Defensive medicine affects healthcare systems worldwide. The concerns and perception about medical liability could lead practitioners to practise defensive medicine. Second victim is a healthcare worker involved in an unanticipated adverse patient event. The role of being second victim and the other possible determinants for defensive medicine is mostly unclear.
ObjectiveTo study the condition of being second victim as a possible determinants of defensive medicine among Italian hospital physicians.
Design, setting and participantsA secondary analysis of the database of the national survey study on the prevalence and the costs of defensive medicine in Italy that was carried out between April 2014 and June 2014 in 55 Italian hospitals was performed for this study. The demographic section of the questionnaire was selected including the physician's age, gender, specialty, activity volume, grade and the variable being a second victim after an adverse event.
ResultsA total sample of 1313 physicians (87.5% response rate) was used in the data analyses. Characteristics of the participants included a mean age 49.2 of years and 19.4 average years of experience. The most prominent predictor for practising defensive medicine was the physicians’ experience of being a second victim after an adverse event (OR=1.88; 95%CI, 1.38–2.57). Other determinants included age, years of experience, activity volume and risk of specialty.
ConclusionsMalpractice reform, effective support to second victims in hospitals together with a systematic use of evidence-based clinical guidelines, emerged as possible recommendations for reducing defensive medicine.
La medicina defensiva afecta a los sistemas de salud de todo el mundo. Las preocupaciones y la percepción acerca de la responsabilidad médica podrían llevar a los médicos a ejercer la medicina defensiva. La segunda víctima es un trabajador sanitario que participa en un episodio adverso imprevisto del paciente. Sin embargo, el papel de segunda víctima y otros posibles determinantes de la medicina defensiva son poco claros.
ObjetivoEstudiar la situación de segunda víctima como posible determinante de la medicina defensiva entre los médicos hospitalarios italianos.
Diseño, entorno y participantesEn este estudio se realizó un análisis secundario de la base de datos de la encuesta nacional sobre prevalencia y costes de la medicina defensiva en Italia, que se había llevado a cabo entre abril y junio de 2014 en 55 hospitales italianos. Se seleccionaron los datos personales del cuestionario, como edad del médico, sexo, especialidad, volumen de la actividad, grado y la variable de ser segunda víctima después de un episodio adverso.
ResultadosSe utilizó una muestra total de 1.313 médicos (87,5% de tasa de respuesta) en el análisis de datos. Las características de los participantes incluyeron una media de edad de 49,2 años y 19,4 años de experiencia por término medio. El factor predisponente más importante para la práctica de la medicina defensiva fue la experiencia de los médicos de haber sido segunda víctima después de un episodio adverso (OR=1,88; IC 95%: 1,38-2,57). Otros factores determinantes fueron: edad, años de experiencia, volumen de la actividad y riesgo de la especialidad.
ConclusionesLa reforma de la responsabilidad médica, un apoyo efectivo a segundas víctimas en hospitales y un uso sistemático de las guías clínicas basadas en la evidencia se presentaron como posibles recomendaciones para la reducción de la medicina defensiva.
