There is scarce information on the time to return to work after general surgery. The aim of this study was to analyze time off work after elective cholecystectomy and to compare the results with those in patients undergoing other surgical interventions.
MethodsObservational and comparative study. Inclusion criteria were: being of working age and undergoing elective laparoscopic cholecystectomy (group 1) or unilateral inguinal hernia or haemorrhoidectomy (group 2).
Results36 patients were included: 18 patients in each group. Overall, return to work occurred at a mean of 35.7 days, with no significant differences (p=0.656) between groups (group 1: 36.6 days vs. group 2: 35.44 days). The reasons for not returning to work earlier were fear of complications (37.5%), pain control (37.5%), surgeon recommendation (12.5%), and general practitioner recommendation (12.5%).
ConclusionsTime to recovery after laparoscopic cholecystectomy is prolonged. No statistically significant differences with less complex surgical procedures were detected.
Existe escasa información acerca de la vuelta al trabajo tras una cirugía general. El objetivo de este estudio fue el de analizar el tiempo de ausencia del trabajo tras una colecistectomía electiva, comparando los resultados con los de aquellos pacientes sometidos a otras intervenciones quirúrgicas.
MétodosEstudio observacional y comparativo. Los criterios de inclusión fueron: estar en edad laboral y someterse a una colecistectomía electiva laparoscópica opcional (grupo 1), cirugía por hernia inguinal unilateral o una hemorroidectomía (grupo 2).
ResultadosSe incluyó a un total de 36 pacientes, 18 de ellos en cada grupo. La vuelta al trabajo se produjo a una media de 35,7 días, sin diferencias significativas (p=0,656) entre los grupos (grupo 1: 36,6 días frente al grupo 2: 35,44 días). Los motivos de no retornar al trabajo con anterioridad fueron el miedo a las complicaciones (37,5%), el control del dolor (37,5%), la recomendación del cirujano (12,5%), y la recomendación del médico de familia (12,5%).
ConclusionesEl tiempo de recuperación tras una colecistectomía laparoscópica es largo. No se detectaron diferencias estadísticamente significativas en comparación a las intervenciones quirúrgicas menos complejas.
Laparoscopic cholecystectomy has been a standard procedure since its introduction and is one of the most commonly performed procedures each year.1 For many years, reducing hospital admission has been a goal of healthcare. The safety, clinical results, complications, and long-term follow-up of laparoscopic cholecystectomy have been analyzed in depth, and several groups have evaluated the feasibility of performing this type of surgery as a day-case procedure.2,3 Such a switch would reduce the costs of the process.4
Despite the extensive literature on laparoscopic cholecystectomy, little attention has been paid to recovery time or return to work after surgery. Furthermore, there is scarce information on the wide variations among patients and countries found in this topic.5
A recent focus group discussion between physicians and patients analyzed some of the factors involved in reluctance to return to work after laparoscopic cholecystectomy.6 This information could be useful to minimize the time to return to work and to decrease the burden on the health system. However, no comparative study has analyzed back-to-work times in patients undergoing surgery for other reasons. Such a study could be useful to introduce measures for improvement.
The aim of this study was to analyze the time to return to work after laparoscopic cholecystectomy and to compare these times with those in patients who underwent surgery for haemorrhoids and unilateral inguinal hernia.
Material and methodsAn observational comparative study was performed among consecutive patients attending a single institution from January 2011 to May 2011 for cholelithiasis. The study was approved by the Research Ethics Committee at our institution and all participants gave their written informed consent for their data to be used in this study.
Inclusion and exclusion criteriaAdult patients of working age (less than 65 years old) who underwent elective surgery in the study period were considered eligible for inclusion. We selected two groups of procedures: Group 1 (study group) consisted of patients who underwent elective laparoscopic cholecystectomy, and group 2 (control group) comprised patients who underwent unilateral groin hernioplasty or haemorrhoidectomy in the same period and in the same hospital. Patients who refused to participate or who were not actively employed were excluded from the analysis.
A questionnaire was sent to all included patients after a telephone call. Non-responders were contacted after 1 month and those who failed to respond were contacted again 1 month later and sent a new questionnaire.
