Dental implant fixation techniques are widely studied in order to reduce surgical morbidity. Computer-guided flapless surgery has been considered an efficient alternative that presents several advantages and some limitations. This technique allows the virtual planning and simulation of the prosthetic-surgical treatment that can help predict the difficulties and limitations in order to reduce possible errors. In addition to the prosthetic predictability, computer-guided surgery enhances accuracy and reduces surgical morbidity. Thus, the aim of this study was to report on a 7-year follow-up of immediately loaded implants inserted into an edentulous maxilla using virtual planning and flapless surgery.
Las técnicas de fijación del implante dental se estudian ampliamente para reducir la morbilidad quirúrgica. La cirugía sin flapless guiada por ordenador ha sido considerada como una alternativa eficiente con varias ventajas y algunas limitaciones. Esta técnica permite la planificación virtual y simulación del tratamiento protésico quirúrgico con la predicción de las dificultades y limitaciones para reducir posibles errores. Además de la previsibilidad de prótesis, la cirugía guiada por ordenador mejora la precisión y reduce la morbilidad quirúrgica. Por lo tanto, el objetivo de este estudio fue reportar a 5 años de seguimiento de los implantes de carga inmediata insertados en un maxilar desdentado utilizando la planificación virtual y la cirugía sin colgajo. El presente caso prospectivo informó el éxito del tratamiento y destacó la importancia de la planificación, lo que justifica el costo de esta tecnología.
The association of the computer-guided surgery and the flapless approach became an efficient alternative for implants insertion with several advantages, such as preservation of peri-implant bone volume; faster surgery; more patient's comfort; reduced bleeding, edema and post-operative pain, faster recovery and soft tissue, including gingival margins and papilla.1
The technique of the computer-guided surgery is indicated for the absence of dental units, partial or total, both in maxilla and mandible, provided that there is enough quantity of bone for the implant installation. Furthermore, another factor to be assessed is the patient's mouth opening, which must be greater than 50mm between the residual alveolar ridge and the incisal of the teeth, to allow the placement of the surgical guide and appropriate positioning of the drill.2
However, the technique has some limitations, such as the poor visualization of anatomical structures and alveolar bone with a higher risk of perforation or fenestration in cortical and adjacent teeth, bone heating due to non-exposure of the tissue and poor bone refrigeration during osteotomy, and higher risk to implants malposition. In addition, it is also difficult to manipulate the soft tissue for a better adaptation of keratinized gingiva around the implant structures.3
Khorshid et al. (2014)4 described, as consequences of the limitations mentioned above, complications such as: (1) lack of primary stability of dental implant and impossibility of applying immediate loading due to the low bone density; (2) diameter and size of inadequate implants, which may cause the microfracture of bone during implant placement and possible fibrous and granulation tissue encapsulation around the implants; (3) surgical positioning different from the virtual planning.
Considering all those limitations, the technique should be performed by experienced professionals who have a previous knowledge about the conventional technique in addition to the specific selection of cases with enough bone thickness in the alveolar ridge.
Thus, the aim of this study was to describe the accurate fixation of implants submitted to immediate loading in an edentulous maxilla using computer-guided virtual planning associated to flapless surgery after a 7-year follow-up.
