Selection of ideal anesthetic drugs in maxillofacial surgery.
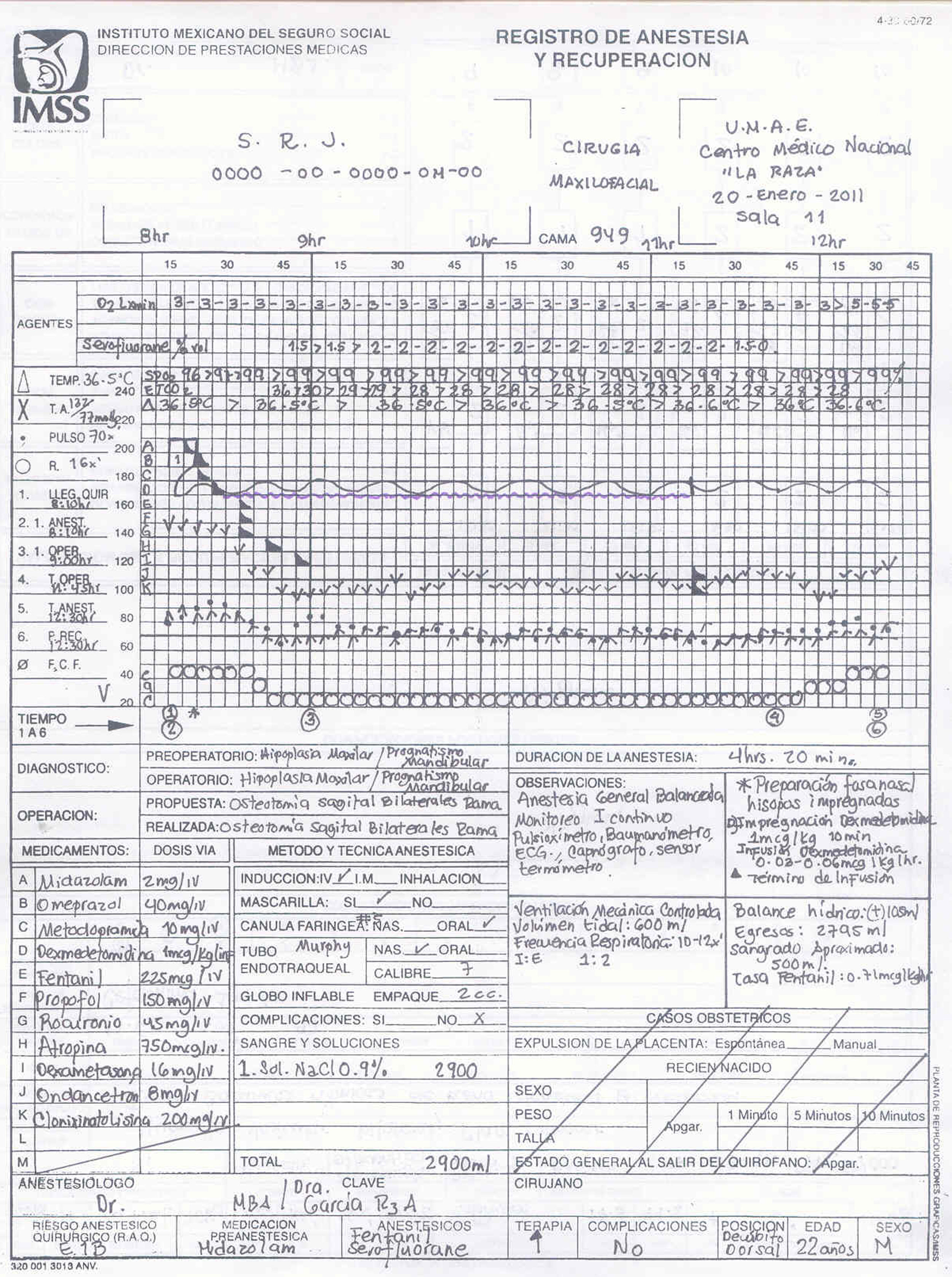
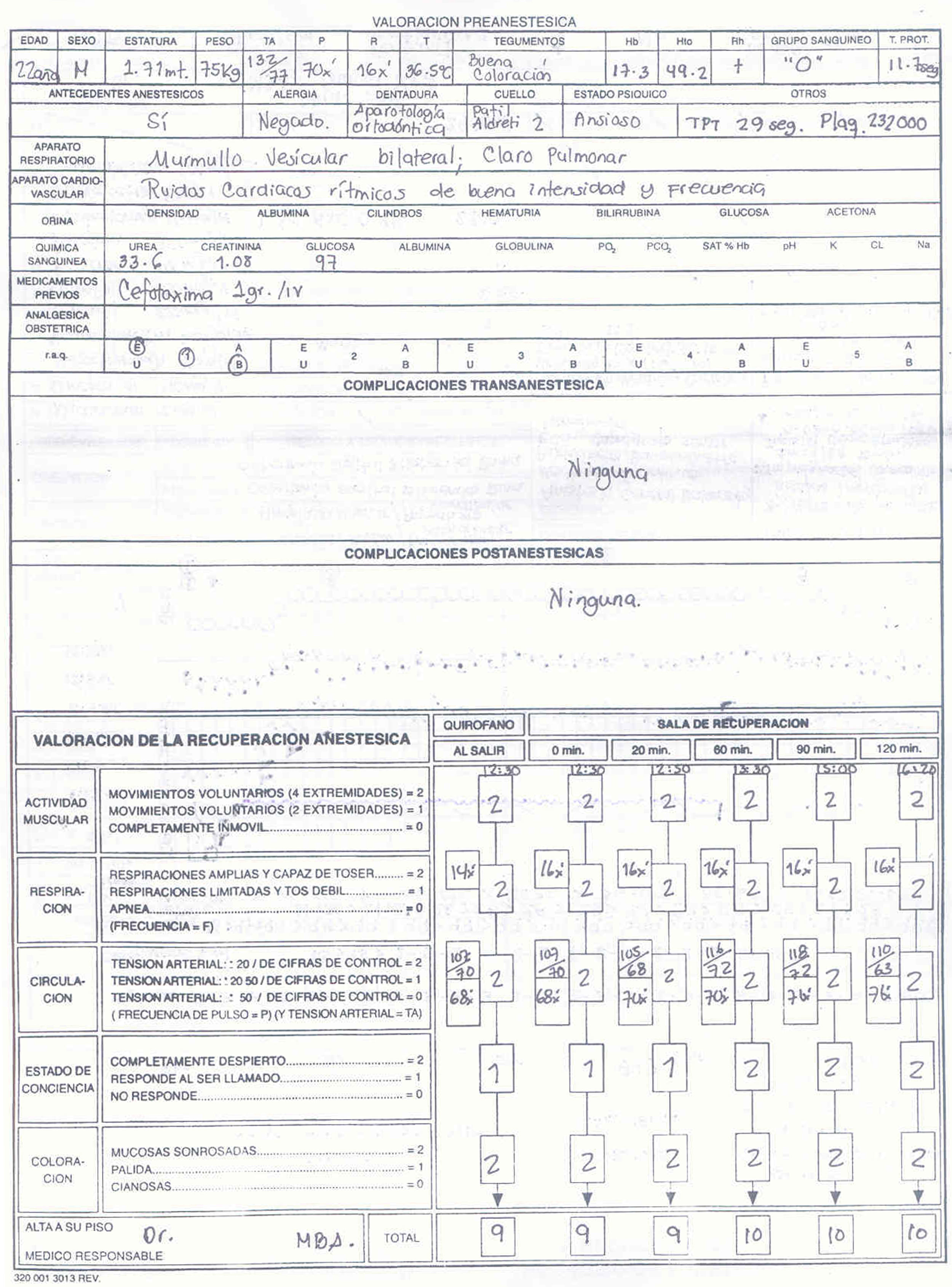
Material and methodsA 22-year-old male patient weighing 75kg and 171cm in height, with no premedication. Pre-operative vital parameters were BP 120/70, HR 72×min, SpO2 96%, temperature 36.5°C, sinus rhythm on 5-lead EKG, capnograpy. Patient was subjected to 5min of pre-oxygenation through a facial mask. The sniff test was performed, good ventilation was confirmed and a Q-tip impregnated in 0.05% oxymetazoline was applied. An intravenous continuous infusion of dexmedetomidine (solution concentration of 0.8μcg/ml) was initiated at a rate of 0.05mcg/kg/h with a score of 2 on the Ramsay scale. Induction was initiated with fentanyl 3mcg/kg, propofol 2mg/kg, rocuronium 0.6mg/kg. A No. 7 Murphy endotracheal tube lubricated with a 10% lidocaine spray was introduced through the right nostril down to the nasopharynx. At the start of surgery, the dose of dexmedetomidine was increased to 0.1mcg/kg/h. Intra-operatively, BP was maintained between 84/55mmHg and 90/53mmHg, and HR between 58 and 76 per minute.