Study variablesThe main endpoint was the time of return to work after the surgical procedure. We collected data on the type of hospital admission, surgical risk using the Charlson comorbidity index,7 clinical results, comorbidities, type of work, and information on return to work after surgery. Variables related to the patients’ opinion of the length of convalescence were also included. All data were collected using self-administered questionnaires.
Sample size calculationThe sample size was calculated prior to the performance of the study by considering previously published data indicating a possible difference of 50% in return to work 14 days after two groups of surgical procedures.5,8 We would need to study a minimum sample size of 18 patients per group to have a power of 80% and an alpha risk of 5%.
Statistical analysisQuantitative data are expressed as absolute numbers, mean, standard deviation (SD) and range between parentheses. Categorical variables are presented as absolute numbers or percentages. Comparisons of qualitative data were performed by means of a two-tailed Chi-square test (or Fisher's exact test when needed). Continuous variables were compared by using a non-parametric test (Mann–Whitney U test) according to a previous analysis of the normal distribution of the data. Survival curves were plotted using the Kaplan–Meier test and were compared with the log-rank test to analyze the time taken to return to work after surgery. A bilateral p-value of less than 0.05 was considered statistically significant. The statistical analysis was performed using the SPSS™ statistical package, version 17.0 (SPSS™ Chicago, IL, USA).
ResultsBetween January 2011 and May 2011, 717 patients were attended in our department. Of these, 141 were eligible for inclusion in the study: 59 in group 1 and 82 in group 2. Sixty-three patients (44.7%) returned the questionnaire. Finally, 27 patients were excluded: 22 for providing inconsistent data and the remaining five because they were not actively working at the time of the study (four were unemployed and one had taken early retirement). Therefore, 36 patients were included in the final analysis (18 patients in group 1 and 18 patients in group 2: 10 patients who received an unilateral groin hernia repair and the remaining, an hemorroidectomy).
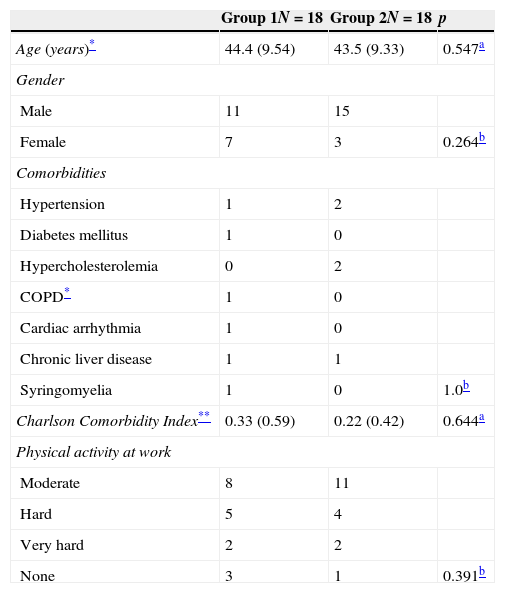
Patient characteristics and clinical dataThe general characteristics of the two groups are shown in Table 1. There were no statistically significant differences in age, gender, comorbidities or the Charlson comorbidity index between the two groups.
Characteristics of patients and work in both groups.
| Group 1N=18 | Group 2N=18 | p | |
|---|---|---|---|
| Age (years)* | 44.4 (9.54) | 43.5 (9.33) | 0.547a |
| Gender | |||
| Male | 11 | 15 | |
| Female | 7 | 3 | 0.264b |
| Comorbidities | |||
| Hypertension | 1 | 2 | |
| Diabetes mellitus | 1 | 0 | |
| Hypercholesterolemia | 0 | 2 | |
| COPD* | 1 | 0 | |
| Cardiac arrhythmia | 1 | 0 | |
| Chronic liver disease | 1 | 1 | |
| Syringomyelia | 1 | 0 | 1.0b |
| Charlson Comorbidity Index** | 0.33 (0.59) | 0.22 (0.42) | 0.644a |
| Physical activity at work | |||
| Moderate | 8 | 11 | |
| Hard | 5 | 4 | |
| Very hard | 2 | 2 | |
| None | 3 | 1 | 0.391b |
Only three patients were self-employed (one in group 1 vs. two in group 2; p=1.0). Table 1 shows the type of physical activity performed at work by the patients in the two groups.
