To determine the degree of autonomy of patients treated with mechanical thrombectomy; to assess the degree of neurological deficit on admission and 24 h, and the degree of dependency at 3 months after performing the mechanical thrombectomy.
MethodQuantitative, observational, and descriptive study, with a sample of 57 patients treated with mechanical thrombectomy in the Autonomous City of Buenos Aires. Neurological deficit was measured with the National Institute of Health Stroke Score upon admission and 24 h after treatment with mechanical thrombectomy, and functional outcome with the modified Rankin scale at three months.
ResultsThe degree of dependency at three months was 2,4 points. The mean neurological deficit score on admission was 12,1 points, and 9,3 points after 24 h. Neurological deficit at 24 h has been found to be predictive of functionality at three months.
ConclusionThe mean of the neurological deficit at admission was situated in a moderate neurological deficit. The mean of the neurological deficit at 24 h has been placed in a moderate neurological deficit. The score for the degree of dependency at three months was placed in the mild disability category. A significant correlation has been obtained between the neurological deficit at 24 h and the functional result at three months.
Determinar el grado de autonomía de los pacientes tratados con trombectomía mecánica; evaluar el grado de déficit neurológico al ingreso y a las 24 horas y el grado de dependencia a los tres meses tras la realización de la trombectomía mecánica.
MétodoEstudio cuantitativo, observacional y descriptivo, con una muestra de 57 pacientes tratados con trombectomía mecánica en la Ciudad Autónoma de Buenos Aires. El déficit neurológico ha sido medido con la National Institute of Health Stroke Score al ingreso y tras las 24 horas del tratamiento con trombectomía mecánica y el resultado funcional con la escala de Rankin modificada a los tres meses.
ResultadosEl grado de dependencia a los tres meses se ha situado en 2,4 puntos. La puntuación media del déficit neurológico al ingreso ha sido de 12,1 puntos, a las 24 horas de 9,3 puntos. El déficit neurológico a las 24 horas ha resultado ser predictivo de la funcionalidad a los tres meses.
ConclusiónLa puntuación media del déficit neurológico al ingreso se ha situado en un déficit neurológico moderado. La puntuación del déficit neurológico a las 24 h se ha situado en un déficit neurológico moderado. La puntuación del grado de dependencia a los tres meses se ha situado en la categoría discapacidad leve. Se ha obtenido correlación significativa entre el déficit neurológico y el resultado funcional.
Stroke is among the leading casus of disability and demise world over; specifically, acute stroke is the third cause of mortality, the number one cause of disability in the adult population of developed nations, and the second most common cause of dementia.1 In 2015, a group of randomised clinical trials demonstrate functional benefits three months after stroke in a group of patients treated with mechanical thrombectomy and alteplase compared to the group treated with alteplase alone. 2–5
The HERMES meta-analysis categorised earlier trials and revealed that endovascular thrombectomy added to alteplase doubled the possibilities of achieving a higher score on the modified Rankin Scale compared to alteplase alone, when the damages are associated with a previous occlusion of large vessels, even among the elderly, 300 min after the stroke.6 This means that, since the year 2015, different neurology societies and clinics agreed to mechanical thrombectomy as the optimal treatment option in cases of acute stroke.4,6–9 The DEFUSE 3 Study concluded that endovascular thrombectomy, when undertaken within up to 16 h from the time the patient was last known to be well, in subjects with reversible perfusion images, enhanced functional outcomes.6 The initial characteristics of stroke severity are always recorded and represent the best parameter prior to treatment to predict the results and to have a preliminary idea of the resources that will be needed to care for the individual after the stroke. The indicators of stroke severity that include post-treatment information can be predictive of clinical and functional outcomes. For instance, the change in the National Institute of Health Stroke Score (NIHSS) proved to be the single most powerful predictor of functional results 90 days after a stroke.1,3,4,6
On the other hand, the extent of stroke involvement can be assessed using the mRS, which is the most widely used measure in studies published in recent decades.1
At 90 days, the mRS is also the primary outcome measure recommended for use in studies of acute stroke, made by the European Stroke Organisation (ES0) task force. Repeated assessments of the severity of the stroke are routinely collected in research studies on stroke and are a chance to evaluate the longitudinal data regarding functional outcomes after patient discharge.1