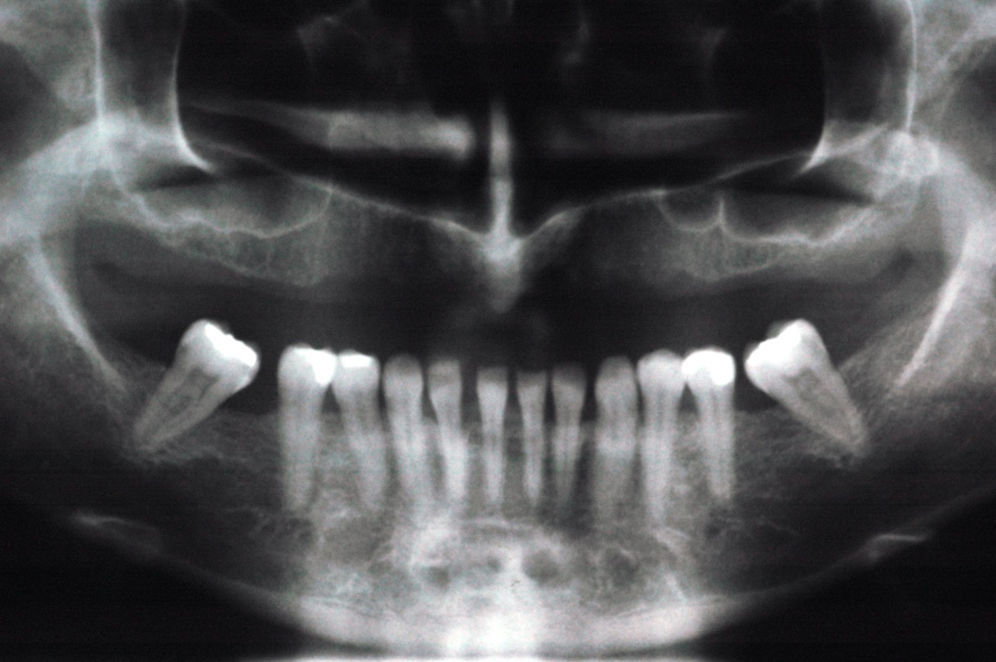
Case reportThe female Caucasian patient B.R.R., 38 years old, with good general health and edentulous maxilla for over 5 years, complained about esthetics and function of the maxillary complete denture. The patient presented natural teeth in mandible except for the right and left first molars (Fig. 1). After evaluation by experts in implantology, surgery and prosthodontics, the professionals indicated treatment using the Nobel Guide TM concept (Nobel Biocare AB) for virtual planning, flapless implant surgery and immediate loading of a maxillary screw-retained full-arch implant-supported denture.
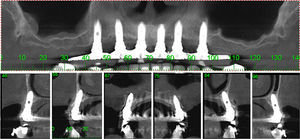
Initially, the case was transferred to a semi-adjustable articulator after confirmation of a mouth opening greater than 50mm and a low smile line. Functional wax try-in was conducted to determine better teeth positioning regarding esthetics, phonetics and occlusal vertical dimension. Duplication in colorless resin was carried out before computed tomography. A total of six perforations (1–1.5mm in diameter; 0.5mm in depth) were fabricated in the replica and 3 perforations were positioned at the buccal surface. The perforations were filled with gutta-percha (Tanari® – Tanariman Industrial Ltda, Amazonas, Manaus, Brazil) as radiopaque markers. Condensation silicone (Zetalabor® – Labordental, São Paulo, SP, Brazil) was used for inter-arch record in centric relation and occlusal vertical dimension. Computed tomography of the maxilla was conducted according to the “double-scan” technique, which shows several objects of different densities by two scans. The first scan was performed with the patient wearing the tomographic guide with radiopaque markers and inter-arch record. The second scan was made only for the tomographic guide. The tomographic slices presented 0.4mm in thickness and data were recorded as DICOM files to be transferred to the virtual planning software (Nobel Guide – Nobel Biocare AB). The virtual planning was accomplished by both surgeon and prosthetist to analyze implants length and distribution, abutment type, visualization of anatomic structures, and denture adaptation based on the direction of the abutment screws. After planning, data were used for the fabrication of the surgical guide by stereolitography. Implant analogs were attached to the surgical guide for the fabrication of the working cast with resilient artificial gingiva and dental stone. An inter-arch record was positioned between the surgical guide and the opposite arch in the articulator for transferring the position of centric relation and occlusal vertical dimension during surgery.