Day-case surgery was performed in 88.8% of the patients in group 2 vs. 0% in group 1 (p<0.001). In hospitalized patients, the length of hospital stay was similar in the two groups (group 1: 1.17 days vs. group 2: 0.28 days, p=0.105). Postoperative complications were also similar in both groups: group 1: 0% vs. group 2: 1 patient (5.5%) (p=1.0).
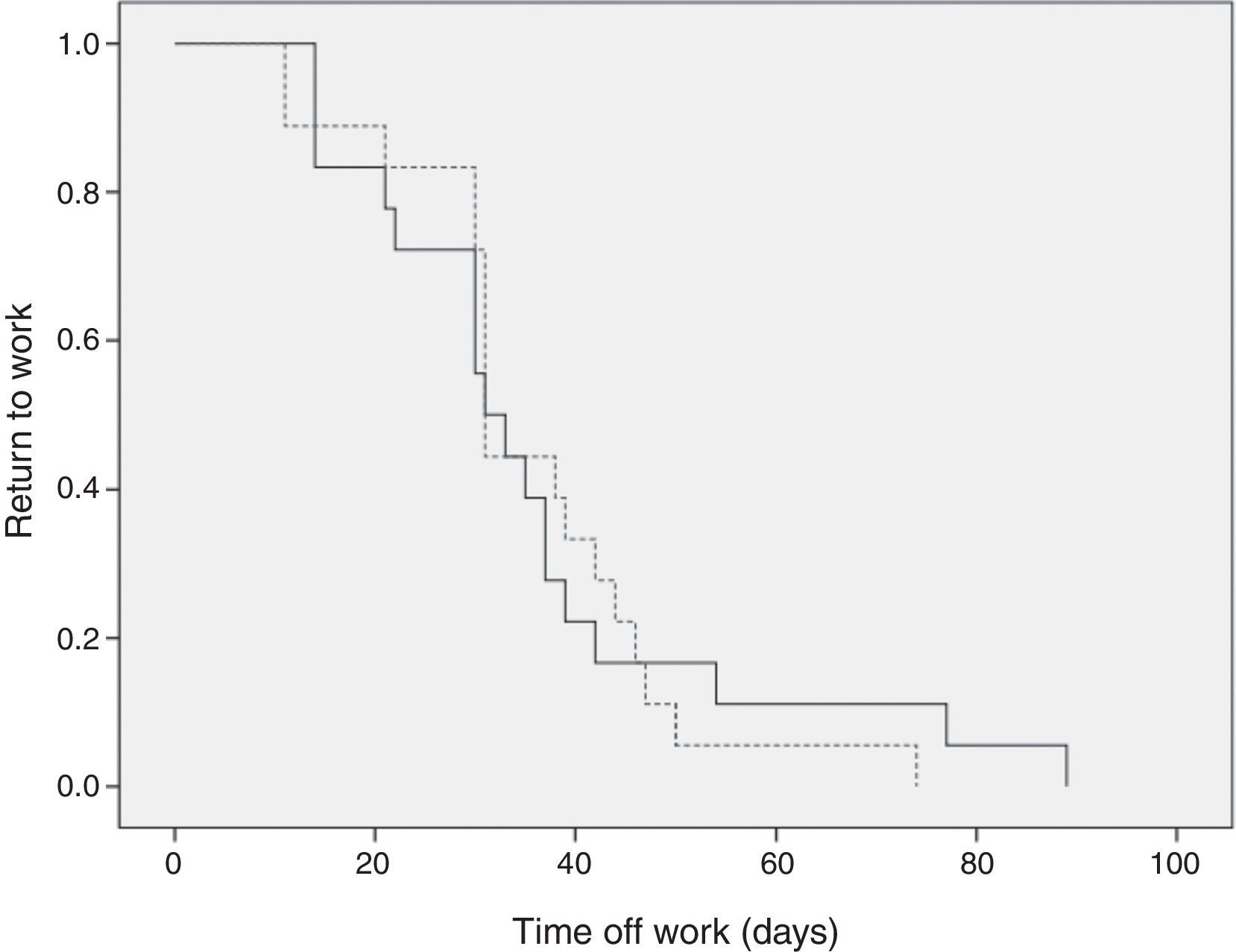
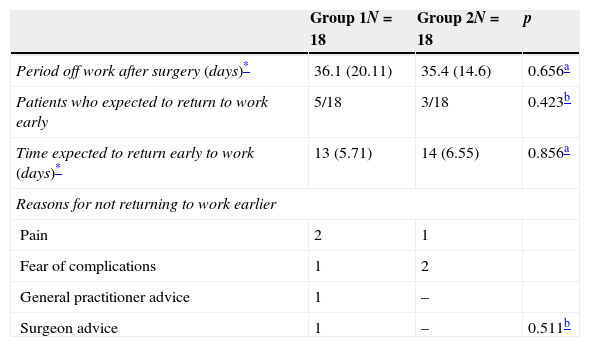
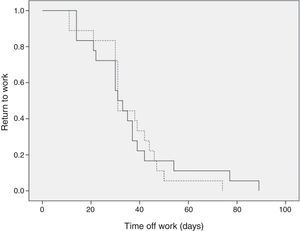
Time to return to workOverall, return to work occurred at a mean of 35.7 days (range 11–89). There were no statistically significant differences (p=0.656) in the time to return to work between the two groups: group 1, mean: 36.6 days (range 14–89) vs. group 2, mean: 35.4 days (range 11–74) (Table 2). Fig. 1 shows the survival curves for return to work after surgery in each group. There were no statistically significant differences among the groups (p=0.922).
Time to return to work after surgery and patient's opinion in both groups.
| Group 1N=18 | Group 2N=18 | p | |
|---|---|---|---|
| Period off work after surgery (days)* | 36.1 (20.11) | 35.4 (14.6) | 0.656a |
| Patients who expected to return to work early | 5/18 | 3/18 | 0.423b |
| Time expected to return early to work (days)* | 13 (5.71) | 14 (6.55) | 0.856a |
| Reasons for not returning to work earlier | |||
| Pain | 2 | 1 | |
| Fear of complications | 1 | 2 | |
| General practitioner advice | 1 | – | |