ResultsThe selection of anesthetic drugs allowed for hemodynamic stability and comfort on awakening.
ConclusionAnesthesia for orthognathic surgery, as it has evolved today, requires combining different anesthetic techniques in order to ensure that the patient remains calm, comfortable and reassured, with adequate post-operative analgesia.
Selección de fármacos anestésicos ideales en cirugía maxilofacial.
Material y métodosVarón de 22 años, 75kg de peso y 171cm de altura. No premedicado. Parámetros vitales prequirúrgicos: PA 120/70; FC 72×min; SPO2 96%; temperatura 36,5°C; ECG 5 derivaciones ritmo sinusal, y capnografía. Preoxigenación por 5min mediante mascarilla facial. Se realiza prueba de olfateo corroborando buena ventilación, se coloca hisopo impregnado de oximetazolina spray 0,05%. Se inicia la administración de dexmedetomidina (concentración de solución 0,8μg/ml) en infusión continua por vía intravenosa a 0,05μg/kg/h con una escala Ramsay 2, se inicia inducción con fentanil 3μg/g, propofol 2mg/kg, rocuronio 0,6mg/kg. Se introduce por narina derecha tubo endotraqueal Murphy N.° 7, lubricado con lidocaína 10% spray, a través de la nasofaringe. Comenzando la cirugía se la ajusta dosis de dexmedetomidina a 0,1μg/kg/h. Durante el acto anestésico-quirúrgico se mantiene con PA entre 84/55 y 90/53mmHg, FC con cifras entre 58-76 por minuto.
ResultadosLa selección de los fármacos anestésicos permitió lograr la estabilidad hemo-dinámica y bienestar en el despertar del paciente.
ConclusiónLa anestesia para cirugía ortognática en la actualidad por su evolución hace necesario combinar diferentes técnicas anestésicas para poder proporcionar a los pacientes tranquilidad, seguridad, bienestar y analgesia postoperatoria.
Patient with maxillary hypoplasia and mandibular prognathism, scheduled for bilateral sagittal ramus osteotomy (Le Fort I). History: Prior appendectomy and third molar extractions with no anesthetic complications. Fentanyl plus dexmedetomidine were the drugs that came closest to the desired profile.