Some studies correlate the long-term results with stays in specialised and critical care units and have determined that reperfusion does not appear to be the sole determinant of good functional outcomes within this context, but that other aspects, such as the individual’s intrinsic characteristics and specific aspects of care in critical care units, could play a role that could, in fact, potentially undermine the positive effects of reperfusion and have a very different impact on short- and long-term functional outcomes.6
The premises underlying the effect of nursing care in clinical settings (interventionistic neurology rooms, critical care units, stroke units, units specialised in neurology) on short- and long-term results involved the nursing staff having drafted clinical practice guidelines that put forth the best nursing interventions and activities to obtain the best recovery possible of acute stroke patients’ autonomy. Among such nursing interventions, we would emphasize recording the evolution of the person’s neurological status using the NIHSS, as well as the having the nurses record subjects’ functional evolution by means of the mRS, with the aim of ensuring ongoing evaluations from «needle time» (initiation of the thrombectomy in the intervention room) until the individual is discharged.3,6,9–12 The Best Practice Guidelines and a number of evidence-based nursing studies currently published state that the nurse shall be responsible for administering and managing these scales, not only with an eye to improving communication between professionals, but also the neurological and functional status of the patient through holistic, continuous care and monitoring.6–8,13
Therefore, this study pursues the aim of assessing the determinants to implement in protocols that are appropriate in the unit and thereby enhance the quality of care, as well as continuity of nursing care.
ObjectivesThe main objective of this work is to establish the degree of autonomy of those patients who were treated with mechanical thrombectomy. Secondary aims include: to evaluate the degree of neurological deficient at the time of admission and 24 h after treatment with mechanical thrombectomy, to assess the level of dependence at three months of the mechanical thrombectomy, and to correlate the neurological deficit and the degree of dependence.
MethodsStudy design and patientsThis is an observational, descriptive, retrospective study of a case series of patients with occlusions of the middle cerebral artery in the M1 or M2 branches who underwent mechanical thrombectomy at La Clínica La Sagrada Familia (Ciudad Autónoma de Buenos Aires) between 1 January 2016 and 20 April 2017.
Patient selectionThe inclusion criteria consisted of acute obstruction of the anterior cerebral artery, older than 18 years, with a NIHSS of 6 points or more. All the participants receiving intravenous thrombolysis prior to the intervention within no more than 4.5 h of the onset of stroke symptoms, in line with the ESO guidelines.17
The following comprised the exclusion criteria: (1) the presence of intracranial haemorrhage, (2) ischaemic stroke as established by the Alberta Stroke Program Early CT Score (ASPECTS) of less than 6 points, (3) pregnancy, and (4) subjects allergic to contrast.
Variables and data collectionIn order to carry out this study, sociodemographic variables (affiliation, age, sex, and start date of the study) were collected, in addition to the degree of neurological deficit at the time of admission and at 24 h and the degree of autonomy at 3 months.
Description of the assessment toolsNational Institute of Health Stroke ScoreThe NIHSS uses a numerical score to describe the severity of the stroke in terms of the neurological deficit. This scale must be administered at the beginning and during the evolution of the stroke. Scores range from a minimum of 0 points and a maximum of 42 points. Results are categorised as follows: Asymptomatic: 0 points; Minor neurological deficit: 1 point; Mild neurological deficit: between 2–5 points; Moderate neurological deficit: between 6–15 points; Important neurological deficit: between 16–20 points, and Severe neurological deficit: more than 20 points.6
Modified Rankin ScoreThe mRS is used to quantify the functional outcome and degree of autonomy after stroke and is one of the most widely used scales for this purpose. Scores range from 0 to 6 points. The categories are defined based on the following classifications: 0 points: asymptomatic; 1 point: minimal disability; 2 points: mild disability; 3 points: moderate disability; 4 points: moderately severe disability; 5 points: severe disability, and 6 points: demise.6
Study outcome measuresThe clinical result was measured as the degree of autonomy as established by the mRS at 90 days of the stroke. A good outcome was classified as mRS ≤ 2 and a poor outcome was defined as mRS ≥ 3.
Statistical and data analysisA descriptive analysis was performed using measures of central tendency (mean [M] or median) and dispersion (standard deviation [SD]) where appropriate for quantitative variables, and percentages for qualitative variables).