Defensive medicine (DM) is a deviation from sound medical practice that is induced primarily, but not solely, by the threat of liability claims.1–4 Therefore, a doctor's attitude towards DM determines the extent to which he deviates from his usual behaviour or that which is considered evidence-based medicine. This deviation can include ordering unnecessary tests, procedures, visits, and hospital admissions or the avoidance of high-risk patients, procedures, or medical services.5,6 Therefore, DM is expensive and may expose patients to risk of injury from unnecessary tests and procedures, whereas it can deny patients productive care.4,7
In the United States, 93% of physicians reported practising DM in a hospital, and 78% of hospital doctors in the United Kingdom and 60% in Israel and in Italy practised DM in a hospital.2,4,7,8 The percentage of doctors practising DM is higher for some specialties, for example, obstetrics and gynaecology (97%), gastroenterology (94–98%), neurosurgery (75–83%), and orthopaedics and traumatology (96%).5,9–14The practice of DM is a significant financial burden in healthcare systems. In the United States, DM is estimated to cost approximately US $50–100 billion annually.15,16 Two national surveys in the United States estimated the costs of DM in the orthopaedic community to range from US $256.3 million to nearly $2 billion annually.15,16 In Italy has been recently estimated that DM could absorb 10.71% of the total national health expenditure, with an estimated total cost of about €11.60 billion per year.8 Another study in Italy estimated the yearly cost of defensive procedures performed by gastroenterologists to be €8637 million in a region with a population of around 10 million inhabitants.11 At the patient level, the practice of DM was also estimated to cost hospitals US $226, which is the 13% of the mean patient cost (US $1695).17
Even though several studies showed how concerns and perception about medical liability – including being sued – could cause practitioners to practise DM, the role of other determinants of DM remain mostly unclear, including the doctor's age and experience.2,4,9,12,16,18–21 A second victim is ‘a healthcare provider involved in an unanticipated adverse patient event, medical error, and/or a patient-related injury, who becomes victimised in the sense that the provider is traumatised by the event’.22,23 The possible role of being second victim has never been assessed as possible determinants of DM. The objective of this study, therefore, was to identify the determinants of DM among Italian hospital doctors including being a second victim.
MethodsA cross-sectional study design was adopted to perform a secondary analysis of the database of the national survey study on the prevalence and the costs of DM in Italy. The survey was carried out between April 2014 and June 2014 in 55 Italian hospitals.8 1500 physicians were randomly invited to complete the survey. The invitation email contained a link to an anonymous web-based questionnaire. Reminder invitations were sent every month during the data collection period. No incentive was provided for participation to the survey. The demographic section of the 44 items questionnaire adopted in the survey, including the physician's age, gender, specialty, activity volume, and grade was adopted to perform the analysis. To better understand the impact of this psychosocial burden, a variable we termed ‘being a second victim’ was also included in the demographic section.
For the scope of this study, doctors who declared to perform any of the following were considered to be practising DM. Ordering unnecessary laboratory exams and/or diagnostic tests or procedures, prescribing more medications than medically indicated, referring patients to specialists and/or to emergency room, admitting or transferring patients to hospital in unnecessary circumstances, avoiding treating high-risk patients, or avoiding performing high-risk procedures. In brief the doctors were asked to answer “yes” or “not” to any of the above reported conditions.
Each quantitative variable was summarised as a mean value and standard deviation. To summarise qualitative variables, frequencies and percentages were used. First, we performed univariate analyses to evaluate differences in doctors who practise DM and those who do not. Student's t tests (for continuous variables) or chi-squared tests (for categorical variables) were used. Second, significant factors identified in this first step of analysis were entered into a multivariate binary logistic regression model and evaluated as possible predictors of DM practice (outcome variable). A p value of <0.05 was considered significant.
Five factors were evaluated in relation to the practice of DM: age, gender, specialty, experience, activity volume, and perception of being a ‘second victim’. Since only three physicians in the sample were 29 or 30 years old or younger, participants were divided into three age groups: younger than 40 years, 41–50 years, and older than 50 years. Specialties were categorised into either a higher-risk specialty or lower-risk specialty.7,24 The doctors’ years of physician-level experience were divided into three grades: junior, middle, or senior. According to the Italian national contract for medical doctors, junior grade includes doctors in foundation year one to five. Senior grade includes consultants and doctors practising more than 15 years. By exclusion, middle grade includes those physicians who are not junior or senior grade. The activity volume was categorised into three levels based on weekly activity: low (up to 30 procedures/visits per week); medium (from 31 to 70 procedures/visits per week), or high (more than 70 procedures/visits per week). The status of second victim perception was assigned to the doctors based on a dichotomous scale (yes/no). The data were analysed using SPSS 22.0 for Windows (IBM Corp. Released 2013. Armonk, NY, USA).
