This is a patient with post-partum hemorrhage (PPH), secondary to uterine atony managed with sub-lingual misoprostol 1000μg. Hyperpyrexia resulting from the route of administration of the drug and the clinical presentation of the condition, give rise to diagnostic difficulties and special interventions during the management process. A literature review on misoprostol, its pharmacological profile and side effects concluded that sub-lingual misoprostol results in a maximum concentration and is associated with the highest incidence of side effects as compared to other routes of administration.
Se presenta el caso de una paciente con hemorragia posparto (HPP) secundaria a atonía uterina, tratada con misoprostol 1.000μg por vía sublingual, y el curso de su evolución, en la que la hiperpirexia como efecto secundario por la vía de administración elegida, y la presentación clínica, generan dificultad diagnóstica e intervenciones especiales dentro del proceso de manejo. Se realiza una revisión de la literatura acerca del misoprostol, sus perfiles farmacocinéticos y sus efectos secundarios. Se concluye que el misoprostol, administrado por vía sublingual, procura la concentración máxima más alta y se asocia con la incidencia más alta de efectos secundarios en comparación con otras vías.
In 2003 the International Federation of Gynecology and Obstetrics (IFGO) classified PPH as a top priority condition worldwide and suggested the implementation of strategies for prevention, early diagnosis and timely treatment.3
In 2005 the World Health Organization (WHO) statistics reported maternal mortality complications associated to pregnancy, childbirth and the puerperium of up to 450×100,000 life births in developed countries and 9×100,000 born alive in developing countries.3 National statistics indicate that for 2006 in Colombia, obstetric hemorrhage was the second cause of maternal death after hypertensive disorders typical of pregnancy.5
Both FIGO and WHO recommend active labor for all women. The first therapeutic option for the management of uterine atony is the administration of uterotonics (oxytocin), in addition to volume replacement (crystalloids or blood byproducts); the second line of treatment is prostaglandins. In the absence of response, the next step is surgery: B-Lynch technique, ligation of uterine arteries and hysterectomy.4,6Temperature control mechanisms make a difference in the pathophysiological processes like fever and hyperthermia; in both fever and hyperpyrexia (>41°C to 105.8°F) these mechanisms are maintained through the elevation of the temperature set point in the hypothalamus and heat production exceeds the body's heat loss.1
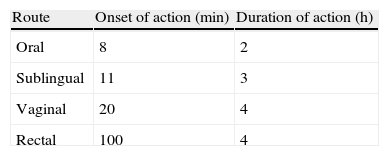
Misoprostol is a prostaglandin E1 synthetic analog, with uterotonic and cervix maturation effects; it is safe, stable at room temperature, with few side effects, affordable and economic; however, unsupervised use of misoprostol may lead to complications and teratogenicity. The clinical applications of misoprostol include medical abortion, cervix maturation, induction of labor and postpartum hemorrhage. Misoprostol may be administered orally, vaginally, sublingually or rectally. Its pharmaceutical profile depending on the route of administration is as follows (Table 1).2
A study in Ecuador evaluating 163 women receiving sublingual misoprostol for the management of PPH showed side effects associated with the route of administration, evidencing body temperatures above 40°C but the trial was unable to explain the pathophysiological mechanism of this association. Similar studies in other populations have not shown any similar behavior results.1
Materials and methodsA bibliographic search was undertaken in MEDLINE/PubMed, Lilacs, Scielo, Ovid, Elsevier, and Cochrane, using the terms “hyperpyrexia due to misoprostol”, “sublingual misoprostol”, “PPH”. The search included review articles, case series and case reports published between 2000 and 2010.
Case reportA 30-year-old patient, G3P1C0A1V1, with 40 weeks of gestation was admitted to the emergency room in active labor. The patient had a history of migraine, normal prenatal controls and no other co-morbidities or established risk factors. In her first visit the patient's vital signs were: HR 80bpm, RR 16rpm, BP 110/70mmHg, in latent phase of labor, hospitalized for labor care, progresses free of complications to eutocic vaginal delivery. In the immediate post-birthing, the patient presents profuse endouterine genital bleeding, of approximately de 800cc; the red code is activated and active uterotonic (oxytocin) management is established, volume resuscitation with crystalloids and 1000mg of sublingual misoprostol, with sound bleeding control and hemodynamic stabilization. After 1h with this management approach, the patient presents with fever (41°C), hypotension (BP 70/40mmHg), and tachycardia (HR: 200bpm), blood sugar 120mg/dl; electrocardiogram: supraventricular tachycardia followed by sensory disorders (disorientation). The initial diagnosis considered was reactivation of postpartum hemorrhage and the patient undergoes revision of the birth canal with no evidence of active losses; intravenous hydration is continued and antipyretic but the patient remains unresponsive with persistent 40°C temperature. Empirical antibiotic therapy (Clindamycin and gentamycin) was administered; suddenly the patient presents an episode of tonic movements with loss of consciousness and the decision was to do orotracheal intubation to protect the airway. Other probable diagnoses were side reaction to misoprostol vs. amniotic fluid embolism because of the obvious systemic involvement; the patient is then transferred to the intensive care unit. Paraclinical examination: blood test, renal function, coagulation tests and liver profile were normal; arterial gasses with metabolic acidemia; uneventful electrocardiogram; normal electrolytes and normal plain brain CT-scan.
