To analyze the impact of implementing a therapeutic education (TE) program for patients with chronic migraine.
MethodProspective longitudinal intervention and assessment study before and after the program, lasting 6 months, conducted at the Headache and Facial Pain Unit of Hospital Clinic in Barcelona.
ResultsTE resulted in a significant improvement in the frequency of headache days per month, DCM (15.6 ± 6.84 vs. 11.5 ± 4.68; p < 0.001), migraine days per month, DMM (7.38 ± 1.44 vs. 5.88 ± 1.36; p < 0.001), and increased perception of quality of life, measured through the MSQ scale (65.4 ± 10.11 vs. 51 ± 11.36; p < 0.001). Regarding satisfaction, we can observe that 97.5% of patients who attended group sessions would recommend them to other people with migraines and, furthermore, considered the content to be good or excellent.
ConclusionsTE in the treatment of chronic migraine offers a promising improvement in the quality of life of patients by empowering them with knowledge about their condition and pain management strategies. This complements pharmacological treatments by focusing on prevention and self-care. Although more research is needed to establish standard protocols, the presence of advanced practice nurses in headaches is crucial for the successful implementation of these programs.
Analizar el impacto de la implantación de un programa de educación terapéutica (ET) para pacientes con migraña crónica.
MétodoEstudio longitudinal prospectivo de intervención y valoración antes y después del programa, con una duración de 6 meses realizado en la unidad de cefalea y algia facial de Hospital Clinic de Barcelona.
ResultadosLa ET resultó en una mejora significativa de la frecuencia de los días de dolor de cabeza al mes, DCM (15,6 ± 6,84 vs. 11,5 ± 4,68; p < 0,001), los días de migraña al mes, DMM (7,38 ± 1,44 vs. 5,88 ± 1,36; p < 0,001) y aumentando la percepción en la calidad de vida, medida a través de la escala MSQ (65,4 ± 10,11 vs 51 ± 11,36; p < 0,001). Respecto a la satisfacción podemos observar que el 97,5% de los pacientes que asistieron a las sesiones grupales las recomendarían a otras personas con migraña y, además, consideraron los contenidos como buenos o excelentes.
ConclusionesLa ET en el tratamiento de la migraña crónica ofrece una prometedora mejora en la calidad de vida de los pacientes al capacitar a estos con conocimientos sobre su condición y estrategias de manejo del dolor. Esto complementa los tratamientos farmacológicos al centrarse en la prevención y el autocuidado. Aunque se necesitan más investigaciones para establecer protocolos estándar, la presencia de enfermeras de práctica avanzada en cefaleas es crucial para la implementación exitosa de estos programas.
Migraine is a neurological condition characterised by headache attacks. The prevalence of migraine worldwide is 12%. Treatment is based on control of symptoms, prevention of symptoms and education.1,2
The WHO defines therapeutic education (TE) as “A continuous process of medical care, consisting of educational activities essential to the management of pathological conditions, managed by healthcare providers (HCPs), duly trained in the education of patients and designed to help a patient (or a group of patients and their families) to manage their treatment and prevent avoidable complications while keeping or improving their quality of life. TE covers organised activities, including psychosocial support, designed to make patients fully aware of their disease and to inform them about care, hospital organisation and procedures as well as health-and disease-related behaviours.” Its fundamental objectives are to provide information, plus practical knowledge to improve compliance with the therapeutic plan and, above all, to modify behaviour. An essential aspect is that it empowers patients to improve their disease through the acquisition of skills, as opposed to simply providing information.3
TE has been shown to effectively contribute to preventing complications and improving quality of life in numerous chronic diseases.4–7 In 2023, a TE programme for patients with chronic migraine was implemented at the Hospital Clínic of Barcelona. The programme is structured into multidisciplinary group visits, and addresses 3 topics: understanding the pathology, identifying triggers and consolidating hygienic-dietary habits, together with managing expectations and living with pain.
ObjectiveTo analyse what impact of the implementation of the TE programme had on patients with chronic migraine.
MethodDesignProspective longitudinal observational study carried out in the headache and facial pain unit of the Hospital Clínic in Barcelona.
Study periodBetween February and July 2023.
Study populationPatients treated in the headache and facial pain unit who met the following inclusion criteria:
- -
Subjects with a diagnosis of chronic migraine (>15 headache days per month) according to the international classification of headache disorders (ICHD).8
- -
Score >56 on the Headache Impact Test (HIT-6) scale.