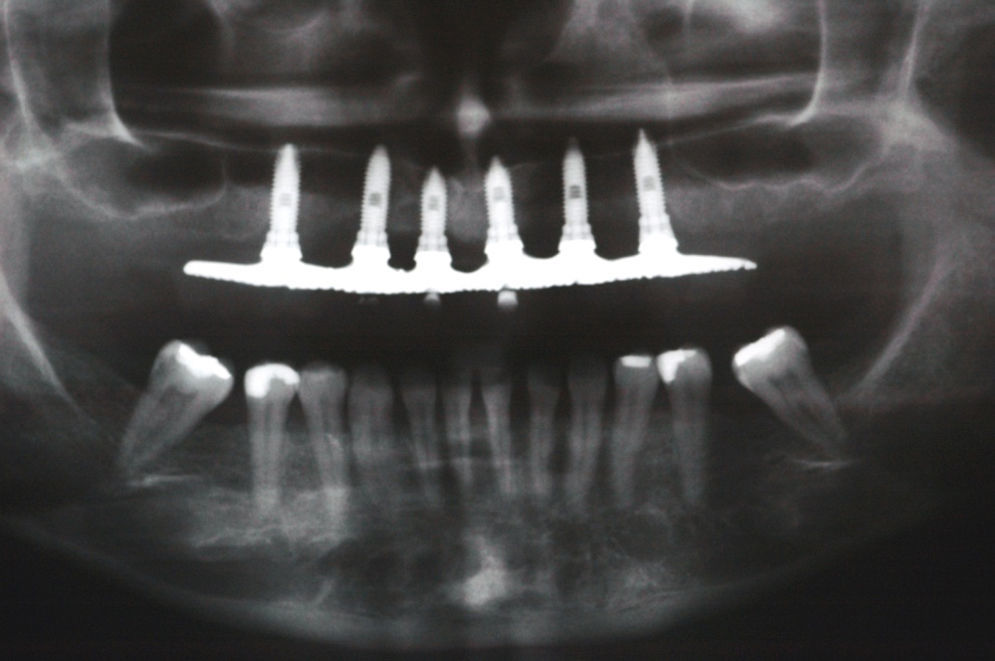
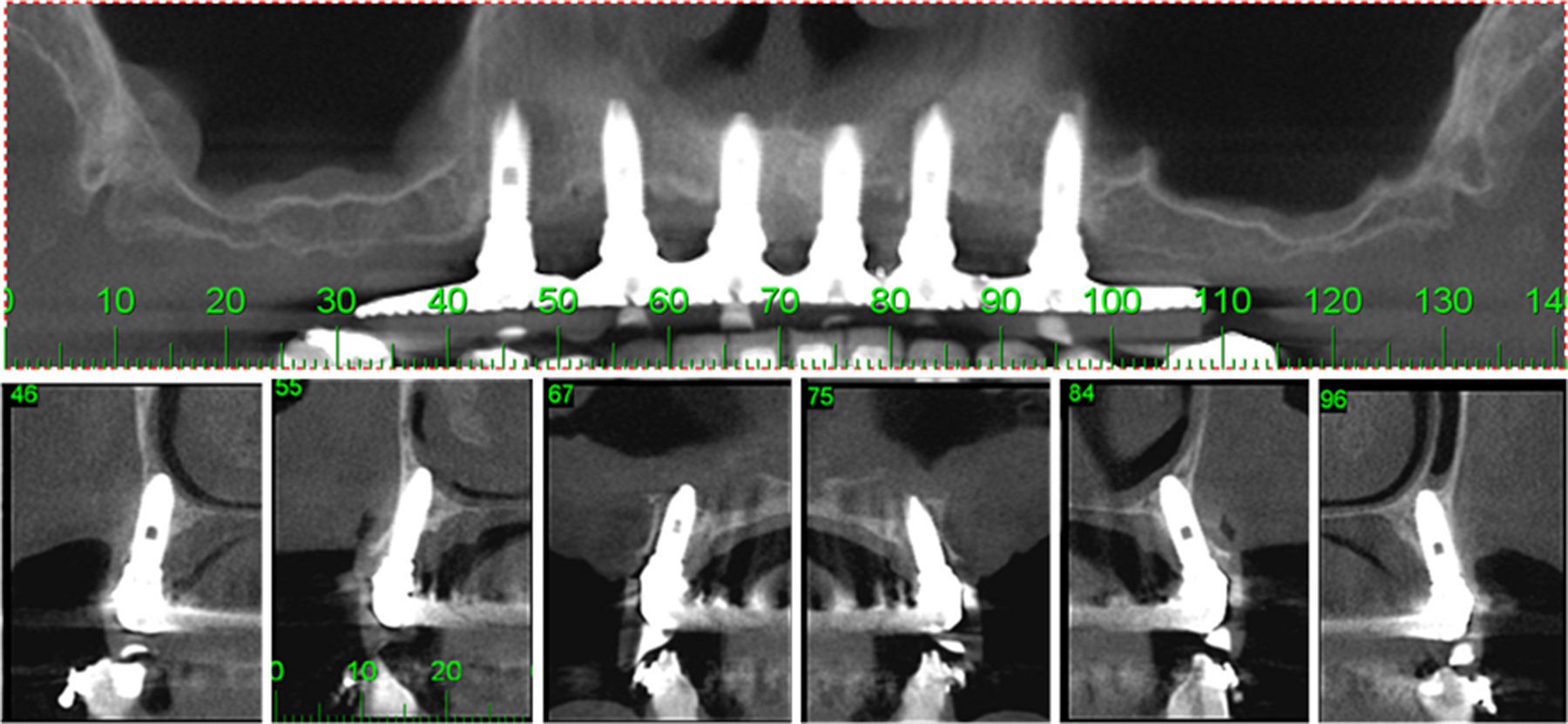
The flapless surgery was conducted under local anesthesia with 2% mepivacaine chloride and adrenalin 1/100,000 (Scandicaine 2% Especial – Septodont, Barueri, Brazil). The surgical guide was positioned and stabilized with anchorage screws fixed with a 1.5mm drill. Firstly, osteotomy and implant insertion were conducted at the right posterior region using the specific sequence of drills (Nobel Guide® – Nobel Biocare AB). Then, another implant was inserted at the left posterior region for further insertion of the anterior implants. The abutments (Neodent, Curitiba, Brazil) were attached to the implants with regular platform (Titamax EX® – Neodent, Curitiba, Brazil) (2mm mini-abutment – 3.75mm×13mm at right second premolar, 1mm mini-abutment – 3.75mm×13mm at left second premolar, 1mm mini-abutment – 3.75mm×13mm at right canine, 1mm mini-abutment – 3.75mm×13mm at left canine, 1mm mini-abutment – 3.75mm×11mm at right central incisor, and 1mm mini-abutment – 3.75mm×11mm at left central incisor). All implants presented initial torque values upper than 45Ncm (Figs. 2 and 3). After implants fixation, the components were attached for transfer impression. The impression copings were splinted with acrylic resin (Pattern Resin LS® – GC America INC, Alsip, USA) for stabilizing the assembly. The index was positioned and an addition of silicone (3M ESPE Express® – 3M, Sumaré, Brazil) was used for impression. Laboratorial procedures were conducted for the fabrication of the implant-supported denture with metallic framework based on the previous wax try-in. Periapical radiographs were obtained to check framework fit. The denture was inserted 48h after implants fixation and occlusal adjustments were conducted to avoid overloading (Fig. 4). The patient was informed about medication, diet and hygiene. Clinical and radiographic examinations were performed in a seven-year follow-up after implants insertion. The prosthesis was removed to assess mobility, pain, edema and integrity of implants and abutments. Plaque control, gingival sounding, occlusal contacts and mobility were routinely evaluated. No alteration was observed to suggest infection, prosthesis instability and implants mobility (Figs. 5 and 6).