ObjectiveSelection of the ideal anesthetic drugs for induction and maintenance in maxillofacial surgery that offer supplemental analgesia, reliable and effective dosing to ensure adequate ventilation in the post-anesthetic care unit, and good hemodynamic stability.1
Material and methodsA 22-year-old male patient weighing 75kg and 171cm in height, with no premedication. Pre-operative vital parameters were BP 120/70, HR 72×min, SpO2 96%. Physical exam: oval-shaped face, increased cross-sectional diameter, broad forehead, unbalanced facial thirds with projection of the middle mandibular third; central nose, permeable nares, and no information regarding hypertrophic or hypotrophic turbinates; central mouth, short upper lip, incompetent lower lip. Intraoral examination: natural dentition with functional orthodontic appliance; Grade I mandibular protrusion; no information of macroglossia; Mallampati I. Temporomandibular Joint: finding of crepitation and mild pain under finger pressure that resolves when the maneuver is interrupted; distance between incisors greater than 3cm; mandibular space, 3cm; horizontal mandibular length is 11cm. Cylindrical neck with a circumference of 25cm; with neck flexion and extension, central trachea is mobile; the Patil–Aldrete distance is 6cm; atlanto-occipital joint Grade I extension, and cervical flexion greater than 90°.
Five minutes of pre-oxygenation through a facemask using 100% oxygen at a rate of 3L/min was used. The sniff test was performed and good ventilation was confirmed in both nares, although the patient reported better oxygenation through the right nostril. A Q-tip impregnated in a 0.05% oxymetazoline spray was placed in both nostrils for 10min. The administration of dexmedetomidine was initiated (solution concentration 0.8μc/ml) using a continuous intravenous infusion at 0.05mcg/kg/h with a score of 2 on the Ramsay scale. Narcosis was initiated using fentanyl at 3mcg/kg, and induction with propofol 2mg/kg. An oropharyngeal cannula (Guedel) was then placed, adequate ventilation was confirmed and a combination of rocuronium 0.6mg/kg plus atropine 10mcg/kg was used for relaxation, providing at the same time manual ventilation assistance for 5min. Direct laryngoscopy was then performed using the McCoy blade, visualizing a Cormack–Lehane Grade I; a No. 7 Murphy endotracheal tube lubricated with 10% lidocaine spray was introduced through the right nostril down to the nasopharynx. Magill forceps were then passed to the oropharynx and the tip of the tube was directed to the trachea, achieving intubation on first attempt. Vertex and basal auscultation was performed, confirming bilateral vesicular murmur and the presence of an ETCO2 capnography curve of 28–36mmHg. The patient was connected to 600ml tidal volume-controlled mechanical ventilation, set at a respiratory rate of 10–12, I:E 1:2, and 100% O2 at 2L/min, and with sevoflurane at 1.5–2vol%. At the start of surgery, the dose of dexmedetomidine was adjusted to 0.1μcg/kg/h. Throughout anesthesia and surgery, values were maintained as follows: BP between 84/55mmHg and 90/53mmHg, HR 58–70 per minute, ETCO2 28–29mmHg, and 99% SpO2 with stable hemodynamic condition. Overall fluid balance was (+) 105ml, with input of 0.9% NaCl 1900ml and Hartmann 1000, and 2795ml output, with approximately 500ml of blood loss. On completion of the surgical procedure, wound site hemostasis was checked and oropharyngeal secretions were suctioned. A Guedel cannula was placed, the vaporizer was closed and manually assisted ventilation support was maintained with 100% oxygen at 3L×min. Extubation was accomplished uneventfully upon recovery of protective reflexes (Fig. 1).
DiscussionNociception involves a series of mechanisms that code and transmit pain signals from the site where the noxious stimulation is produced at the periphery toward higher centers of the central nervous system (CNS).
The action of aspartate and glutamate receptor agonists as they bind to their receptors, results in hyperalgesia. Glutamate is the main excitatory amino acid of the CNS and may participate in nociceptive transmission at a spinal level. From the thalamus and the reticular substance, the stimulus is relayed to the cerebral cortex, the parietal lobe and the somatosensory area.
The efficacy of α-2 adrenergic agonists may vary depending on the surgical procedure. It has been shown that α-2-adrenergics reduce sympathetic tone, induce sedation, reduce heart rate (HR) and blood pressure (BP), and also diminish the metabolic response to stress during the perioperative period.
