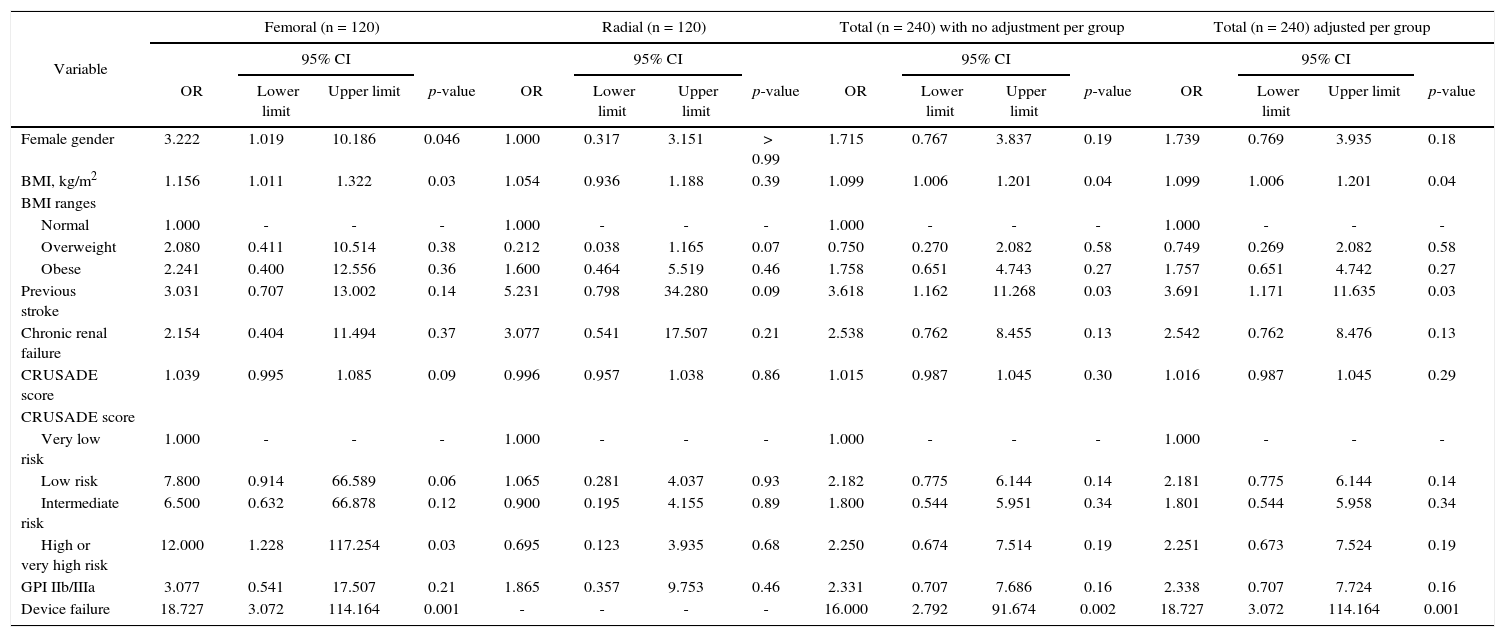
The following were identified as risk factors for vascular access complications: BMI, previous stroke, longer duration of the procedure, and VCD failure. At the stratified analysis, female gender and high or very high risk CRUSADE score were complication predictors only for the femoral group, although significant interaction effects were not identified (Table 4). Variables with p < 0.20 in the univariate analysis were assessed together in the multivariate model. The factors that remained significant were BMI (odds ratio − OR = 1.132; 95% CI: 1.021-1.254 per +1kg/m2) and VCD failure (OR = 17.147; 95% CI: 1.825-161.076).
Univariate analysis results - factors associated with the occurrence of complications.
| Variable | Femoral (n = 120) | Radial (n = 120) | Total (n = 240) with no adjustment per group | Total (n = 240) adjusted per group | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | 95% CI | 95% CI | |||||||||||||
| OR | Lower limit | Upper limit | p-value | OR | Lower limit | Upper limit | p-value | OR | Lower limit | Upper limit | p-value | OR | Lower limit | Upper limit | p-value | |
| Female gender | 3.222 | 1.019 | 10.186 | 0.046 | 1.000 | 0.317 | 3.151 | > 0.99 | 1.715 | 0.767 | 3.837 | 0.19 | 1.739 | 0.769 | 3.935 | 0.18 |
| BMI, kg/m2 | 1.156 | 1.011 | 1.322 | 0.03 | 1.054 | 0.936 | 1.188 | 0.39 | 1.099 | 1.006 | 1.201 | 0.04 | 1.099 | 1.006 | 1.201 | 0.04 |
| BMI ranges | ||||||||||||||||
| Normal | 1.000 | - | - | - | 1.000 | - | - | - | 1.000 | - | - | - | 1.000 | - | - | - |
| Overweight | 2.080 | 0.411 | 10.514 | 0.38 | 0.212 | 0.038 | 1.165 | 0.07 | 0.750 | 0.270 | 2.082 | 0.58 | 0.749 | 0.269 | 2.082 | 0.58 |
| Obese | 2.241 | 0.400 | 12.556 | 0.36 | 1.600 | 0.464 | 5.519 | 0.46 | 1.758 | 0.651 | 4.743 | 0.27 | 1.757 | 0.651 | 4.742 | 0.27 |
| Previous stroke | 3.031 | 0.707 | 13.002 | 0.14 | 5.231 | 0.798 | 34.280 | 0.09 | 3.618 | 1.162 | 11.268 | 0.03 | 3.691 | 1.171 | 11.635 | 0.03 |
| Chronic renal failure | 2.154 | 0.404 | 11.494 | 0.37 | 3.077 | 0.541 | 17.507 | 0.21 | 2.538 | 0.762 | 8.455 | 0.13 | 2.542 | 0.762 | 8.476 | 0.13 |
| CRUSADE score | 1.039 | 0.995 | 1.085 | 0.09 | 0.996 | 0.957 | 1.038 | 0.86 | 1.015 | 0.987 | 1.045 | 0.30 | 1.016 | 0.987 | 1.045 | 0.29 |
| CRUSADE score | ||||||||||||||||
| Very low risk | 1.000 | - | - | - | 1.000 | - | - | - | 1.000 | - | - | - | 1.000 | - | - | - |
| Low risk | 7.800 | 0.914 | 66.589 | 0.06 | 1.065 | 0.281 | 4.037 | 0.93 | 2.182 | 0.775 | 6.144 | 0.14 | 2.181 | 0.775 | 6.144 | 0.14 |
| Intermediate risk | 6.500 | 0.632 | 66.878 | 0.12 | 0.900 | 0.195 | 4.155 | 0.89 | 1.800 | 0.544 | 5.951 | 0.34 | 1.801 | 0.544 | 5.958 | 0.34 |
| High or very high risk | 12.000 | 1.228 | 117.254 | 0.03 | 0.695 | 0.123 | 3.935 | 0.68 | 2.250 | 0.674 | 7.514 | 0.19 | 2.251 | 0.673 | 7.524 | 0.19 |
| GPI IIb/IIIa | 3.077 | 0.541 | 17.507 | 0.21 | 1.865 | 0.357 | 9.753 | 0.46 | 2.331 | 0.707 | 7.686 | 0.16 | 2.338 | 0.707 | 7.724 | 0.16 |
| Device failure | 18.727 | 3.072 | 114.164 | 0.001 | - | - | - | - | 16.000 | 2.792 | 91.674 | 0.002 | 18.727 | 3.072 | 114.164 | 0.001 |
The identification of predictors of vascular access complications according to the technique used allows for the individualization of conducts and decision-making, guided by the search for the efficacy-safety binomial. In the ARISE clinical trial, the systematic use of VCD in patients submitted to invasive stratification through femoral access showed to be non-inferior to the radial access regarding the incidence of vascular complications related to the arterial puncture site at 30 days. In the present sub-study, BMI and VCD failure were predictors of complications at the multivariate analysis. As for the stratified model, female gender and high CRUSADE score were correlated with complications through the femoral access only, demonstrating a patient profile prone to benefit from the radial technique.