Patients who met the following exclusion criteria were excluded from the study:
- -
Subjects diagnosed with episodic migraine (<15 headache days per month) according to the ICHD.
- -
Score <56 on the Headache Impact Test (HIT-6) scale.
Patients were included in the TE programme following the criteria described.
The programme lasted 6 hours divided into 4 sessions. It was structured in group visits in which the following people participated: neurologist, advanced practice nurse (APN) in headaches and psychologist.
The TE group consisted of 4 sessions per subject of 1.30 h/session, in groups of a maximum of 10 people. Standardised educational material and content were used based on 3 themes: understanding migraine; triggers and hygienic-dietary habits; expectations and living with pain.
The variables analysed were: sociodemographic (age, gender), clinical (days of headache per month [DHM], days of migraine per month [DMM]), intensity (using the visual analogue pain scale [VAS]), impact (Headache Impact Test [HIT-6]9), and quality of life (Migraine-Specific Quality of Life Questionnaire [MSQ]).]),10 which were assessed at the start of the programme and at 3 months.
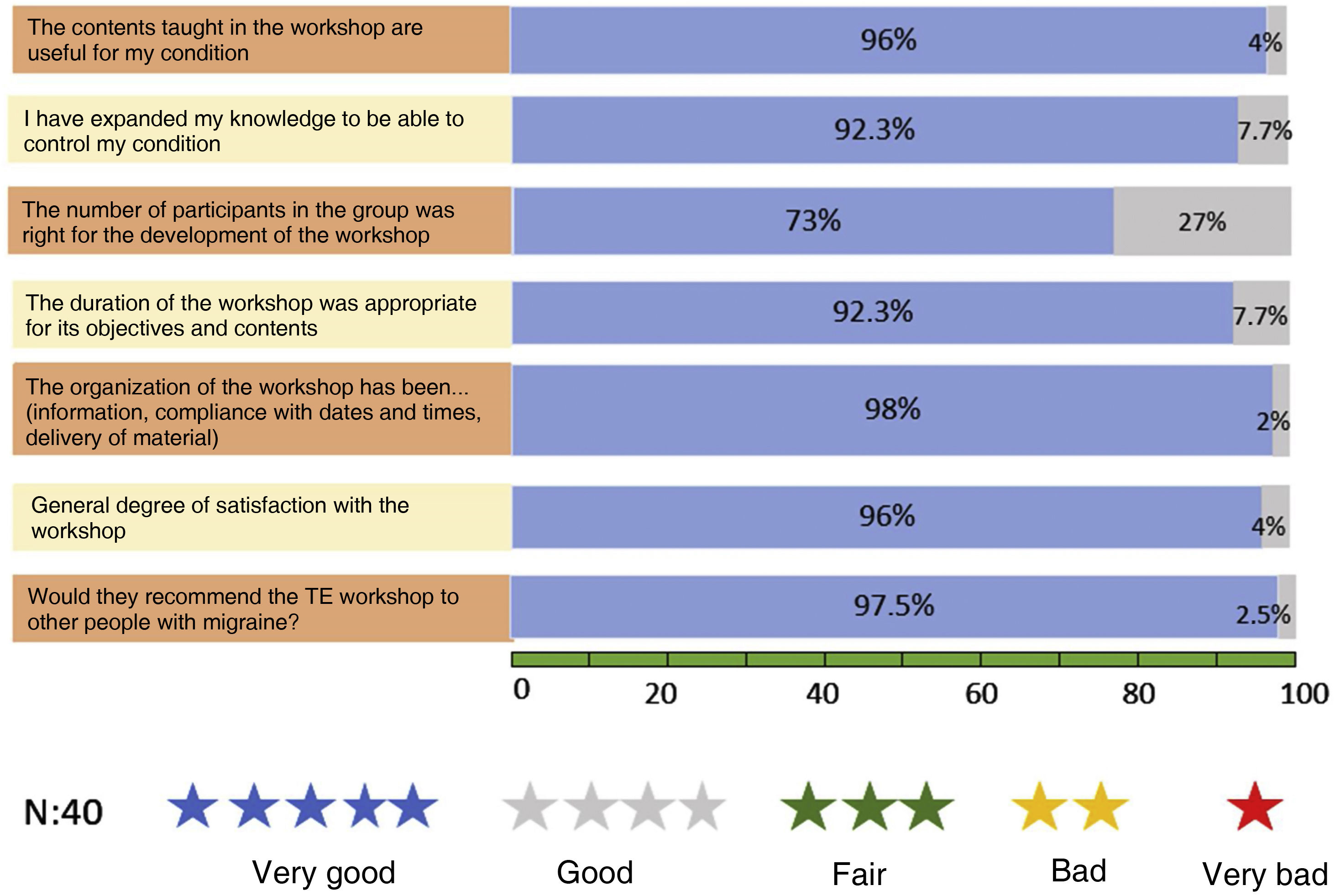
Patient experience and satisfaction with TE were also analysed, for which the opinion of the attendees of the group sessions was quantitatively evaluated anonymously using an ad hoc questionnaire at the end of the sessions and organisational variables were analysed, such as the number of subjects included and attendance.