The patient evolves to hemodynamic stability with progressive consciousness recovery without inotropic support or vasopressants, adequate progressive weaning from ventilation until spontaneous breathing is achieved and normalization of the acid–base balance. After 24h of the initial process, the patient was extubated with normal puerperium evolution, maintaining hemodynamic stability and no signs of systemic inflammatory response, ruling out the initial diagnoses and concluding that it was a case of idiosyncratic reaction to sublingual misoprostol. The patient was discharged on day three with no complications.
DiscussionMisoprostol is a safe drug but its toxic dose has not yet been established. However, we do know that the lethal dose in animals is up to 1000-fold of the so-called therapeutic doses in human beings. Nonetheless, it is important to understand the pharmacokinetic properties of the various routes of administration to choose the best regime based on the desired clinical application.2
No clinically significant adverse events have been found with misoprostol. Diarrhea is the main adverse reaction reported, usually mild and self-limiting; there can also be nausea and vomiting that resolve in 2–6h. Acknowledging the hyperexia associated with its administration is vital since any diagnostic delay results in higher mortality.
Sublingual misoprostol gives the maximum highest concentration and hence is associated with a higher incidence of side effects, consistent with the relationship suggested by the absorption kinetics of these two elements. Sublingual misoprostol has the shortest time to achieve maximum concentration following its administration, which makes it very useful when a fast-acting clinical response is needed, such as in the case of PPH. This is by no means the only advantageous route of administration; for instance, the vaginal route provides high bioavailability and a constant plasma level making it the preferred route when a longer duration of clinical effects is required.2
Misoprostol studies for the prevention of PPH have reported: chills in 32–57% of the cases, hyperpyrexia (41°C) following the administration of 600μg, and hyperpyrexia with delirium and/or ICU admission following the oral administration of 800μg.
Temperature elevations associated with the use of misoprostol are compatible with the hypothalamic adjustment. E2 prostaglandins (PGE2) have been involved in the pathophysiological mechanism of endogenous fever and identified as the major mediator for inducing fever because of its interaction with the Prostaglandin E3 (EP3) receptor. There is no evidence that prostaglandin E1, acts differently from PGE2. In sum, misoprostol-induced fever mimics the PGE2 endogenous thermoregulation patterns, changing the hypothalamic adjustment in its upper segment and stimulating temperature elevation. However, pharmacological studies are required to validate this hypothesis.1
During pregnancy, the increased rate of puerperal fever following misoprostol administration may be the result of a lower threshold of prostaglandins that induce temperature elevation. In contrast, pre-clinical studies suggest that pregnancy suppresses fever due to an increased endogenous production of antipyretics and decreased endogenous output of pyrogens.1
Despite the uncertain link between prostaglandins, pregnancy and fever, it has been known that endogenous prostaglandins play an important role in the pathophysiological processes involved with labor, membrane rupture, cervical maturation, myometrial contractility, delivery and uterine involution.
Other misoprostol use-related effects are: uterine rupture, infection (low incidence: 0.92%); in early pregnancy: congenital defects and although mutagenesis studies with misoprostol have been negative, no embryotoxic, fetotoxic or teratogenic effects have been shown.2
ConclusionsProstaglandins are the second line of pharmacological treatment in PPH. Misoprostol, a synthetic prostaglandin E1 analog, may be administered orally, vaginally, sublingually or through the rectum. It is safe and well tolerated, while no clinically significant adverse effects have been identified. In misoprostol trials for the prevention of PPH, hyperpyrexia (41°C) has been reported following the administration of 600μg, and hyperpyrexia with delirium and/or ICU admission following the oral administration of 800μg. As compared to other routes of administration, the higher maximum concentration of the sublingual administration has been associated with a higher incidence of side effects.
FundingAuthors’ resources.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez Pacheco FH, Zambrano Benítez CP. Reporte de caso y revisión de la literatura: hiperpirexia como efecto secundario posterior a la administración de misoprostol por vía sublingual en el manejo de la hemorragia posparto. Rev Colomb Anestesiol. 2013;41:65–8.