Intergroup differences were examined by means of the chi-squared test for qualitative variables. Statistical significance was set at 0.05 to choose those variables that were ultimately included in the binary logistic regression model. All analyses and calculations were performed using the PASW statistical software package (v. 24.0; SPSS Inc., Chicago, Illinois, USA).
Ethical aspectsThe study was approved by the Santiago-Lugo Research Ethics Committee on 20 September 2018 with registration code 2018/335. It has likewise been authorised by the ethics committee of the Eneri Institute and by the administration of the Clínica La Sagrada Familia (Ciudad Autónoma de Buenos Aires, Argentina).
ResultsThe sample consisted of 57 patients who were treated with mechanical thrombectomy. Categorised by sex, the sample was 52.6% male (n = 30) and 47.4% (n = 27) female. Table 1 presents the contingency table with the sample characteristics.
Contingency table for sample characteristics.
| N | Percentage | Mean | SD | Q1 | Q2 | Q3 | LI | LS | |
|---|---|---|---|---|---|---|---|---|---|
| Sex | 57 | ||||||||
| Female | 27 | 47.4 | |||||||
| Male | 30 | 52.6 | |||||||
| Year | 57 | ||||||||
| 2016 | 41 | 71.9 | |||||||
| 2017 | 16 | 28.1 | |||||||
| NIHSS upon admission | 57 | 12.1 | 7.3 | 5 | 13 | 17 | 0 | 35 | |
| Asymptomatic (0) | 1 | 1.8 | |||||||
| Minor neurological deficit (1) | 1 | 1.8 | |||||||
| Mild neurological deficit (2–5) | 13 | 22.8 | |||||||
| Moderate neurological deficit (6–15) | 22 | 38.6 | |||||||
| Important neurological deficit (16–20) | 14 | 24.6 | |||||||
| Severe neurological deficit >20 | 6 | 10.5 | |||||||
| NIHSS at 24 h | 57 | 9.9 | 9.3 | 3 | 6 | 16 | 0 | 35 | |
| Asymptomatic (0) | 4 | 7 | |||||||
| Minor neurological deficit (1) | 4 | 7 | |||||||
| Mild neurological deficit (2–5) | 19 | 33.3 | |||||||
| Moderate neurological deficit (6–15) | 15 | 26.3 | |||||||
| Important neurological deficit (16–20) | 6 | 10.5 | |||||||
| Severe neurological deficit >20 | 9 | 15.8 | |||||||
| mRS at 3 months | 57 | 2.4 | 2 | 0.5 | 2 | 4 | 0 | 6 | |
| 0 (Asymptomatic) | 14 | 24.6 | |||||||
| 1 (Minimal disability) | 10 | 17.5 | |||||||
| 2 (Mild disability) | 7 | 12.3 | |||||||
| 3 (Moderate disability) | 8 | 14 | |||||||
| 4 (Moderately severe disability) | 8 | 14 | |||||||
| 5 (Severe disability) | 6 | 10.5 | |||||||
| 6 (Demise) | 4 | 7 |
NIHSS: National Institute of Health Stroke Score.
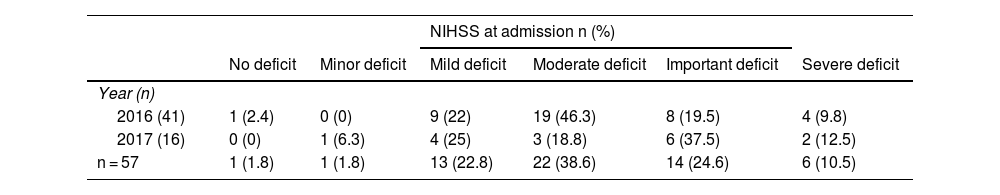
Insofar as neurological functioning at the time of admission is concerned, the mean NIHSS score was 12.1 (±7.3) points, meaning that the deficit in neurological functioning was moderate. By year, the neurological deficit at admission in 2016 was largely regarded as moderate with the mean HIHSS of 12 (±7.11) points, while it was deemed important in 2017 with a score of 12.5 (±8.02) points. The mean value of the NIHSS at 24 h was 9.9 (±9.3) points, which reflects a moderate degree of deficit. Again, by year, the neurological deficit at 24 h of admission was mostly considered mild in the year 2016, with a mean score for that year of 11.15 (±10.9) points and moderate for the following year 2017, with a mean score of 6.75 (±5.76) points.