It is still unclear how to select the drug for perioperative maintenance, in particular in orthognathic surgery. It is of the utmost importance to perform an adequate assessment of the airway as well as to select drugs that may avoid respiratory depression, considering that the placement of inter-dental wiring is common, preventing rapid access in the post-operative care unit in the event of an emergency.2,3
In orthognathic surgery it is important to consider blood losses, and there are some specific drugs that may be selected, including clonidine and dexmedetomidine, which produce a significant increase in the incidence of perioperative hypotension, a pharmacological effect that may be of use in this type of surgery.4
Dexmedetomidine is a lipophilic imidazole derivative and a potent α-2 adrenergic agonist with an affinity eight times greater than that of clonidine for the α-2 adrenergic receptors.
Dexmedetomidine may be a very attractive option given the anesthetic considerations in these patients, because it does not produce respiratory depression, it reduces the post-operative use of opioids by up to 66%, and causes no depression of the ventilatory centers.
Its mechanism of action is through binding to the α-2-AR and activation of G proteins (guanine nucleotide-fixing regulatory proteins). This results in adenyl cyclase inhibition, lowering cAMP concentration.
α-2-AR agonists are used as analgesics and sedatives that act on the raphe magnus in the rostroventromedial region of the medulla, and are considered an important source of descending control of the spinal pain receptor neurons.
Their analgesic action is due to the inhibition of excitatory neurotransmitters in the spinal cord where there are large numbers of α-2-AR exciters.
Anti-nociceptive action: It occurs predominantly on the α-2-AR receptors in the spinal cord. Their systemic administration produces antinociceptive and sedative effects, whereas the intrathecal administration only produces an antinociceptive action. Hypnotic-sedative action: At sedative doses, they reduce cerebellar cGMP concentrations in the locus ceruleus in a dose-dependent fashion. This produces a dose-dependent reduction in the pre-synaptic release of noradrenaline in the ascending pathway to the cortex, as well as in the serotoninergic pathway, both associated with the transition from wakefulness to sleep.
Anesthetic action: They reduce the need for other drugs used for anesthetic induction and maintenance and this is related to the inhibitory effect on the noradrenergic central transmission. It has also been suggested that there is an additional site of action of the α-2 agonists, different from the auto-inhibiting presynaptic receptor of the noradrenergic pathways, that might mediate the concentration-reducing action on the minimum alveolar concentration (MAC) of volatile anesthetics.
Cardiovascular action: Stimulation of α-2-AR receptors in the spine, the brain and the periphery, produces an initial rise in blood pressure after the administration of dexmedetomidine as a result of the stimulation of peripheral vascular post-synaptic α-2 receptors. The drop in heart rate reflects baroreceptor stimulation, and the subsequent reduction in heart rate is due to sympathetic depression of central origin that leaves an unopposed vagal tone. Others believe that the hypotension that follows the initial hypertension is attributable to the peripheral vascular action because of the stimulation of pre-synaptic α-2-AR receptors, and it could also be explained by suppression of sympathetic nerve discharge.
Actions on the respiratory system: α-2-AR receptors have little participation in central control of respiratory function. Considering that non-REM sleep produces a descent in the slope and a 3–5mmHg displacement to the right on the hypercapnic ventilation response curve, the effects on respiration are explained on the basis of dexmedetomidine-induced sleep because of the action on the locus ceruleus and not on a more medullary level.
Renal action: They induce diuresis probably through the attenuation of antidiuretic hormone secretion or through the blockade of its effect on the renal tubules.
Endocrine actions: These actions relate to diminished sympathetic flow and the resulting reduction in circulating catecholamines. The stimulation of α-2-AR receptors localized in pancreatic beta cells would explain the tendency toward hyperglycemia resulting from reduced insulin secretion.
