Radial access is the object of increasing interest for interventional cardiologists, providing several advantages, including the reduced rates of major bleeding, which is related to increased risk of death and ischemic events. However, its role as an access technique in primary percutaneous coronary intervention (PCI) remains controversial due to the greater complexity of the procedure and possible delay in obtaining myocardial reperfusion, compared to femoral access.
MethodsRetrospective study including consecutive patients with a diagnosis of ST-elevation acute myocardial infarction (STEMI) undergoing primary PCI by radial access. Clinical, angiographic and procedure characteristics were analyzed, as well as early and late follow-up outcomes.
ResultsFrom October 2010 to February 2012, 61 patients underwent primary PCI by radial access. Mean age was 59±11.1years, 24.6% were female and 21.3% were diabetic. Door-to-balloon time was 126.1±44.7minutes, fluoroscopy time was 16.1±9.5minutes, angiographic success was achieved in 98.5%, with myocardial blush grades 2 and 3 in 77.4% and ST-segment elevation resolution > 50% at 90 minutes in 70.5% of the patients. Hospital mortality was 6.6% and the rate of major bleeding was 1.6%. In the late follow-up, clinical restenosis was observed in 7.2% and additional deaths in 3.5% of the patients.
ConclusionsThe use of radial access for primary PCI is safe and effective when performed at experienced centers and did not present delayed reperfusion when compared to historical data, showing low risk of major bleeding.
Intervenção Coronária Percutânea por AcessoTransradial em Pacientes com Infarto Agudo do Miocárdio com Supradesnivelamento do Segmento ST
IntroduçãoA via radial é objeto de interesse crescente de cardiologistas intervencionistas, por oferecer diversas vantagens, entre elas a redução da taxa de sangramento maior, associado a maior risco de morte e eventos isquêmicos. Entretanto, sua utilização como via de acesso na intervenção coronária percutânea (ICP) primária é motivo de controvérsias, pela maior complexidade do procedimento e pelo possível retardo para se obter a reperfusão miocárdica, quando comparada à via femoral.
MétodosEstudo retrospectivo, que incluiu pacientes consecutivos com diagnóstico de infarto agudo do miocárdio com supradesnivelamento do segmento ST (IAMCSST) submetidos a ICP primária por via radial. Foram analisados os perfis clínico, angiográfico e do procedimento, assim como a evolução tanto inicial como tardia.
ResultadosEntre outubro de 2010 e fevereiro de 2012, 61 pacientes foram submetidos a ICP primária por via radial. A média de idade foi de 59+11,1 anos, 24,6% eram do sexo feminino e 21,3% eram diabéticos. O tempo porta–balão foi de 126,1+44,7 minutos, o tempo de fluoroscopia foi de 16,1+9,5 minutos, o sucesso angiográfico foi alcançado em 98,5%, com obtenção de blush miocárdico graus 2 ou 3 em 77,4%, e resolução do segmento ST > 50% aos 90 minutos em 70,5% dos pacientes. A mortalidade hospitalar foi de 6,6% e a taxa de sangramento grave foi de 1,6%. Na evolução tardia, reestenose clínica ocorreu em 7,2% e óbitos adicionais, em 3,5% dos pacientes.
ConclusõesA utilização da via radial para ICP primária é segura e eficaz quando realizada em serviço familiarizados com a técnica, não apresentou retardo para a reperfusão, comparativamente a dados históricos, e demonstrou baixo risco de sangramento maior.
Radial access is the subject of increasing interest regarding diagnostic and therapeutic procedures worldwide and in Brazil. It has several advantages when compared to femoral access, such as convenience for the patient immediately after the procedure, earlier return to activities, decreased length of stay with consequent reduction of hospital costs, and a low complication rate at the puncture site. The low risk of puncture site complications leads to a reduced rate of major bleeding, which, in turn, is associated with a decreased risk of death and ischaemic events. 1−5
This access is particularly important in the setting of acute myocardial infarction with ST-segment elevation (STEMI), in which the use of antiplatelet and antithrombotic therapies is more aggressive, increasing the risk of bleeding. However, the role of percutaneous coronary intervention (PCI) through radial access in STEMI remains controversial, for reasons related to the complexity of the procedure and its possible delay in obtaining early reperfusion, the main goal of primary PCI.