Tools used- •
Visual analogue pain scale (VAS), which allows the intensity of the pain described by the patient to be measured with maximum reproducibility between observers. It consists of a 10-centimetre horizontal line, at the ends of which are the extreme expressions of a symptom. On the left is the absence or lesser intensity and on the right is the greatest intensity. The patient is asked to mark on the line the point that indicates the intensity and it is measured with a millimetre ruler. The intensity is expressed in centimetres or millimetres. The assessment will be: 1 “Mild pain” if the patient rates the pain as less than 3. 2 “Moderate pain” if the assessment is between 4 and 7. 3 “Severe pain” if the assessment is equal to or greater than 8.
- •
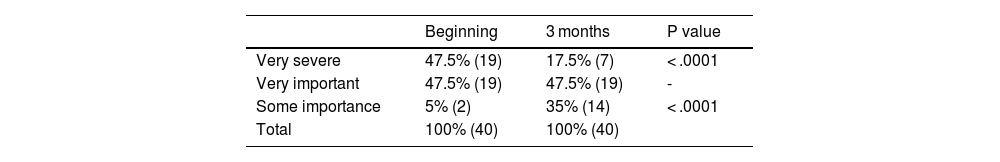
Impact (Headache Impact Test or HIT-6),9 which is a functional impact measurement tool for headaches consisting of 6 items that assess the frequency of intense headaches, the limitation of daily activities, including work, school and social settings, desire to lie down in bed, fatigue, irritability and difficulty concentrating. This scale scores 60 or more as very severe impact, 56–59 as significant impact, 50–55 as some impact and 49 or less as little or no impact.
- •
Quality of life (Migraine-Specific Quality of Life Questionnaire or MSQ),10 is a specific questionnaire for migraine designed to assess limitations in quality of life and the effect of treatments. It is structured into 3 domains that assess reduction or prevention in socializing, work-related activities and emotions related to migraine; version 2.1 improved its content for greater clarity and was shortened to facilitate administration. The results of this questionnaire range from 14 to 84, with higher scores meaning a worse quality of life.
- •
Patient experience and satisfaction with TE, ad hoc questionnaire, which has 7 questions and is rated with stars, with 5 stars being “very good”, 4 stars “good”, 3 stars “fair”, 2 stars “bad” and 1 star “very bad.”
The study was conducted according to the ethical principles established in the Declaration of Helsinki. This includes approval by the centre’s research ethics committee, and the fact that the subjects were informed of the study, and participated voluntarily, certifying this by signing the written informed consent.
Data analysisData processing and analysis was performed using the SPSS statistical program version 29.0. Student’s t-test for independent samples was used for quantitative variables and Pearson's χ2 test for qualitative variables, with a significance level of α = .05. The results were presented as mean ± standard or deviation proportions.
ResultsForty individuals who met the inclusion criteria (chronic migraine and score >56 on the HIT-6 scale) were analysed. 80% were women (32) and 20% men (8), with a mean age of 41.44 years (±13.48), with 66.6% attending the TE programme and 24 sessions.
Eighty-seven-point five percent (35) of the subjects were included due to therapeutic indication and 12.5% due to poor control of migraine crises.
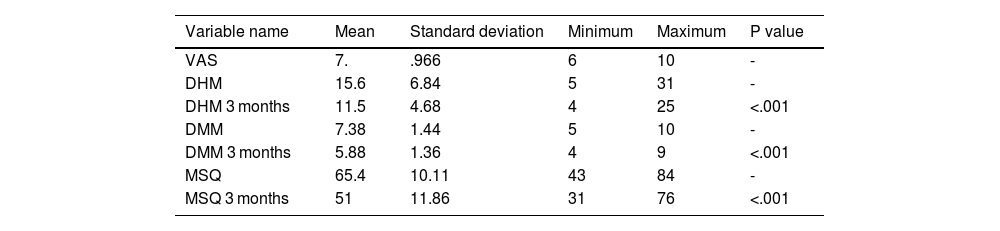
Table 1 shows the results of the pre- and post-intervention clinical variables. Statistically significant improvement was seen in the reduction of DHM (15.6 ± 6.84 vs. 11.5 ± 4.68; p < .001), DMM (7.38 ± 1.44 vs. 5.88 ± 1.36; p < .001) and an increase in the perception of quality of life, measured by the MSQ scale (65.4 ± 10.11 vs. 51 ± 11.36; p < .001).