| Surgeon advice | 1 | – | 0.511b |
Of all the patients evaluated, eight (22.2%) returned to work early (group 1: 5 patients vs. group 2: 2 patients, p=0.691) at a mean of 13.4 days (Table 2). Table 2 shows the reasons for not returning to work earlier in groups 1 and 2.
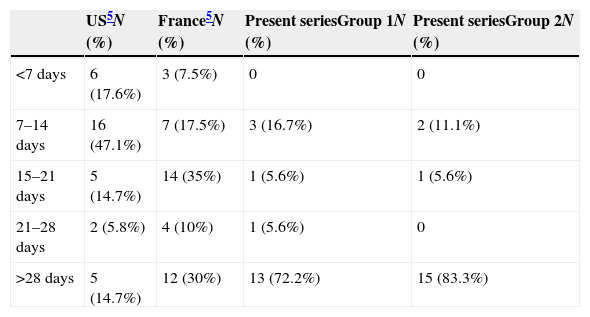
Table 3 compares the time to return to work in groups 1 and 2 with that in previous studies performed in distinct countries.5 A total of 65% of American and 25% of French patients returned to work within 14 days of surgery, while only 13.8% of our series did so after the same procedure or after a procedure of low complexity.
DiscussionCurrently, reducing health costs is imperative but there is little information on return to work after surgery. In the present study, we found a long recovery period before return to work after surgical procedures.
Cholecystectomy is one of the commonest procedure performed worldwide.9 Some investigations have focused on reducing hospitalization for this procedure, but there is scarce information on how to shorten recovery times after surgery. Vitale et al.5 compared return to work in patients undergoing surgery in the USA and in France. Interestingly, 65% of the Americans and 25% of the French patients returned to work within 14 days. In our series, only 13.8% of the patients did so after the same procedure or after a complex intervention (Table 3).