This study aimed to evaluate the clinical, angiographic and procedural profiles, as well as the initial and late evolution in patients with STEMI undergoing primary PCI through radial access in a non-selected population representative of daily clinical practice.
METHODSThis was a retrospective study that included all consecutive patients with STEMI treated with primary PCI by radial access in the first 12 hours or up to 24 hours with persistent pain or hemodynamic instability. Patients with a previous CABG, patients with chronic renal failure, those on dialysis with a fistula in their upper right limb, and those in cardiogenic shock with no radial pulse were excluded. Patients in cardiogenic shock who responded to initial therapy with vasoactive amines and had a radial pulse on arrival to the catheterization laboratory were included.
The radial artery puncture was performed with the patient positioned with the right arm extended to the side, with his or her hand in the supine position. Local anaesthesia was used and was performed with 2 to 3mL of 2% lidocaine. A Jelco 20 was used to puncture the artery, and after puncture, arterial sheaths specific to the radial artery, which were 5-F to 7-F and 11cm in length, were inserted. After the procedure, the arterial sheath was removed in the room without heparin reversal, and a compression bandage applied, and then removed, usually two hours after the procedure.
All patients received a loading dose of 300mg of acetylsalicylic acid and 600mg of clopidogrel, followed by maintenance doses of 100mg and 75mg a day, respectively, and unfractionated heparin intravenously, at a dose of 70 to 100 U/kg.
The patients were followed after discharge, and follow-up occurred at one month, three months, six months, and one year through medical consultation or telephone contact.
Bleeding was defined according to the Thrombolysis in Myocardial Infarction 6 criteria (TIMI: minimal, any clinical sign of bleeding associated with a decrease in hemoglobin < 3g/dL; minor, any clinical sign of bleeding associated with a decrease in hemoglobin of 3g/dL to 5g/dL; and major, intracranial bleeding, signs of clinically significant bleeding associated with decrease in hemoglobin > 5g/dL, or fatal bleeding) and the Bleeding Academic Research Consortium (BARC: type 0, no bleeding; type 1, minor bleeding that does not require medical attention or hospitalization; type 2, any sign of bleeding that does not fit types 3, 4, or 5, but has at least one of non-surgical medical intervention, need for hospitalization, or increased level of care, or need for clinical evaluation; type 3A, bleeding associated with a decrease in hemoglobin of 3g/dL to 5g/dL or bleeding requiring blood transfusion; type 3B, bleeding associated with a decrease in hemoglobin > 5g/dL, cardiac tamponade, bleeding requiring surgical treatment for control, except dental, nasal, skin, hemorrhoids, or bleeding requiring the use of vasoactive drugs; type 3C, intracranial bleeding except micro-bleeding or hemorrhagic transformation, different subcategories of bleeding confirmed by autopsy, imaging tests or peritoneal or intraocular bleeding that compromises eyesight; type 4, bleeding related to coronary artery bypass graft (CABG) surgery; and type 5,fatal bleeding).
The TIMI criteria were used to define reinfarction after the procedure, 6 which states that for patients within 48 hours of the index procedure, three conditions must be present: documentation that creatine kinase MB fraction (CK-MB) was decreased (or total CK, when CK-MB is not available); the CK-MB obtained at least four hours after the procedure is > three times the upper limit of normal levels (or total CK, when CK-MB is not available); and an increase in CK-MB levels of at least 50% above the previous value.
Angiographic success was defined as a stenosis < 30% of the diameter with final TIMI 3 flow. The stent thrombosis was classified as acute, subacute, late, or very late; and as possible, probable, and definitive according to the criteria of the Academic Research Consortium (ARC). 8
Continuous variables were expressed as means and standard deviations and categorical variables as numbers and percentages.