Pre and post intervention clinical variables.
| Variable name | Mean | Standard deviation | Minimum | Maximum | P value |
|---|---|---|---|---|---|
| VAS | 7. | .966 | 6 | 10 | - |
| DHM | 15.6 | 6.84 | 5 | 31 | - |
| DHM 3 months | 11.5 | 4.68 | 4 | 25 | <.001 |
| DMM | 7.38 | 1.44 | 5 | 10 | - |
| DMM 3 months | 5.88 | 1.36 | 4 | 9 | <.001 |
| MSQ | 65.4 | 10.11 | 43 | 84 | - |
| MSQ 3 months | 51 | 11.86 | 31 | 76 | <.001 |
Table 2 shows the results of the impact variable (HIT-6), measured at baseline and at 3 months, where it can be seen that the impact of headache (HIT-6) was significantly reduced after the intervention in the groups that scored as very severe (47.5% vs. 17.5%; p < .0001) and somewhat severe (5% vs. 35%; p < .0001).
Fig. 1 shows the results of the satisfaction survey. The overall assessment was positive, with the information and content being considered very good and good.
97.5% of those who attended the group sessions would recommend them to other people with migraine.
DiscussionThe implementation of the TE programme for patients which chronic migraine was the purpose of the interest in the scientific literature. Our study measures the efficacy and impact of a multidisciplinary TE programme for patients with chronic migraine led by the advanced practice nurse, and in this context the results of our study align with previous research that has evaluated the effectiveness of TE programmes in the management of other chronic pathologies such as diabetes.11
A previous study evaluated patient satisfaction with educational information leaflets, finding that the use of such leaflets was understandable and increased overall knowledge about the disease. In addition, patients considered this information to be useful in improving their migraine control.7 These findings support the importance of providing patients with education about their disease to empower patients in its management.
Furthermore, a review on neuroscience education as a therapy for migraine12,13 highlighted that the combination of TE with traditional pharmacological treatments represents a promising therapy. This review found that TE not only reduces the frequency of migraine days, but also the intensity and duration of pain, as well as the need for acute medications. These results underscore the value of comprehensive approaches that combine both education and pharmacotherapy in the treatment of chronic migraine.
Our study shares these results from the review and provides additional evidence in support of these conclusions, by demonstrating that a structured TE programme for patients with chronic migraine can lead to significant improvements in the frequency and intensity of migraine attacks, as well as in the functional impact and quality of life of patients with chronic migraine.
These results support the efficacy of TE as an integral part of chronic migraine management, providing patients with additional tools to effectively manage their disease and improve their overall well-being.
However, it is important to recognise that the effectiveness of TE may vary depending on the specific population and context, and that further research is required to fully understand its long-term impact and relationship to other therapeutic approaches.
ConclusionThe findings of our study support the effectiveness of TE as an integral part of chronic migraine management, and demonstrate that a multidisciplinary and structured TE programme for patients with chronic migraine at Hospital Clínic de Barcelona had a significant impact on multiple aspects of the disease, resulting in a positive impact on quality of life and reduction in the frequency of headache days and attacks, during the first 3 months of implementation.
These results support the integration of TE programmes into the clinical care of chronic migraine as an effective strategy to improve clinical outcomes and quality of life for patients. However, further research is needed to establish standardised protocols and evaluate the long-term effectiveness of these programmes to fully understand the role of TE in chronic migraine management and its relationship to other therapeutic approaches.
Ultimately, TE in chronic migraine represents a promising approach to the comprehensive management of this disease, offering hope and improving the quality of life of those who suffer from it.
In addition to this, the advanced practice headache nurse is a facilitator in the multidisciplinary team, as they are responsible for the implementation of these programmes.
FundingNo funding.
Conflict of interestsThe authors have no conflict of interests to declare.
My thanks to my colleagues, the advanced practice neurology nurses at Hospital Clínic, for encouraging me to develop and implement a therapeutic education programme in the headache and facial pain unit.