A prolonged period of convalescence is a burden to the health system. The cost of worker absenteeism in Spain has been calculated as 120 € per day (about 100 US$) by the Spanish Labour Ministry.10 A possible explanation for the delay in return to work could be the percentage of self-employed patients but, in this study, only 8.3% of the patients were self-employed.
The results of the present study demonstrate a long recovery period in patients after cholecystectomy and other surgical procedures. These results are similar to previously published results in our country and to those reported in French patients but are very different from those reported in the USA.5,10,11 In a novel study, Bisgaard et al.11 evaluated the influence of surgeon recommendations on the time to return to work after cholecystectomy. Surprisingly, the recommendation in patients with a moderate workload was 2 days of convalescence. In a sample of 85 patients, the mean number of days of sick leave was 6, with some patients returning to work on the day of surgery.11
The reasons for not returning to work earlier should also be evaluated. The return to work involves patients, surgeons and general practitioners. Patients themselves are undoubtedly the key element in early return to work. Experiences evaluating a very early return to work after surgery revealed that pain control and preoperative expectations were significantly associated with convalescence.11 This finding has been supported by other studies.5,6,12 Moreover, in this study, of eight patients who returned to work early, three (37.5%) had physical symptoms and a further three were afraid of complications.
Surprisingly, among specialists, opinions vary on an appropriate convalescence time. In hernia repair, for example, despite a lack of evidence, some patients are advised by surgeons to limit their physical activity for 6–8 weeks to prevent recurrence.13,14
In addition, the range of variation in recommendations on return to work after surgery is surprising, not only in cholecystectomy but also the other procedures included in this study (haemorrhoidectomy and unilateral inguinal hernia).15 The most surprising finding in our survey was the wide variation in the recommended convalescence time for haemorrhoidectomy, which ranged from 1 to 16 weeks.15
A recent study using focus group methodology in patients and physicians found evidence of some discrepancies among participants. While physicians believed that their advice was the key factor, patients seldom mentioned their physician's advice and reported that the major factor influencing their return to work after cholecystectomy was physical complaints (postoperative pain).6 Finally, there were also some cultural norms that influenced the patient, specialists and general practitioners’ perspectives and point of view as it was also stated.5
To minimize the time taken to return to work, several steps should be considered. Firstly, information should be given preoperatively on the expected recovery time when there are no complications. Secondly, information should again be provided on standard recovery times at hospital discharge, as well as after the first postoperative follow-up schedule in outpatient department. Thirdly, since general practitioners in Spain have the final say in return to work, fluid communication between these physicians and their patients must be maintained. Indeed, general practitioners have been found to require more information on and training in occupational health.12 Finally, as indicated by our results, the use of adequate analgesia protocols in these patients is essential.6,11
The role of general practitioners in managing information on convalescence after surgery and the influence of this information are controversial.12 However, in Spain, the role of general practitioners should be considered in attempts to reduce recovery times. We are currently designing a future prospective study aiming to reduce the interval until return to work in our institution, involving all surgical staff and general practitioners and including patients’ expectations.
The major strength of the present study is the homogenous sample size and the comparison of distinct surgical procedures. However, this study also has some limitations. First, the response rate to the questionnaire was low, which could be due to a selection bias. The control group was designed to include patients undergoing less complex procedures in the same period and therefore we included those undergoing surgery for groin hernia and haemorrhoids. These low-complexity procedures, however, can result in postoperative pain, which may account for the long recovery period, similar to that in the study group.
In conclusion, the time to return to work after surgery was long both in the laparoscopic cholecystectomy group and in patients undergoing surgery for groin hernia or haemorrhoids. The causes of this late return to work were inadequate pain control and lack of adequate information on possible complications. Stronger efforts are warranted in initiatives to improve this parameter.
DisclaimerNone.
FundingNone.
Conflict of interestDavid Parés MD, PhD and other co-authors have no conflict of interest.
The authors thank Gail Craigie for editorial support.
This study was presented at the 29th Congreso Nacional de Cirujanos in Madrid (Spain), 13th–15th November 2012.