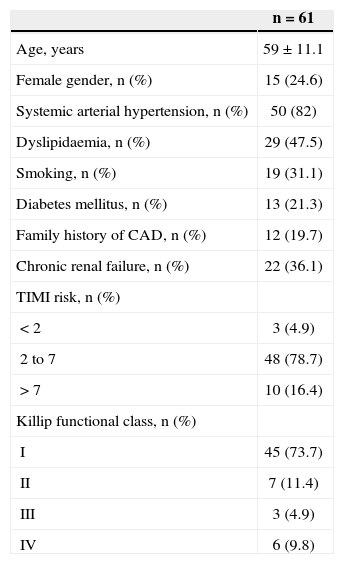
RESULTSBetween October 2010 and February 2012, 61 consecutive patients with STEMI underwent transradial PCI, with 71 lesions treated and 77 stents implanted. Of these patients, 26 (42.6%) were initially treated in basic health units in small neighbouring towns, with no alternative but to transfer them to the referral center, which was performed by the Mobile Emergency Service (Serviço de Atendimento Móvel de Urgência – SAMU). The mean age was 59±11.1years, 24.6% were females and 21.3% were diabetics. Most patients had a TIMI risk score of 2 to 7 and were Killip functional class I, and six (9.8%) were in cardiogenic shock (Table 1).
Baseline clinical characteristics of patients who underwent primary percutaneous coronary intervention through radial access
| n=61 | |
|---|---|
| Age, years | 59±11.1 |
| Female gender, n (%) | 15 (24.6) |
| Systemic arterial hypertension, n (%) | 50 (82) |
| Dyslipidaemia, n (%) | 29 (47.5) |
| Smoking, n (%) | 19 (31.1) |
| Diabetes mellitus, n (%) | 13 (21.3) |
| Family history of CAD, n (%) | 12 (19.7) |
| Chronic renal failure, n (%) | 22 (36.1) |
| TIMI risk, n (%) | |
| < 2 | 3 (4.9) |
| 2 to 7 | 48 (78.7) |
| > 7 | 10 (16.4) |
| Killip functional class, n (%) | |
| I | 45 (73.7) |
| II | 7 (11.4) |
| III | 3 (4.9) |
| IV | 6 (9.8) |
CAD=coronary artery disease; n=number of patientTIMI=Thrombolysis In Myocardial Infarction.
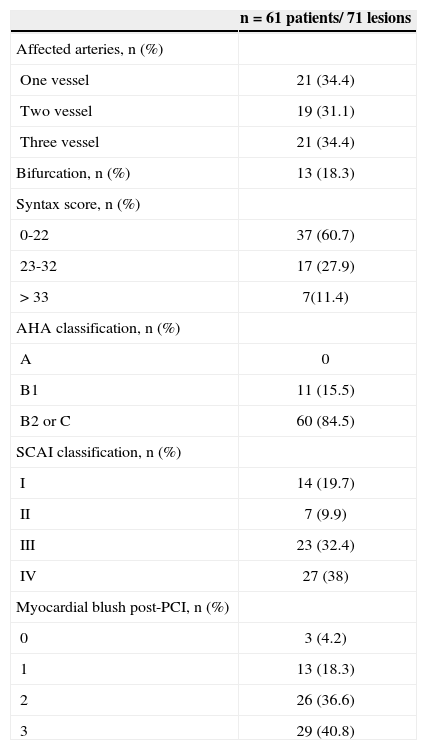
Regarding the angiographic characteristics, 34.4% cases were single vessel disease, 31.1% were two vessel, and 34.4% were three vessel. Most lesions were type B2 or C (84.5%) according to the classification of the American Heart Association (AHA) and type III or IV according to the Society for Cardiac Angiography and Interventions (Table 2).