The distribution of the neurological deficit at 24 h by year reveals a decrease in the proportion of important deficit (>10%) and an increase in the categories of no deficit (>5%), minimal deficit (>5%), and mild deficit (>10%) in comparison with the results at the time of admission.
With respect to functioning or dependence at three months, the mean was 2.4 (±2) points, evincing a good functional outcome following treatment (mRS ≤ 2 points). The degree of functioning at three months was mainly no deficit in the year 2016 with a mean score of 2.56 (± 2.14) points and very mild in the year 2017 with a mean score of 1.81 (± 1.33) points.
Table 2 presents the results by category of neurological deficit on admission and at 24 h and on functioning at three months.
Distribution of NIHSS at the time of admission by year.
| NIHSS at admission n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|
| No deficit | Minor deficit | Mild deficit | Moderate deficit | Important deficit | Severe deficit | |||
| Year (n) | ||||||||
| 2016 (41) | 1 (2.4) | 0 (0) | 9 (22) | 19 (46.3) | 8 (19.5) | 4 (9.8) | ||
| 2017 (16) | 0 (0) | 1 (6.3) | 4 (25) | 3 (18.8) | 6 (37.5) | 2 (12.5) | ||
| n = 57 | 1 (1.8) | 1 (1.8) | 13 (22.8) | 22 (38.6) | 14 (24.6) | 6 (10.5) | ||
| NIHSS at 24 h n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|
| No deficit | Minor deficit | Mild deficit | Moderate deficit | Important deficit | Severe deficit | |||
| Year (n) | ||||||||
| 2016 (41) | 3 (7.3) | 3 (7.3) | 13 (31.7) | 8 (19.5) | 6 (14.6) | 8 (19.5) | ||
| 2017 (16) | 1 (6.3) | 1 (6.3) | 6 (37.5) | 7 (43.8) | 0 (0) | 1 (6.3) | ||
| n = 57 | 4 (7) | 4 (7) | 19 (33.3) | 15 (26.3) | 6 (10.5) | 9 (15.8) | ||
| mRS at 3 months n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | ||
| Year (n) | ||||||||
| 2016 (41) | 11 (26.8) | 6 (14.6) | 3 (7.3) | 5 (12.2) | 6 (14.6) | 6 (14.6) | 4 (9.8) | |
| 2017 (16) | 3 (18.8) | 4 (25) | 4 (25) | 3 (18.8) | 2 (12.5) | 0 (0) | 0 (0) | |
| n = 57 | 14 (24.6) | 10 (17.5) | 7 (12.3) | 8 (14) | 8 (14) | 6 (10.5) | 4 (7) | |
NIHSS: National Institute of Health Stroke Score.
Based on this study, it has been determined that for the sample studied in the Ciudad Autónoma de Buenos Aires, the value of the outcome of the neurological deficit after categorisation, may be predictive of functionality (mRS), achieving a level of statistical significance with a 95% CI with the exception of the score for the deficit at the time of admission, which has not reached statistical significance (Table 3).
Significance level Significance level based on the Chi-square test between NIHSS outcome categorised at admission as prognostic of functionality (mRS) at discharge and at 3 months. (A) NIHSS score categorised at 24 h as prognostic of functionality (mRS) at discharge and at 3 months. (B) Sex as variable predictive of function quantified using the mRS at 3 months and (C) at a 95% CI.
