Spontaneous coronary artery dissection is a rare cause of acute coronary syndrome and its diagnosis is made by necropsy in more than 70% of the cases. Optimal treatment is still uncertain, and the treatment options are percutaneous coronary intervention, coronary artery bypass surgery and medical therapy. The objective of this study was to evaluate the clinical characteristics, treatment modalities and outcome of a series of cases with spontaneous coronary artery dissection.
MethodsRetrospective, single-center study, based on the analysis of the database at a high-complexity cardiology service.
ResultsWe identified 25 patients with spontaneous coronary artery dissection, 56% were female, with a mean age of 48.8±10 years. Only 24% had no risk factor for atherosclerosis and in 92% of the cases, the clinical presentation was of acute coronary syndrome. The left anterior descending artery was the most commonly affected vessel (48.1%) and there was only one case involving multiple vessels. The conservative approach was used in 56%, percutaneous coronary intervention in 40% and coronary artery bypass grafting in 4%. The in-hospital and late event-free survival was 92% and 84.2%, respectively.
ConclusionsSpontaneous coronary artery dissection predominated in young women, with at least one risk factor for coronary artery disease. The choice of different therapeutic strategies confirms the still controversial nature of the optimal approach for spontaneous coronary artery dissection. We believe that individualized therapy is still the optimal modality.
Dissecção Espontânea de Artéria Coronária: Abordagem Terapêutica e Desfechos de Uma Série Consecutiva de Casos
IntroduçãoA dissecção espontânea de artéria coronária é causa rara de síndrome coronariana aguda e, em mais de 70% das vezes, o diagnóstico é feito por meio de necrópsia. O tratamento ideal ainda é incerto, sendo a intervenção coronária percutânea, a cirurgia de revascularização miocárdica e o tratamento clínico as opções terapêuticas. O objetivo deste trabalho foi avaliar as características clínicas, o tratamento e a evolução de uma série de casos de dissecção espontânea de artéria coronária.
MétodosEstudo retrospectivo, unicêntrico, baseado em análise de banco de dados de um serviço de alta complexidade em cardiologia.
ResultadosIdentificamos 25 pacientes com dissecção espontânea de artéria coronária dos quais 56% eram do gênero feminino, com idade de 48,8±10 anos. Apenas 24% não apresentaram fator de risco para aterosclerose e, em 92% dos casos, o quadro clínico foi de síndrome coronária aguda. A artéria descendente anterior foi o vaso mais acometido (48%) e houve apenas um caso envolvendo múltiplos vasos. A estratégia conservadora foi realizada em 56%, a intervenção coronária percutânea em 40% e a revascularização miocárdica em 4%. A taxa livre de eventos hospitalares e tardios foi de 92 e 84,2%, respectivamente.
ConclusõesA dissecção espontânea de artéria coronária foi predominante em mulheres jovens, com pelo menos um fator de risco para doença arterial coronariana. A escolha de diferentes estratégias terapêuticas confirma a natureza ainda controversa da abordagem ideal da dissecção espontânea de artéria coronária. Acreditamos que o tratamento ideal ainda seja o individualizado.
The importance of the discussion on coronary artery disease (CAD) in contemporary society is attested by the endemic number of people affected by this condition. Cardiovascular diseases are still the leading causes of death in Brazil, representing more than 40% of deaths.1 CAD is most commonly related to atherosclerosis, but congenital anomalies of the coronary artery, coronary arteritides associated with systemic vasculitis, fibromuscular dysplasia, and spontaneous coronary artery dissection (SCAD) are other causes to consider.
The first case of SCAD was described by Pretty in 1931, found in autopsy.2 This is a rare cause of acute myocardial ischemia, and the diagnosis is still established by autopsy in over 70% of cases.3,4 It occurs most often in young patients, predominantly females. The most common clinical presentation is that of an acute coronary syndrome. The left anterior descending artery is the more affected vessel, and multivessel dissection occurs in approximately 20% of cases; recurrence at ten years occurs in one-third of patients. Recent estimates reported 7.7% mortality at ten years.5-7
The aim of this study was to describe the incidence, clinical features, therapeutic modalities, and outcome of patients in a case series of SCAD.
METHODSThis was a retrospective, single-center study conducted at a high-complexity tertiary care cardiology service. The research was based on an analysis of the database, clinical record reviews, and phone contacts.