DiscussionThe high-cost is one advantage of the computer-guided surgery associated with the flapless approach since specific software is needed for virtual planning and fabrication of the surgical guide. This financial limitation should be previously discussed with the patients. In addition, implant angulation can be influenced by poor visualization of bone tissue on implant surface after its fixation. Poor irrigation can be another disadvantage since bone heating may avoid osseointegration and cause implant loss.5 As an alternative, the professionals should be careful throughout the surgical procedure and intermittent movements should be conducted using new drills during osteotomy. Furthermore, patient's mouth opening must provide enough space for the placement of the surgical guide and the appropriate positioning of the drills.
A 44-month follow-up reported 42% of surgical and technical complication after the fixation of 176 implants submitted to immediate loading using the computer-guided flapless surgery. The authors suggested that this rate resulted from the lack of professionals’ experience.6 Another study about the limitation of the computer-guided surgery revealed that inaccuracy might occur during image acquisition, recording, software operation, fabrication of the surgical guide, and professionals’ mistakes.7
In this study, the patient complained about oral health due to poor esthetics and discomfort of the complete denture. Thus, immediate loading using the computer-guided flapless surgery was suggested. The 7-year follow-up revealed a positive result for the rehabilitation of the stomatognathic system. In addition, the patient's satisfaction was achieved since no post-operative complication was reported.
Although the computer-guided surgery presents higher cost and requires more accurate steps than the conventional technique, the satisfactory result reduces errors and ensures treatment predictability and accuracy. The present prospective case reported the treatment success and highlighted the importance of planning, which justifies the cost of this technology.
Conflicts of interestThe study was supported by Drs. Jéssica Lemos Gulinelli, Edilson José Ferreira, Marcos Rikio Kuabara, Thiago Borges Mattos, João Borges Mattos, Evandro José Germano and Pâmela Letícia Santos have no financial relation with any of the products involved in this study.