| A | NIHSS at admission n (%) | ||||||
|---|---|---|---|---|---|---|---|
| No deficit | Minor deficit | Mild deficit | Moderate deficit | Important deficit | Severe deficit | P value | |
| mRS at 3 months (n) | 0.6 | ||||||
| 0 (14) | 0 (0) | 1 (7.1) | 6 (42.9) | 5 (35.7) | 2 (14.3) | 0 (0) | |
| 1 (10) | 0 (0) | 0 (0) | 3 (30) | 5 (50) | 1 (10) | 1 (10) | |
| 2 (7) | 0 (0) | 0 (0) | 3 (42.9) | 2 (28.6) | 1 (14.3) | 1 (14.3) | |
| 3 (8) | 1 (12.5) | 0 (0) | 0 (0) | 3 (37.5) | 3 (37.5) | 1 (12.5) | |
| 4 (8) | 0 (0) | 0 (0) | 0 (0) | 3 (37.5) | 3 (37.5) | 2 (25) | |
| 5 (6) | 0 (0) | 0 (0) | 1 (16.7) | 3 (50) | 2 (33.3) | 0 (0) | |
| 6 (4) | 0 (0) | 0 (0) | 0 (0) | 1 (25) | 2 (50) | 1 (25) | |
| n = 57 | 1 (1.8) | 1 (1.8) | 13 (22.8) | 22 (38.6) | 14 (24.6) | 6 (10.5) | |
| NIHSS a las 24 h n (%) | |||||||
|---|---|---|---|---|---|---|---|
| No deficit | Minor deficit | Mild deficit | Moderate deficit | Important deficit | Severe deficit | P value | |
| mRS at 3 months (n) | 0.001a | ||||||
| 0 (14) | 3 (21.4) | 3 (21.4) | 8 (57.2) | 0 (0) | 0 (0) | 0 (0) | |
| 1 (10) | 1 (10) | 1 (10) | 7 (70) | 1 (10) | 0 (0) | 0 (0) | |
| 2 (7) | 0 (0) | 0 (0) | 1 (14.3) | 5 (71.4) | 0 (0) | 1 (14.3) | |
| 3 (8) | 0 (0) | 0 (0) | 3 (37.5) | 4 (50) | 0 (0) | 1 (12.5) | |
| 4 (8) | 0 (0) | 0 (0) | 0 (0) | 2 (25) | 2 (25) | 4 (50) | |
| 5 (6) | 0 (0) | 0 (0) | 0 (0) | 3 (50) | 2 (37.3) | 1 (16.7) | |
| 6 (4) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (50) | 2 (50) | |
| n = 57 | 4 (7) | 4 (7) | 19 (33.3) | 15 (26.3) | 6 (10.5) | 9 (15.8) | |
| C | mRS at 3 months n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | P value | |
| Sex | 0.4 | |||||||
| Male (30) | 7 (23.3) | 8 (26.7) | 2 (6.7) | 4 (13.3) | 4 (13.3) | 2 (6.7) | 3 (10) | |
| Female (27) | 7 (25.9) | 2 (7.4) | 5 (18.5) | 4 (14.8) | 4 (14.8) | 4 (14.8) | 1 (3.7) | |
| n = 57 | 14 (24.6) | 10 (17.5) | 7 (12.3) | 8 (14) | 8 (14) | 6 (10.5) | 4 (7) | |
95% CI: 95% confidence interval; mRS: modified Rankin Scale; NIHSS: National Institute of Health Stroke Score.
As regards the primary objective of the present study, the NIHSS at the time of admission in the CABA zx was found to be 12.1, which sits squarely in the category of moderate neurological deficit. Compared to other studies, the mean NIHSS are seen to be variable; this must be probed in future studies, bearing in mind that incidence of stroke increases as the number of inhabitants in a given geographical location also rises. In 2022, CABA had a population of 3,120,612 inhabitants; thus, it would have been reasonable for in this study to have included more people under 65 years of age, who were fully autonomous at baseline and who had a moderate or important degree of neurological impairment following the ischaemic event.
The initial neurological deficit is moderate, similar to that reported by other authors; in the studies revised, they ranged from 6.62 to 17.5 points.1,7,14,15
As far as the first secondary objective is concerned, the mean NIHSS at 24 h was 9.9 points, which situates most of the sample in the category of moderate deficit.
After the first 24 h, we observed an improvement on the NIHSS of approximately 2 points. Compared to the main ECA zx, the HERMES meta-analysis detected an improvement of the NIHSS at 24 h of 3–6 points (control vs. intervention) and the MR CLEAN of between 2–4 points (control vs. intervention) using the PASWh statistical software package.1,16
The change of the NIHSS at 24 h with respect to the neurological deficit at the time of admission is particularly worth noting, noting that mechanical thrombectomy improves neurological functioning a mere 24 h following the intervention, inasmuch as the sample is distributed into lower degrees of deficit versus admission.1
With reference to the second secondary objective, the mRS functionality score was 2.4; i.e., exhibiting good functional recovery.