ResultsA total sample of 1313 physicians (87.5% response rate), 794 males and 519 females, was used in the data analyses. The sample included 310 general surgeons (23.6%), 119 anaesthesiologists (9.0%), 110 internists (8.3%), 109 paediatricians (8.3%), 91 psychiatrics (6.9%), 85 emergency doctors (6.4%), 90 radiologists (6.8%), 67 cardiologists (5.1%), 64 urologists (4.8%), 80 pathologists (6.0%), 54 neurologists (4.1%), 49 rehabilitation doctors (3.7%), and the remaining 85 respondents practised in other specialties (6.4%). The main practice locations were hospital wards in combination with ambulatory clinics, 857 (65.2%); ambulatory clinics alone, 282 (21.4%); emergency rooms, 156 (11.8%); and other places/combinations, 18 (1.3%). The majority of the physicians (58.8%) visited/treated more than 40 patients per week. Seven hundred and eighty-five physicians (59.7%) stated that they practise one kind of or a combination of kinds of DM surveyed in the questionnaire and 244 were second victims (18.5%). Other characteristics of the participants included a mean age 49.2 of years, 19.4 average years of experience.
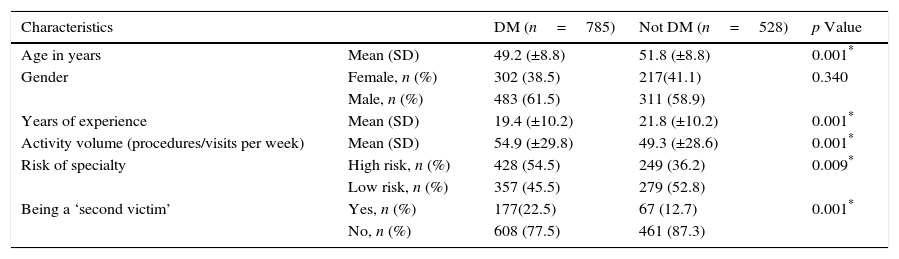
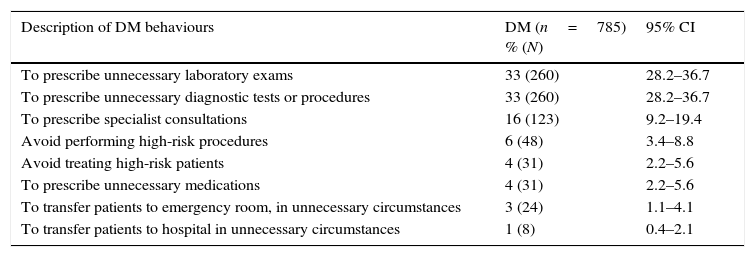
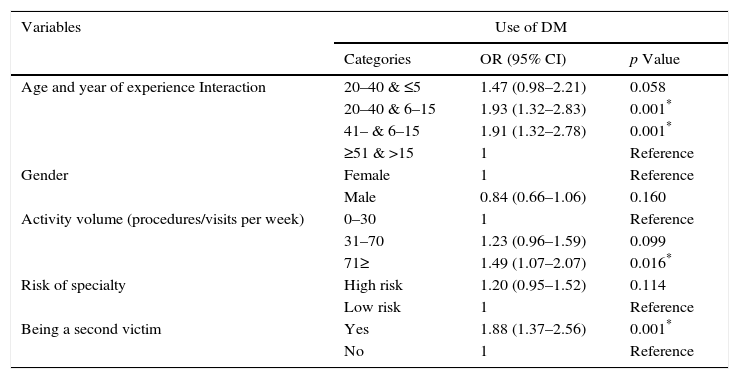
In univariate analysis, age, years of experience, activity volume, risk of specialty, being a ‘second victim’, emerged as to be differently distributed in doctors who practise DM and those who do no (Table 1). Active/positive DM, that occurred when extra tests and procedures are performed primarily to reduce malpractice,4 was the most frequent in the sample. Negative defensive medicine was less used (the description of specific behaviour is be shown in Table 2). Multivariate logistic regression analyses revealed that being a second victim was the most prominent significant predictor for practising DM. Others determinants included the age of physicians, associated with the level of experience and volume patients treated (Table 3).