Ocular actions: α-2-AR agonists lower intraocular pressure by reducing aqueous humor formation through central or peripheral mechanisms.
Intestinal actions: Reduced salivary flow is due to a direct effect of α-2 agonists on α-2-AR receptors of the salivary glands and due to inhibition of acetylcholine release.
Cerebrovascular actions: Four actions have been identified in terms of the drugs’ influence on intracranial hemodynamics: (1) because of their action on presynaptic α-2A receptors, they reduce endothelin-1 production, and facilitate nitric oxide production; (2) because of their action on arteriolar smooth muscle α-2B receptors, they may increase tone directly and create vasoconstriction and hypertension effects (regional but also systemic), which apparently is achieved through the L-type calcium channels and with high doses; (3) through the sedative effect and their action on the locus ceruleus and activation of the metabolic–vascular coupling, they may promote vasoconstriction and, consequently, reduced cerebral blood flow (CBF) at least in some regions of the brain; and finally (4) the systemic effects of the drugs that induce bradycardia and hypotension may activate autoregulatory mechanisms with preserved CBF but with vasodilation and increased cerebral blood volume (CBV).
Clinical applications: The sympatholytic effects of dexmedetomidine are reflected in the lowering of blood pressure and heart rate, and norepinephrine release during the perioperative period. It does not cause respiratory depression, it has been approved by the FDA for use in intensive care since 1999, and now it has been approved for expanded use in anesthesia. This drug may attenuate increases in blood pressure and heart rate during the perioperative period; moreover, it may reduce the need for opioids and inhaled anesthetic agents as adjuncts during general anesthesia. In terms of side effects, dry mouth is common to α-2 agonists, and it was reported in three of the subjects participating in the different studies.
The use of short-acting anesthetics, added to the administration of inhaled anesthetics helps expedite the recovery process.
The usefulness of dexmedetomidine during the perioperative period continues to grow. Because of the hemodynamic stability that it offers, it is a useful adjunct in anesthesia.5,6
ResultsThe anesthetic drugs selected contributed to good hemodynamic stability, comfort on awakening, as well as analgesia and a lower use of the narcotic and the halogenated agent. The surgery lasted 2h and 45min. The dose of fentanyl and dexmedetomidine was adjusted in accordance with the hemodynamic parameters during anesthesia. The patient was transferred to the recovery room in a good state of alertness, and did not experience post-operative nausea or vomiting. Adjunct medications included a steroid (dexamethasone 16mg), ondansetron, gastric protector and analgesic (lysine clonyxinate 200mg).
ConclusionAt present, anesthesia for orthognathic surgery requires a combination of different anesthetic techniques to ensure that the patient is reassured, safe, comfortable and well covered for post-operative analgesia. Aside from the anesthetic and surgical risk, these procedures entail added challenges such as having to share the airway with the surgeon, having to access the airway through the nasopharyngeal approach in most cases, and patients transferred to the PACU with a swollen upper airway and, on occasions, with a partially restricted airway because of the use of interdental wiring. Hypotension, the most important side effect associated with the use of α-2 agonist dexmedetomidine might be beneficial for the procedure. Moreover, dexmedetomidine, aside from potentiating analgesia, provides post-operative sedation but does not change protective reflexes or wakeability. This clinical case shows that anesthetic conditions were optimal for the patient, and that it is possible to perform orthognathic surgery under the pharmcokinetic profile of dexmedetomidine.
Source of fundingThe researchers’ own resources.
Conflict of interestThe authors completed and published this clinical case for purposes of academic use and there are no particular conflicts of interest.
The authors are grateful to the participants in the study, all the physicians and the research team of IMSS UMAE C.M.N. “La Raza” for their commitment to this project.
Please cite this article as: García Méndez N, et al. Consideraciones anestesicas para cirugia ortognatica: reporte de un caso clinico. Rev Colomb Anestesiol. 2013;41:69–74.