Finally, in view of the final secondary objective, the categorised NIHSS score has been correlated with the mRS, reaching significance in all cases with 95% CI, concluding that the NIHSS value at 24 h is a predictor of functionality at 3 months.
This study confirms that other markers of severity that include post-treatment information may be better predictors of clinical and functional outcomes. For instance, the change in NIHSS, the NIHSS of 24 h have proven to be the most powerful predictors of functional outcome three months following stroke, which is consistent with current evidence.17–19 Our study further underpins the importance of using the NIHSS score as a risk modifier in prognostic models for nursing care. Specifically, there is a 2-fold increased risk of mortality and approximately 3-fold greater risk of worsening ambulatory function with each 1-point increase on the NIHSS.20
The results of this study confirm practice in the trials of acute stroke that used the short-term mRS score as a primary endpoint with respect to patient functioning. The step change between mRS 2 and 3 for indirect death/disability and direct healthcare costs endorses the classical dichotomous result.20,21
Assessment of functional status during the subacute phase is recorded in only 24.6% of cases at discharge and for six months after the episode in the primary care database.7 The clinical benefit of stroke treatments is generally gauged on the basis of functional outcome measures evaluated at least three months after stroke and is usually measured using the mRS, which is the most prevalent outcome measure in trials published over the past decades.8,22
The mRS at 90 days is algo an outcome measure that the European Stroke Organization Task Force recommends for use in trials addressing acute stroke. Research has revealed that the increased severity as quantified by the mRS was associated with increased direct healthcare costs, postulating that a patient who has achieve an mRS score of 0 thanks to an expensive treatment such as thrombectomy will incur little or no extrahospital cost, albeit they will have high direct medical costs.1,23
Short- and mid-term appraisals make it possible to forecast the needs and level of nursing care each patient will require, as well as enabling care to be individualised and neurological and functional interventions, care, and rehabilitation measures to activated early. Moreover, this continuity in the evaluation of neurological and functional deficit by means of the NIHSS y mRS provide nurses to foresee the allow nurses to anticipate the level of care required by the individual patient, as well as their needs, in particular by allowing for the prompt initiation of resources aimed at preventing bronchial aspiration, dysphagia, pressure ulcer formation, and postictus pain.3,6,7,24–26 Finally, in order to fully implement acute stroke care, consideration must be given to educational and discharge planning that can help families of stroke survivors to make long-term arrangements specific to the expected functional outcome. The family may find it necessary to modify the home environment, for instance by adding ramps to the house or grab bars in the shower, and by having easy-access beds. The sooner these plans are put in place, the sooner an impaired stroke patient can be discharged, thereby shortening the person's hospital stay. Routine management of the NIHSS and mRS will help nurses to activate resources in a timely manner and design better, more individualised health education interventions tailored to the person's needs.6,7
LimitationsTreatment outcomes cannot be extrapolated to other patients on the basis of what is offered to some subjects meeting certain inclusion criteria.
At the beginning of the study, the protocols were neither strict nor homogenous across our centres as far as subject inclusion or clinical follow up are concerned. No neuropsychological examination was performed specifically because of the tremendous diversity of patients collected in a retrospective study.
Our population was a hospital cohort withing a specific hospital community setting. A larger sample is needed, as well as a study of a variety of places in order to test the causality and predictive capacity before findings can be generalised. It has been impossible to establish the prior function status of the participants in this hospital cohort.
Moreover, the retrospective nature of this analysis can be the source of potential biases (selection bias due to the loss to follow-up and misclassification bias) that would have to be addressed in prospective studies.
ConclusionEnsuring that scales to assess neurological deficit, degree of autonomy, and ability to carry out basic activities of daily living are correctly recorded is a key aspect of nursing practice, for the purpose of ensuring that the necessary and sufficient resources are activated to manage rehabilitation in people who have suffered an ischaemic stroke. In this study, the degree of patient autonomy exhibited a satisfactory functional outcome following treatment (mRS ≤ 2 points). The mean neurological deficit score at admission and at 24 h was found to be moderate neurological deficit. The degree of dependency score at three months was determined as mild disability. Finally, a significant correlation was established between the neurological deficit at 24 h and the functional outcome at 3 months.
FundingThis study has not received any funding of any kind.
Conflict of interestsThe authors have no conflict of interests to declare.