Results of univariate analyses to evaluate differences in doctors who practise defensive medicine and those who do not.
| Characteristics | DM (n=785) | Not DM (n=528) | p Value | |
|---|---|---|---|---|
| Age in years | Mean (SD) | 49.2 (±8.8) | 51.8 (±8.8) | 0.001* |
| Gender | Female, n (%) | 302 (38.5) | 217(41.1) | 0.340 |
| Male, n (%) | 483 (61.5) | 311 (58.9) | ||
| Years of experience | Mean (SD) | 19.4 (±10.2) | 21.8 (±10.2) | 0.001* |
| Activity volume (procedures/visits per week) | Mean (SD) | 54.9 (±29.8) | 49.3 (±28.6) | 0.001* |
| Risk of specialty | High risk, n (%) | 428 (54.5) | 249 (36.2) | 0.009* |
| Low risk, n (%) | 357 (45.5) | 279 (52.8) | ||
| Being a ‘second victim’ | Yes, n (%) | 177(22.5) | 67 (12.7) | 0.001* |
| No, n (%) | 608 (77.5) | 461 (87.3) | ||
Doctor's response rates to items concerning the practice of DM.
| Description of DM behaviours | DM (n=785) % (N) | 95% CI |
|---|---|---|
| To prescribe unnecessary laboratory exams | 33 (260) | 28.2–36.7 |
| To prescribe unnecessary diagnostic tests or procedures | 33 (260) | 28.2–36.7 |
| To prescribe specialist consultations | 16 (123) | 9.2–19.4 |
| Avoid performing high-risk procedures | 6 (48) | 3.4–8.8 |
| Avoid treating high-risk patients | 4 (31) | 2.2–5.6 |
| To prescribe unnecessary medications | 4 (31) | 2.2–5.6 |
| To transfer patients to emergency room, in unnecessary circumstances | 3 (24) | 1.1–4.1 |
| To transfer patients to hospital in unnecessary circumstances | 1 (8) | 0.4–2.1 |
DM, defensive medicine; CI, confidence intervals.
Results of multiple binary logistic regression model predicting the use of defensive medicine.
| Variables | Use of DM | ||
|---|---|---|---|
| Categories | OR (95% CI) | p Value | |
| Age and year of experience Interaction | 20–40 & ≤5 | 1.47 (0.98–2.21) | 0.058 |
| 20–40 & 6–15 | 1.93 (1.32–2.83) | 0.001* | |
| 41– & 6–15 | 1.91 (1.32–2.78) | 0.001* | |
| ≥51 & >15 | 1 | Reference | |
| Gender | Female | 1 | Reference |
| Male | 0.84 (0.66–1.06) | 0.160 | |
| Activity volume (procedures/visits per week) | 0–30 | 1 | Reference |
| 31–70 | 1.23 (0.96–1.59) | 0.099 | |
| 71≥ | 1.49 (1.07–2.07) | 0.016* | |
| Risk of specialty | High risk | 1.20 (0.95–1.52) | 0.114 |
| Low risk | 1 | Reference | |
| Being a second victim | Yes | 1.88 (1.37–2.56) | 0.001* |
| No | 1 | Reference | |
Our study has several limitations that need to be addressed before discussing our results. First, a rigorous measurement of DM and of its determinants is elusive, mainly because distinctions between inappropriate and appropriate care are unclear in many clinical situations.2,25 We believe this measurement issue is the major limitation of our study and indeed all studies investigating DM. We also recognise that other factors may determine DM, such as the enormous variation in the medical malpractice environment, and in the healthcare and welfare systems and legal institutions across countries.20 Although this does not affect the validity of our results, it could limit their generalisability. Our study also has limitations related to the nature of study design. In fact, self-reports of DM may be biased by the recall aspect of trying to remember behaviours not immediately being engaged. Self-reports can also be biased by concerns about reporting DM practices, including a ‘socially desirable response bias’.13,25,26 Together with unconsciously practised DM, this could lead to an underestimation of the prevalence of DM and, consequently, a possible contamination bias of the sample.5 According to the data available another important limitation is that the link between medical liability and practicing DM was not thoroughly explored.