Angiographic characteristics of patients who underwent primary percutaneous coronary intervention through radial access
| n=61 patients/ 71 lesions | |
|---|---|
| Affected arteries, n (%) | |
| One vessel | 21 (34.4) |
| Two vessel | 19 (31.1) |
| Three vessel | 21 (34.4) |
| Bifurcation, n (%) | 13 (18.3) |
| Syntax score, n (%) | |
| 0-22 | 37 (60.7) |
| 23-32 | 17 (27.9) |
| > 33 | 7(11.4) |
| AHA classification, n (%) | |
| A | 0 |
| B1 | 11 (15.5) |
| B2 or C | 60 (84.5) |
| SCAI classification, n (%) | |
| I | 14 (19.7) |
| II | 7 (9.9) |
| III | 23 (32.4) |
| IV | 27 (38) |
| Myocardial blush post-PCI, n (%) | |
| 0 | 3 (4.2) |
| 1 | 13 (18.3) |
| 2 | 26 (36.6) |
| 3 | 29 (40.8) |
AHA=American Heart Association; PCI=percutaneous coronary intervention; SCAI=Society for Cardiac Angiography and Interventions.
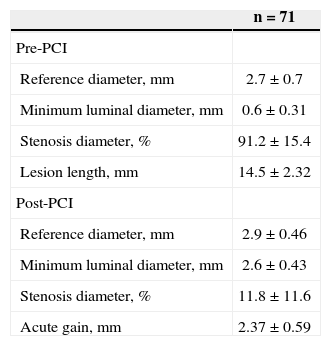
The time between symptom onset and hospital arrival (Dt) was 5.5±4.2hours and the door-to-balloon time was 126.1±44.7minutes. The 61 patients presented 71 lesions; 77 stents were implanted, thrombus aspiration catheters were used in 21.3%, and 81.7% were pre-dilated. The mean fluoroscopy time was 16.1±9.5minutes. It was necessary to change the route of access to the femoral artery in three patients (4.9%), one due to severe spasm that did not resolve with vasodilators and sedation, another due to arteria lusoria, and another due to significant radial artery tortuosity that prevented catheter progression. The glycoprotein IIb/IIIa inhibitor abciximab was used in 37.7% of cases, at the discretion of the operator. Angiographic success was achieved in 98.5%, with myocardial blush grade 2 or 3 in 77.4% and > 50% resolution of the ST-segment elevation at 90 minutes in 70.5% of patients (Tables 3 and 4).
Characteristics of the procedure in patients who underwent primary PCI through radial access
| n=61 | |
|---|---|
| Sheath, n (%) | |
| 5F | 2 (3.3) |
| 6F | 58 (95.1) |
| 7F | 1 (1.6) |
| Crossover of access route, n (%) | 3 (4.9) |
| Δt symptom onset-door, hours | 5.5±4.2 |
| Door-to-balloon time, minutes | 126.1±44.7 |
| Time of ischaemia, hours | 8±4.4 |
| Contrast volume, mL* | 121.2±43.2 |
| Fluoroscopy time, minutes* | 16.1±9.5 |
| Procedure time, minutes* | 48.3±23.2 |
| Abciximab, n (%) | 23 (37.7) |
| Thrombus aspiration catheter, n (%) | 13 (21.3) |
| Total lesions treated | 71 |
| Total stents implanted | 77 |
| Number of stents per patient | 1.26±0.23 |
| Resolution of ST-segment elevation at | |
| 90minutes, n(%) | |
| < 50% | 21 (29.6) |
| > 50% | 49 (70.5) |
| Angiographic success, % | 98.5 |
n=number of patients.
Quantitative coronary angiography
| n=71 | |
|---|---|
| Pre-PCI | |
| Reference diameter, mm | 2.7±0.7 |
| Minimum luminal diameter, mm | 0.6±0.31 |
| Stenosis diameter, % | 91.2±15.4 |
| Lesion length, mm | 14.5±2.32 |
| Post-PCI | |
| Reference diameter, mm | 2.9±0.46 |
| Minimum luminal diameter, mm | 2.6±0.43 |
| Stenosis diameter, % | 11.8±11.6 |
| Acute gain, mm | 2.37±0.59 |
PCI=percutaneous coronary intervention; n=number of lesions.