Study populationThe database of the Hemodynamics Service, Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo (InCor-HCFMUSP) was searched using the keyword “dissection”, between March of 2001 and June of 2012, and 901 potential patients were obtained. Individual assessments clinical records and coronary angiographies were performed, during which the other diagnoses were excluded, such as coronary atherosclerosis, iatrogenic traumatic dissection, stent edge dissection, and other arterial dissections. Overall, 25 patients with compatible clinical history and coronary angiography for SCAD were found. The angiographic diagnosis of coronary dissection was obtained through an evaluation by at least two hemodynamicists.
Data collectionDemographic characteristics, clinical presentation, distribution of CAD, therapeutic modality, and in- and out-patient evolution were obtained. The investigation of the events was performed by using information from medical records and telephone contacts. In those cases in which the same event reoccurred in one patient, the first event was considered for analysis purposes.
The study endpoint was the occurrence of major adverse cardiac and cerebral events (MACCE) during follow-up, defined as death from any cause, stroke, acute myocardial infarction (AMI), and target-vessel revascularization (TVR).
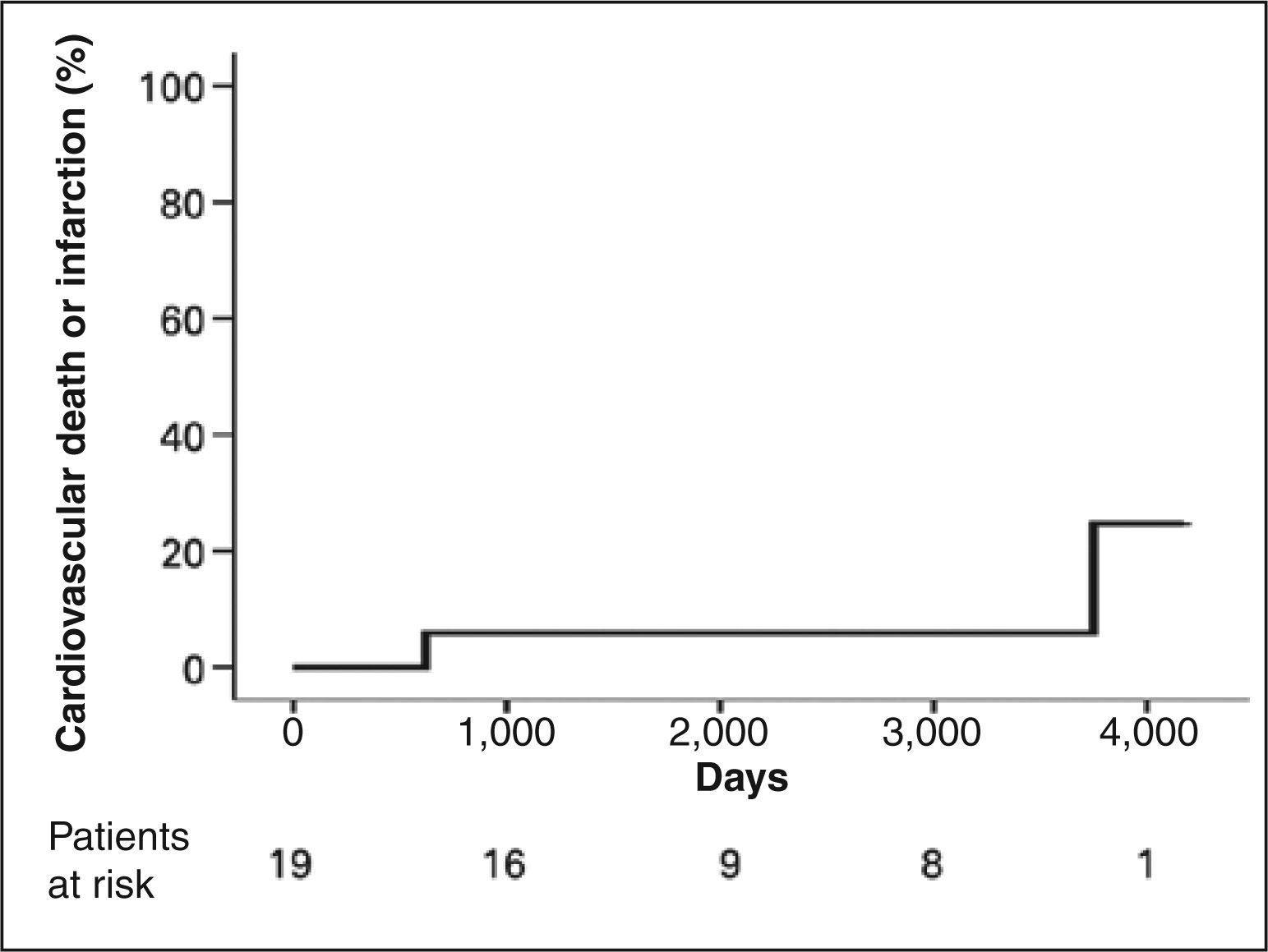
Continuous variables were described as means and standard deviations, whereas categorical variables were described as frequencies and percentages. The event rate was estimated by the Kaplan-Meier method.