The most prominent predictor for practising DM was the physicians’ experience of being a second victim after an adverse event. We believe that this is an important finding for several reasons. In fact, clarification of this issue can be helpful in understanding the real effect of medical liability on DM. In previous studies, objective measures of physicians’ liability experience and exposure were not associated with the propensity to practise DM.2,10 However, the more recent literature shows how physicians’ liability experience is a significant predictor of practising DM.7,12,13,19,27,28 This is probably due to the stress and emotional toll of being involved in litigation; in fact, the majority of doctors that experienced or feared litigation lose confidence, feel shame, and feel guilty.15
A second victim is likely to be a physician that experiences liability. On the other hand, a physician can be a second victim with or without having been sued. We believe that being a second victim is a better predictor of practising DM than the mere liability experience and exposure, because it better measures the personal anxiety and emotional toll of physicians that harmed their patients and suffered for their own actions.16 Moreover, even if a significant portion of physicians become second victims every year, effective management of this problem is poor in the Italian healthcare system, as well as in those of most other developed countries.23,29 In our sample only 3 on 33 hospitals declared to have official procedures to support the second victim. Therefore, we conclude that our study supports the need for implementing effective procedures to help second victims and suggests that the initial costs might easily be reversed later. We believe that any independent ethical consideration about the need for healthcare systems to care for their second victims could be an effective (and simple) way to reduce initiating DM.
According to other studies, age and experience are associated with less frequently practised DM.4,10,12,20 In our regression model, we used a single variable to represent the interaction between age and level of experience, since they were strongly associated in the univariate analysis. We think our findings show that this is the most effective way to describe the physicians’ competency level or experience level in these kinds of studies.
The weekly activity volume was another significant predictor of DM, with higher volumes increasing the odds that a physician will practise DM. This is not surprising, and it suggests a possible way to reduce the practice of DM by simply redistributing the activity level among the clinical teams.
Our study did not show significant differences in the practice of DM among different specialties. The literature suggests that the practice of DM is linked to surgical specialties.7 We believe our survey results failed to corroborate this finding, because our sample included very few physicians in high-risk specialties such as neurosurgery (i.e., 4.11% of entire sample).12 Similar to other studies, we found no correlation between gender and the practice of DM.4,7
Despite some limitations, we believe that our study enriches the current literature on DM. Our findings helped to clarify the determinants of DM. In particular, a new determinant was identified and others that have been previously described were corroborated. We measured a greater tendency of practising DM in physicians who became second victims after an adverse event. We believe this information is relevant both for guiding further research aimed to better understand the mechanism of DM and for implementing possible actions to prevent it.
In conclusion, based also on the results of the present study on DM, the tort reform, currently being discussed in parliament, is finally going to become a law in Italy. It will be applied as a possible normative intervention to reduce the risk of malpractice but its impact on the practice of DM will have to be specifically assessed. The second victims might benefit through the new law, in fact, the legal implications increase the negative psychological impact on the second victim.
Trial registrationThe article does not report the results of a controlled health-care intervention.
Provenance and peer reviewNot commissioned; externally peer reviewed.
FundingThis study was supported by The Italian Ministry of Health (“Medicina difensiva – Sperimentazione di un modello per la valutazione della sua diffusione e del relativo impatto economico” CUP I85J12002450001). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interestNone declared.
We thank Mr. Roberto Serra of the University of Eastern Piedmont for the informatic support he provided for the online survey.