In a Danish registry involving 23,870 patients undergoing invasive coronary procedures through femoral access (35% PCI), in which 86% of the patients used VCD, severe vascular access complications were reported in 0.54% of cases. Despite the low incidence of complications, there was a predominance of pseudoaneurysms, arterial occlusions requiring limb amputation, and retroperitoneal hematomas. The following were identified as predictors of events: female gender, chronic peripheral arterial insufficiency, left femoral access, BMI < 18.5kg/m2, and manual compression.7 The analysis of 10,676 procedures performed through radial access in a highly-experienced Italian center showed a rate of 0.41% of complications related to radial access, of which 0.10% were categorized as severe, including compartment syndrome, pseudoaneurysm, mycotic aneurysm, and hematoma with a decrease in hemoglobin > 3g/dL, whose predictors were older age, female gender, and previous coronary artery bypass graft surgery.8
The clinical presentation of ACS in patients undergoing PCI translates into high risk of bleeding and ischemic outcomes, given the greater anatomical complexity of the lesions, the use of more aggressive antithrombotic therapy, including the use of IIb/IIIa glycoprotein inhibitors, and less frequent use of the radial approach and VCD to achieve hemostasis through the femoral access.9 Although an approximate 20% reduction in the rate of bleeding complications related to invasive coronary procedures was observed, it was due mainly to the use of drugs with better safety profile, demonstrating a gap in the adoption of other strategies aimed at reducing bleeding, especially those related to the vascular access use.10
The radial technique, performed by a proficient interventionist, has been established as the chosen route for invasive ACS stratification. Sequential analysis of 17 randomized trials involving 19,328 patients showed a significant reduction in mortality of 27% and of 40% in severe bleeding when compared with the femoral technique.11 However, the femoral technique still predominates as the preferred access, being used in Brazil in approximately 70% of cases.12 In this context, it is necessary to adopt measures to provide greater safety during the procedure. A contemporary analysis including 85,048 procedures performed through femoral access, of which 28,528 used VCD, showed that compared to manual compression, the former resulted in significant reduction of vascular complications and need for transfusion.13
The present study has limitations. The main limitation is the small sample size, making the estimates more inaccurate, in addition to representing the experience of a single center familiarized with the radial approach. The complication rate for both groups was high in terms of percentage, but the main complications observed were hematoma > 5cm and asymptomatic occlusion of the radial artery, whose prognostic impact has not been well established. In a population that predominantly shows low-to-moderate risk for bleeding, there was no occurrence of pseudoaneurysm, arteriovenous fistula, retroperitoneal hematoma, or infection in the VCD group.
ConclusionsVascular-access related complications are common in patients undergoing early invasive strategy. The radial and femoral techniques with vascular closure device share variables that are predictors of complications, such as body mass index, previous stroke and longer duration of the procedure. Risk factors, such as female gender and high CRUSADE score, are attenuated by the use of the first option.
Funding sourcesNone declared.
Conflicts of interestThe authors declare no conflicts of interest.
Peer review under the responsibility of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.