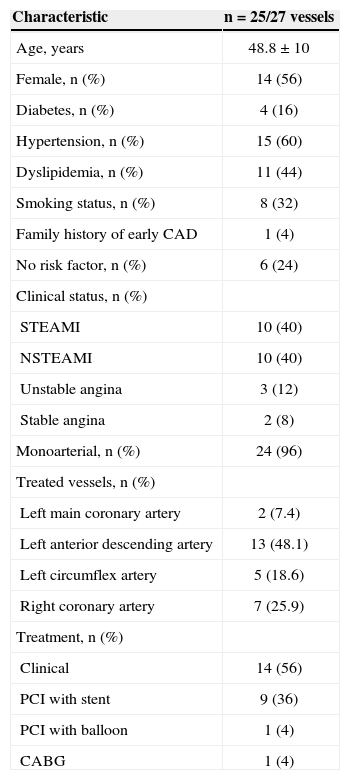
RESULTSTwenty-five patients were identified with a diagnosis of SCAD (Table 1); 56% were female subjects. The mean age was 48.8±10 years. The prevalence of hypertension was 60%; dyslipidemia, 44%; smoking, 32%; and diabetes, 16%. Only 24% of patients had no risk factors for atherosclerosis. Unstable coronary pictures predominated, with 80% of patients presenting with AMI (half of those with ST-segment elevation), and 12% with unstable angina. Two patients (8%) had stable angina.
Clinical, angiographic, and procedural characteristics
| Characteristic | n=25/27 vessels |
|---|---|
| Age, years | 48.8±10 |
| Female, n (%) | 14 (56) |
| Diabetes, n (%) | 4 (16) |
| Hypertension, n (%) | 15 (60) |
| Dyslipidemia, n (%) | 11 (44) |
| Smoking status, n (%) | 8 (32) |
| Family history of early CAD | 1 (4) |
| No risk factor, n (%) | 6 (24) |
| Clinical status, n (%) | |
| STEAMI | 10 (40) |
| NSTEAMI | 10 (40) |
| Unstable angina | 3 (12) |
| Stable angina | 2 (8) |
| Monoarterial, n (%) | 24 (96) |
| Treated vessels, n (%) | |
| Left main coronary artery | 2 (7.4) |
| Left anterior descending artery | 13 (48.1) |
| Left circumflex artery | 5 (18.6) |
| Right coronary artery | 7 (25.9) |
| Treatment, n (%) | |
| Clinical | 14 (56) |
| PCI with stent | 9 (36) |
| PCI with balloon | 1 (4) |
| CABG | 1 (4) |
CAD, coronary artery disease; STEAMI, ST-segment elevation acute myocardial infarction; NSTEAMI, non-ST-segment elevation acute myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft.
There was only one (4%) case of SCAD involving multiple vessels (left main coronary artery [LMCA], left anterior descending artery, and left circumflex artery). The left anterior descendent artery was the most affected vessel (48%). The strategy of medical therapy was predominant, utilized in 56% of cases, and the pharmacological therapy was based on the combination of anti-thrombotic and anti-ischemic drugs. Treatment with percutaneous coronary intervention was performed in 40% of patients by means of bare-metal stent implantation, or by balloon dilation in one case. Only the patient with multivessel dissection was treated with coronary artery bypass graft (CABG) surgery.
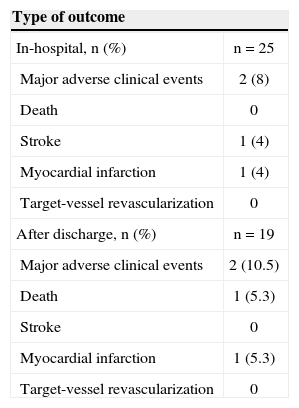
The in-hospital MACCE-free rate was 92%, with only one (4%) case of AMI and one other of stroke, both in patients with SCAD, treated by PCI and clinical therapy, respectively. The late follow-up was 75.6±43.1months. Six patients were lost to follow-up. In the long term; MACCE-free rate was 84.2%. There was no evidence of recurrence of spontaneous dissection in late follow-up. However, an episode of sudden death occurred approximately two years after SCAD in a medically treated patient. There was also a case of AMI without ST-segment elevation in a patient previously treated with PCI (Table 2). The Figure 1 depicts the estimated global incidence of cardiovascular death or myocardial infarction during follow-up.