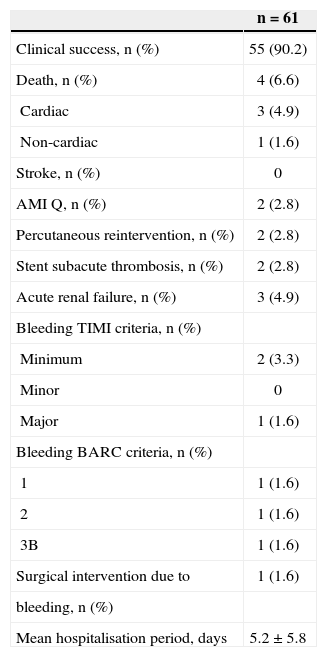
Regarding in-hospital evolution and outcomes up to 30 days (Table 5), clinical success was achieved in 90.2%, and there were two (2.8%) cases of AMI due to subacute stent thrombosis. In those two cases, there was an interruption in the clopidogrel regimen (one on the fifth day and the other on the eighth day post-PCI, after hospital discharge); these patients underwent re-operation through percutaneous reintervention. There were four deaths (6.6%), three from cardiac causes (patients with cardiogenic shock were included in the sample), and one from sepsis secondary to pneumonia associated with mechanical ventilation. Bleeding occurred in three patients, two of which were minor (classified as minimal by the TIMI criteria and 1 and 2 by BARC criteria) and one of which was major (major and type 3B by TIMI and BARC criteria, respectively). The major bleeding occurred in one of the patients whose access was changed to the femoral artery and required vascular surgery. The mean hospital stay was 5.2±5.8days. Table 6 presents the drugs prescribed at hospital discharge.
Clinical outcomes up to 30 days of patients who underwent primary percutaneous coronary intervention through radial access
| n=61 | |
|---|---|
| Clinical success, n (%) | 55 (90.2) |
| Death, n (%) | 4 (6.6) |
| Cardiac | 3 (4.9) |
| Non-cardiac | 1 (1.6) |
| Stroke, n (%) | 0 |
| AMI Q, n (%) | 2 (2.8) |
| Percutaneous reintervention, n (%) | 2 (2.8) |
| Stent subacute thrombosis, n (%) | 2 (2.8) |
| Acute renal failure, n (%) | 3 (4.9) |
| Bleeding TIMI criteria, n (%) | |
| Minimum | 2 (3.3) |
| Minor | 0 |
| Major | 1 (1.6) |
| Bleeding BARC criteria, n (%) | |
| 1 | 1 (1.6) |
| 2 | 1 (1.6) |
| 3B | 1 (1.6) |
| Surgical intervention due to | 1 (1.6) |
| bleeding, n (%) | |
| Mean hospitalisation period, days | 5.2±5.8 |
BARC=Bleeding Academic Research Consortium; AMI=acute myocardial infarction; n=number of patients; TIMI=Thrombolysis In Myocardial Infarction.
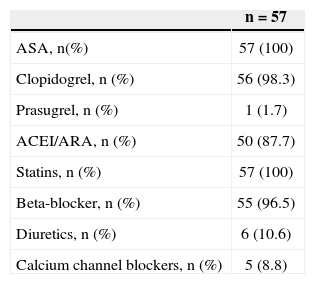
Drugs prescribed at hospital discharge
| n=57 | |
|---|---|
| ASA, n(%) | 57 (100) |
| Clopidogrel, n (%) | 56 (98.3) |
| Prasugrel, n (%) | 1 (1.7) |
| ACEI/ARA, n (%) | 50 (87.7) |
| Statins, n (%) | 57 (100) |
| Beta-blocker, n (%) | 55 (96.5) |
| Diuretics, n (%) | 6 (10.6) |
| Calcium channel blockers, n (%) | 5 (8.8) |
ASA=acetylsalicylic acid; ARA=angiotensin receptor antagonist; ACEI=angiotensin-converting enzyme inhibitor; n=number of patients discharged.
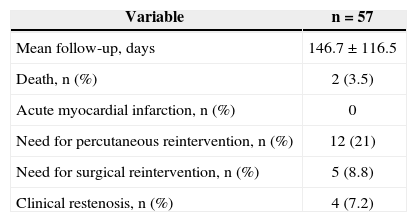
The mean follow-up time was 146.7±116.5days, with 94.7% of patients followed for three months, 91.2% for six months, and 61.4% for one year. During this period, 29.8% of the patients needed a new intervention, of which 21% were percutaneous and 8.8% were surgical. The majority (20.8%) underwent a second surgery to treat lesions that were not addressed in the acute phase, because only the culprit artery was treated in the acute phase, except in cases of cardiogenic shock. The clinical restenosis rate was 7.2%. There were two additional deaths (3.5%), both due to non-cardiac causes: one from complications of peripheral arterial disease and another from a massive pulmonary embolism. There were no cases of AMI in this period (Table 7).