Clinical outcomes
| Type of outcome | |
|---|---|
| In-hospital, n (%) | n=25 |
| Major adverse clinical events | 2 (8) |
| Death | 0 |
| Stroke | 1 (4) |
| Myocardial infarction | 1 (4) |
| Target-vessel revascularization | 0 |
| After discharge, n (%) | n=19 |
| Major adverse clinical events | 2 (10.5) |
| Death | 1 (5.3) |
| Stroke | 0 |
| Myocardial infarction | 1 (5.3) |
| Target-vessel revascularization | 0 |
The incidence of SCAD is substantially higher in young patients, and its incidence, etiology, and pathophysiology remain unclear.4,5 It is believed that hormonal factors, cardiocirculatory stress, and increased shear stress, associated with factors related to the weakening of the vessel wall, are conductive to the primary rupture of the vasa vasorum, leading to bleeding and, hence, the separation of arterial wall layers, creating a false lumen between the intima and media of the vascular wall.8
Intense physical exercise precedes the event in approximately 50% of cases occurring in males, and peripartum status is present in 20% of women.5 A number of comorbidities, such as Marfan syndrome, Ehlers-Danlos syndrome, antibody antiphospholipid disease, Osler-Weber-Rendu disease, polyarteritis nodosa, systemic lupus erythematosus, sarcoidosis, and severe hypertension have been described in association with SCAD. Other associated conditions include chest trauma, cardiac surgery, aortic dissection, cocaine use, smoking, and use of oral contraceptives or cyclosporine, among others.7,9
In this study, a higher incidence of SCAD was observed in a young population, predominantly in females. Regarding clinical characteristics, despite the predominance of younger patients, there was a high rate of systemic hypertension, as well as of dyslipidemia and smoking. Furthermore, only 24% of patients had no risk factors for atherosclerosis, suggesting that part of this population could present with an associated atherosclerotic disease.
Another interesting finding was the absence of women in the peripartum period in the study population, which may be explained by the older age group of the female population, compared to other studies.
Considering that SCAD is an important cause of sudden death in young adults, especially if there is involvement of multiple vessels, of the left main coronary artery (LMCA), or of the proximal left anterior descending artery,4,5 the present study showed a spectrum of clinical presentation with predominance of acute coronary pictures (92%). Although almost half of the patients presented dissection of the left anterior descending artery, the absence of in-hospital cardiac deaths may be explained by the low incidence of multivessel dissections or of LMCA dissections.
The most appropriate therapeutic strategy for the treatment of SCAD depends on the clinical severity and on coronary angiographic findings, such as the number of vessels involved, vessel size, location and extent of the dissection, and the myocardium area at risk.6 In the present study, the choice of therapeutic (clinical, surgical, or percutaneous) strategies confirmed the still uncertain nature of the ideal therapeutic approach to SCAD. The predominance of the conservative strategy (56%) was probably based on clinical stability, on the monoarterial feature, and on an imprecise location of the dissection flap. Most often, the initial site of the intimal tear is difficult to locate. With persistence of symptoms and the identification of the inlet port of the dissection, the percutaneous treatment may be indicated. In dissections with coronary occlusion involving multiple vessels or the LMCA and in presence of cardiogenic shock, an urgent surgical treatment appears to be the more appropriate choice.10,11
The absence of in-hospital deaths and the high event-free rate during late follow-up (84.2%) confirm the trend of a favorable prognosis in patients who survived the first event. Recent studies show a survival rate of approximately 80% at 25-30 months.7,10,12 In light of the current knowledge, the ideal approach to SCAD must be individualized, always taking into account the clinical presentation and the angiographic characteristics.
This study had some limitations, for instance, its retrospective design, based on information from the database and clinical records. Moreover, it was not possible to make telephonic contact in all cases during the late follow-up. Therefore, a non-trivial number of patients failed to be included in the final analysis. Furthermore, the inclusion of patients who had their procedures performed at very different times, above all in a specialty in which the advances of methods, devices, and drugs are so accelerated, caused some individuals to receive different treatments.
CONCLUSIONSIn this study, the incidence of SCAD was predominant in young women with acute coronary syndrome, most of them with the presence of at least one risk factor for coronary atherosclerotic disease. The left anterior descending artery was the most commonly affected vessel, and the therapeutic approach was individualized. The rate of MACCE was reduced in the late evolution, but further evaluation with prospective studies using larger numbers of patients is needed.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.
SOURCE OF FINANCINGNone.