Late evolution of patients who underwent primary PCI through radial access
| Variable | n=57 |
|---|---|
| Mean follow-up, days | 146.7±116.5 |
| Death, n (%) | 2 (3.5) |
| Acute myocardial infarction, n (%) | 0 |
| Need for percutaneous reintervention, n (%) | 12 (21) |
| Need for surgical reintervention, n (%) | 5 (8.8) |
| Clinical restenosis, n (%) | 4 (7.2) |
n=number of patients.
In the authors’ experience, primary PCI through radial access is as effective as through femoral access, with a high rate of technical success, low rate of crossover, and excellent safety, as the rates of bleeding and complications at the puncture site were practically absent in this sample. Many authors believe that the fluoroscopy time, an indirect measure of the difficulty of the procedure, is greater in PCI through radial access than through femoral access. The present results were consistent with those described by Farman et al. 9 for PCI through radial access, and shorter than that demonstrated by Alli et al. 10 for femoral access. It is important to mention that the surgeons must be familiar with the technique in order to achieve angiographic success and a low crossover rate of the access route in order to avoid delay of coronary reperfusion. In this center, the radial approach is the first choice for all procedures, whether therapeutic or diagnostic.
In patients with acute coronary syndrome, major bleeding is as common as recurrent infarction and occurs in approximately 5% of patients, depending on the definition used. A large proportion of the bleeding occurs at the vascular access site. 11 Findings from several studies suggest that major bleeding is associated with an increased risk of death and recurrent ischemic events. 12,13 Vascular access through the radial artery, which is a superficial artery and easily compressible, results in lower rates of access site bleeding than the femoral artery. Furthermore, findings from observational studies suggest a lower risk of death and myocardial infarction when the procedure is performed through radial access.14,15
A series of studies compared the radial and femoral routes in different scenarios. The RadIal Vs. femorAL access for coronary intervention trial (RIVAL) has demonstrated that, for surgeons with a high annual volume of PCI through radial access, patients with STEMI have benefited more from the radial than the femoral access with respect to both the composite endpoint of death, AMI, and stroke (P=0.011) and death (P=0.001). 11 The Prospective REgistry of Vascular Access in Interventions in Lazio region (PREVAIL) study showed best results with PCI through radial access in real world contemporary patients, demonstrating that the routine use of radial access was independently associated with a decreased risk of the primary endpoints, which were composed of major and minor bleeding, stroke and periprocedural complications of the vascular site (odds ratio [OR]: 0.37; 95% confidence interval [95% CI]: 0.16-0.84), as well as a decreased risk of the secondary endpoints, consisting of hospital death and reinfarction (OR: 0.14; 95% CI: 0.03-0.62). 16 The Acute Catheterisation and Urgent Intervention Triage strategY (ACUITY) study has demonstrated that the transradial approach reduces the rate of major bleeding compared to femoral access in patients with acute coronary syndromes (3% vs. 8.4%; P=0.03). 17
Finally, in Brazil, Andrade et al. 18 published a study with consecutive patients who underwent primary PCI through radial access and demonstrated that the performance of this procedure by experienced surgeons is safe, with a virtual absence of severe vascular complications related to the puncture site, findings that were reproduced in our study.
Study limitationsThis study has limitations inherent to its retrospective and observational design. The number of patients in the sample was small, it did not have a control group with PCI performed through the femoral artery, and it was performed at a single centre.
CONCLUSIONSThe use of the transradial approach in primary PCI is safe and effective and, if performed by surgeons who are familiar with the technique, has a high rate of technical success and a low risk of major bleeding, with no significant delay to reperfusion compared to historical data.
CONFLICT OF INTERESTThe authors declare no conflicts of interest.